Deep venous thrombosis with azygos continuation of inferior vena cava
Presentation
Three days non-specific back pain, bilateral leg pain with swelling. Bilateral compartment syndrome on examination with associated rhabdomyolysis and acute kidney injury requiring hemofiltration.
Patient Data
CT Abdomen and pelvis
Distension and non-enhancement along the infrarenal IVC, common iliacs, external iliacs and femoral veins. Thrombus extension into right renal vein. As an anatomical variant, hepatic segment of IVC is absent and IVC continues into azygos venous system; hepatic veins join and drain directly into right atrium. Mild perivascular fat stranding is observed along thrombosed vessels. Remainder exam is unremarkable.
Renal Doppler ultrasound
The right kidney measured 10.1 cm in length. Small 12 mm parapelvic cysts noted within the lower pole. The right renal vein was patent with no thrombus appreciated within.
The left kidney measured 10.4 cm in length. The left renal vein was extremely difficult to visualize. It is unclear whether this is secondary to left renal vein thrombus or due to patient body habitus limiting visualization of the vessel. The IVC inferior to the renal vein entry demonstrated thrombus however the superior extent of this thrombus was not able to be appreciated. Flow is demonstrated within the suprarenal IVC although the caliber of the patent portion of the vessel at this point is narrowed.
Conclusion:
No thrombus identified within the right renal vein. It is not possible on this study alone to comment on whether thrombus is present within the left renal vein secondary to the technically challenging nature of the scan.
Thrombus is present within the IVC inferior to the renal vein entry, although the superior extent of this thrombus was not able to be delineated. Thin stream of flow was visualized within the IVC superior to the renal vein entry.
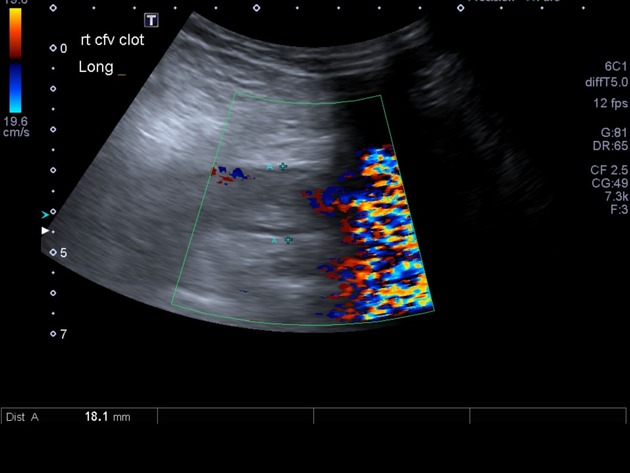
Lower limbs venous Doppler US
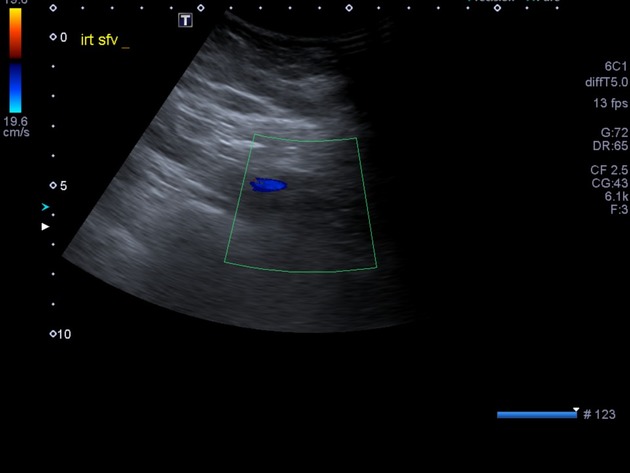
Targeted study of above knee veins in ICU. Extensive occlusive thrombus extends from the common iliac veins to at least the popliteal veins bilaterally.
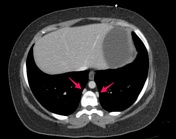


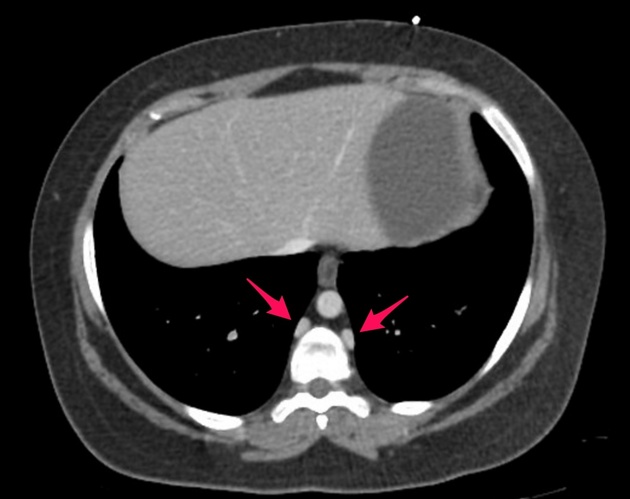
Annotated images depicting transition of thrombosed IVC into azygos (yellow circle) and upper images of thorax showing the azygos and hemiazygos veins (pink arrows). On the ultrasound selected image, the left common femoral vein is delineated by yellow dashed circular line, with an hypoechogenic content and non-compressible.
Case Discussion
Inferior vena cava (IVC) abnormalities are recognized as risk factors for spontaneous deep venous thrombosis in young patients 1. Hepatic segment anomalies of the IVC are thought to occur when the right subcardinal veins fail to merge with the hepatic sinusoids during embryological development. This results in bypassing from the supracardinal anastomosis through the retrocrural azygos vein 1. Azygos continuation of the IVC is a recognized variant and this results in visceral and lower extremity blood returning to the right atrium via the azygos system 2. This interrupted IVC may cause increased blood pressure in the lower extremity veins in the presence of insufficient collaterals. Subsequently, venous stasis develops which predisposes to deep venous thrombosis 2,3.
In this case, the diagnosis was made via CT which was performed to rule out a pulmonary embolism and other differentials to explain the presentation including arterial thromboembolism, malignancy and renal infarction. The significant venous obstruction resulted in obstruction of venous drainage from both lower limbs resulting in bilateral lower limb compartment syndrome. On arrival to intensive care, the patient had progressed to septic shock with anuric renal failure requiring renal replacement therapy. Bilateral fasciotomies would not have relieved the compartment syndrome given that the primary pathology was venous drainage. Catheter-directed thrombolysis and bilateral venous bypass were felt to be of minimal benefit in this scenario. The patient subsequently passed away from overwhelming septic shock with multiorgan dysfunction.
Deep venous thrombosis in young patients with no known prothrombotic states should warrant further investigation for associated venous anomalies that can be delineated through CT 1.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.