BACK MENU NEXT
Mystery cases
Case credits: Matt Skalski
Video presentation
|
Key Points
-
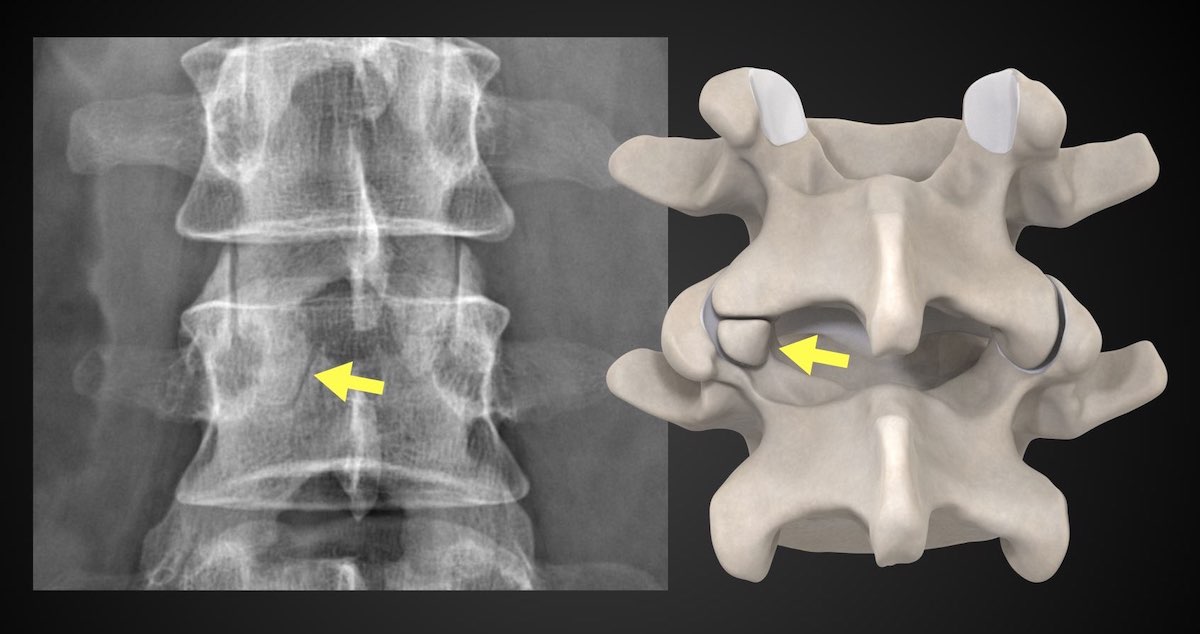
Oppenheimer ossicle
- articular process secondary ossification center that is un-united
- often incidental, if sclerosis/osteophytes then could potentially be symptomatic
- Barbie was better than Oppenheimer (author opinion)
-
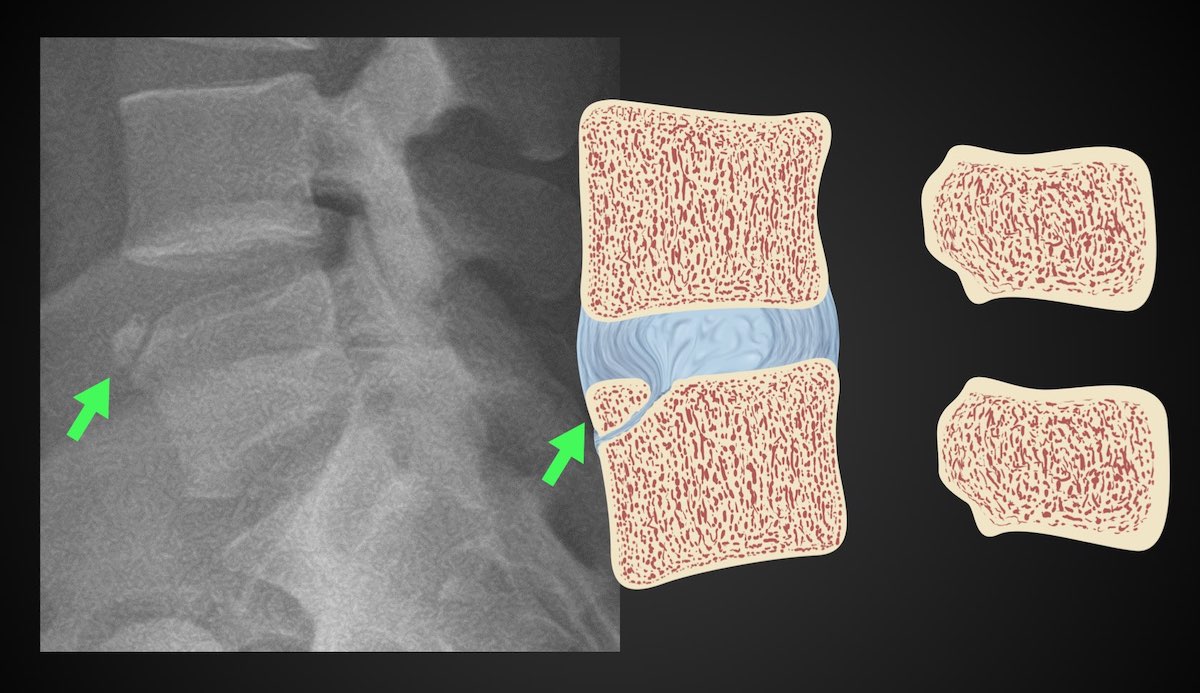
limbus bone
- small corner of ring apophysis un-united
- corticated margin and so shouldn't be confused for acute fracture
-
intercalary bone
- area of disc annulus ossification/calcification
- occurs on background of degenerative disc
-
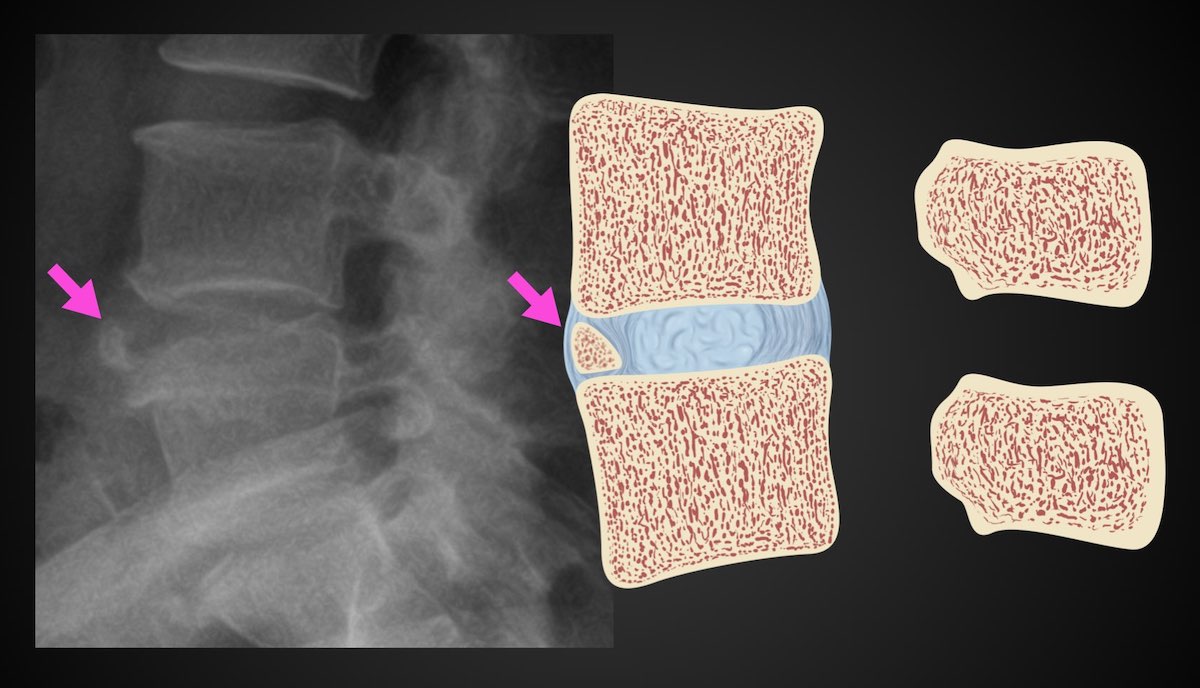
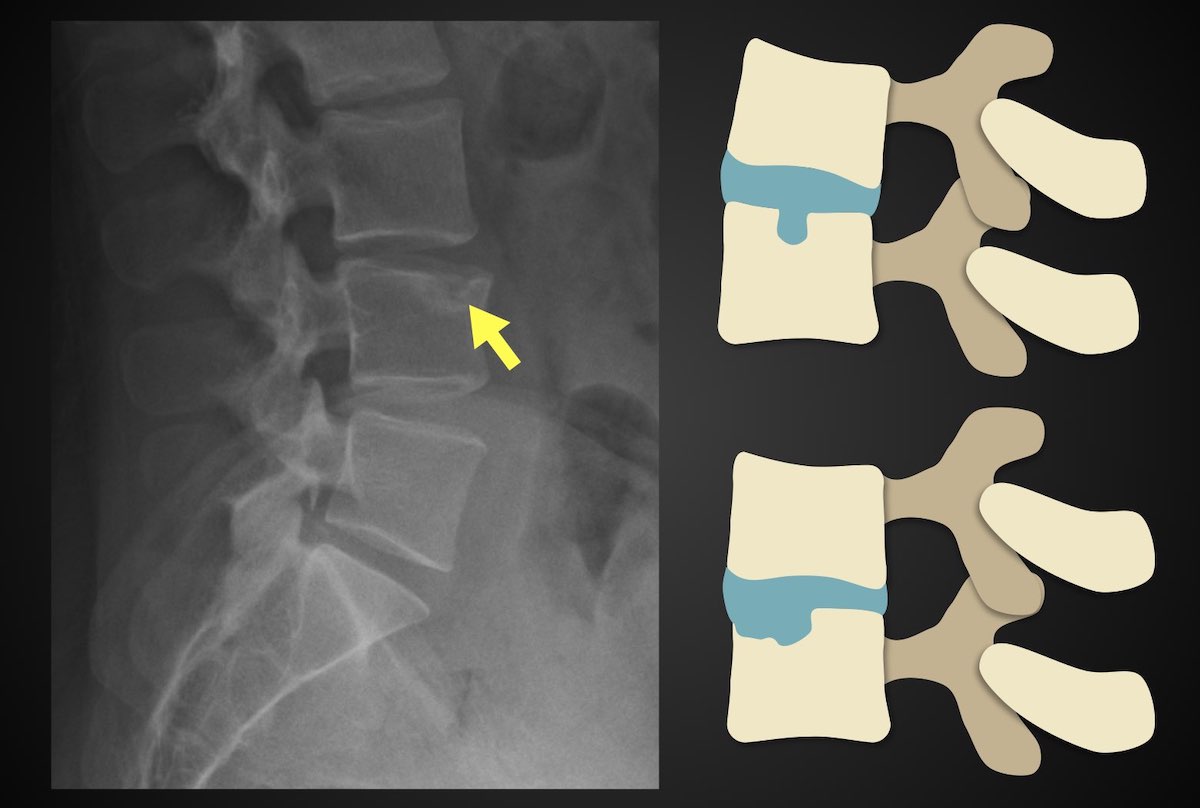
Schmorl node
- intravertebral disc herniation through the endplate
- often multiple, can be "giant"
- may be symptomatic when acute (edema on MRI)
-
prominent nuclear impression
- normal curved impression upon the endplate due to the nucleus
|
SKIP TO NEXT PAGE
Oppenheimer ossicle
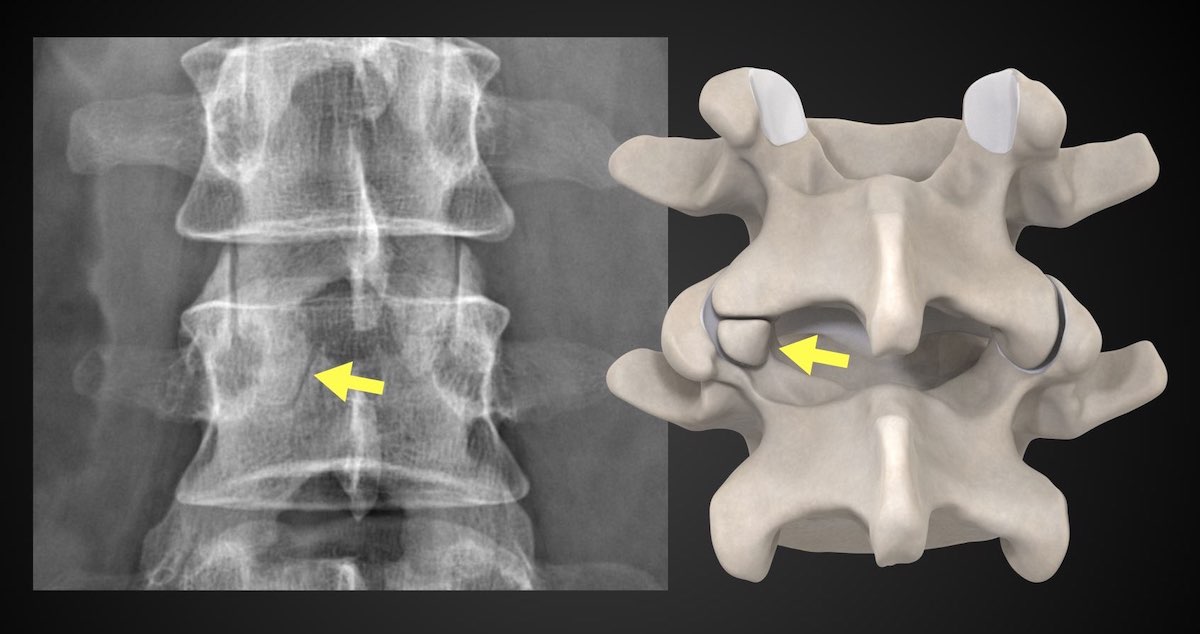
Illustration: Matt Skalski
Oppenheimer ossicles are accessory ossicles associated with the facet joints and are found in ~4% (range 1-7%) of lumbar spines 1.
Oppenheimer ossicles predominantly occur as a single, unilateral ossicle of the inferior articular processes of the lumbar spine although they can also occur at the superior articular process ref.
Best seen on sagittal CT and MR images and can be easily mistaken on thick axial slices.
Oppenheimer ossicles are seen in the lumbar spine, most notably at L2 and L3 levels 2. They appear as smoothly corticated structures that may sometimes be lined by articular cartilage. The synovial space of the adjacent facet joint may communicate with the cleft between the ossicle and the articular process 2.
They may be associated with other vertebral arch malformations, such as articular process hypoplasia 2.
Oppenheimer ossicles are thought to arise as a result of the non-union of an articular process secondary ossification center. These ossicles should fuse between the ages of 17 and 25 years ref.
History and etymology
Oppenheimer nodules were first described by Albert Oppenheimer in 1942 3.
usually asymptomatic and discovered incidentally on imaging 2.
not to be confused with an articular process fracture: an Oppenheimer ossicle will demonstrate regular, well-defined corticated margins
From article: Oppenheimer ossicle
Limbus vertebra
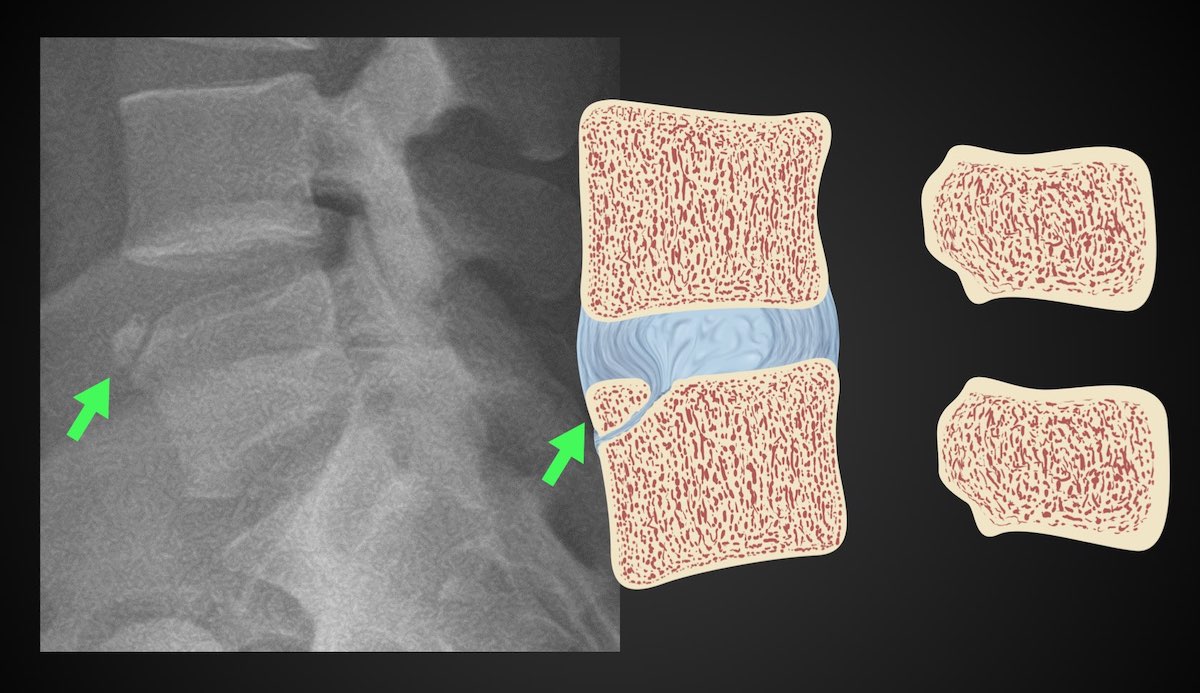
Illustration: Matt Skalski
A limbus vertebra is a well-corticated unfused secondary ossification center of the vertebral body, usually of its anterosuperior corner, that occurs secondary to herniation of the nucleus pulposus through the vertebral body endplate beneath the ring apophysis (see ossification of the vertebrae). These are closely related to Schmorl nodes and should not be confused with limbus fractures or infection.
Their formation occurs before the age of 18 years, but often they are seen in older adults.
Anterior limbus vertebrae are generally asymptomatic and are detected incidentally. Posterior limbus vertebrae are far less common but have been reported to cause nerve compression.
The features of a limbus vertebra are the same on x-rays, CT and MRI.
It should:
Unlike a fracture, in a limbus vertebra, the 'fragment' of bone will not 'fit' into the adjacent vertebral body defect but rather will usually appear to be too small.
A limbus vertebra is usually encountered in the mid-lumbar spine, although occasionally it may be seen in the thoracic spine. The anterosuperior corner of a single vertebral body in the mid-lumbar spine is the most common presentation. The anteroinferior and posteroinferior corners are seen far less frequently 1.
Discography
Radiography with or without CT or MRI is sufficient for diagnosis. Historically, the diagnosis was confirmed with discography where contrast could be seen extending into the intraosseous herniation of the nucleus pulposus 1.
History and etymology
The term limbus is a direct borrowing from the Latin word meaning fringe, as in the edge of something, or hem 3. Interestingly, limbus vertebra was first described by Schmorl in 1927 4.
Consider
intercalary bone: ossification is in the anterior annular fibers of an intervertebral disc
-
acute fractures: should have an adjacent perivertebral hematoma
degenerative disease of the spine
infection: adjacent cortical loss and soft tissue mass
From article: Limbus vertebra
Intercalary bone
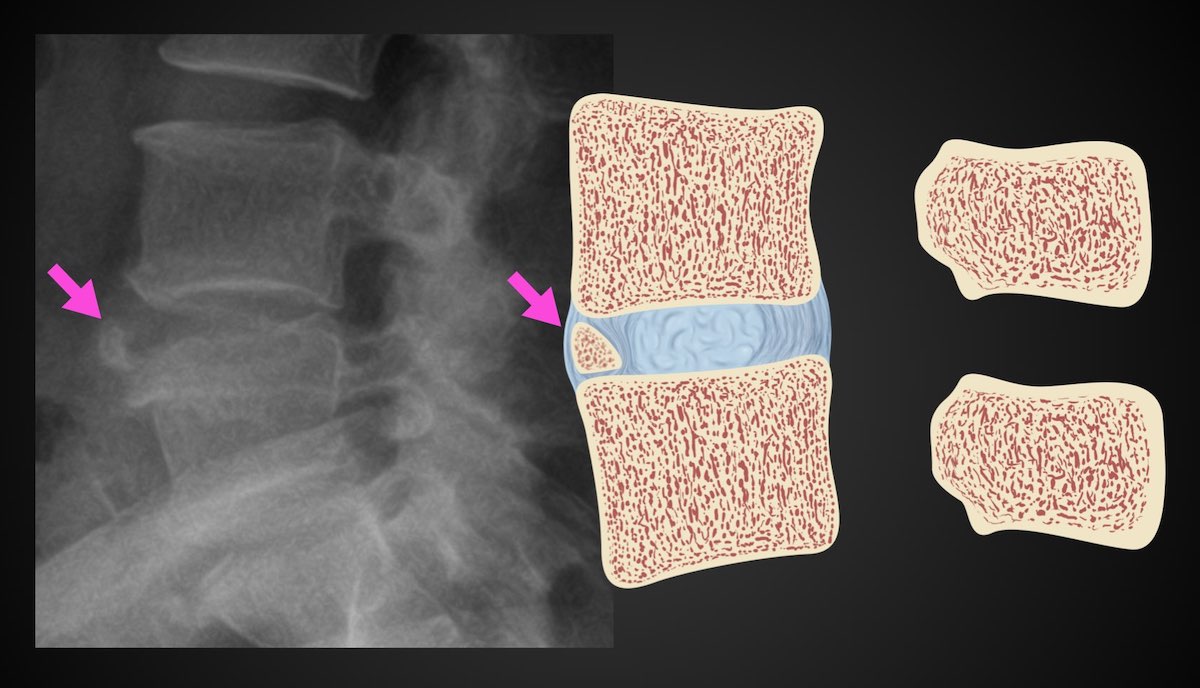
Illustration: Matt Skalski
Intercalary bones are common discal ossifications that are usually triangular in morphology, found in the anterior annular fibers of an intervertebral disc, and are thought to be degenerative in etiology.
From article: Intercalary bone
Schmorl nodes
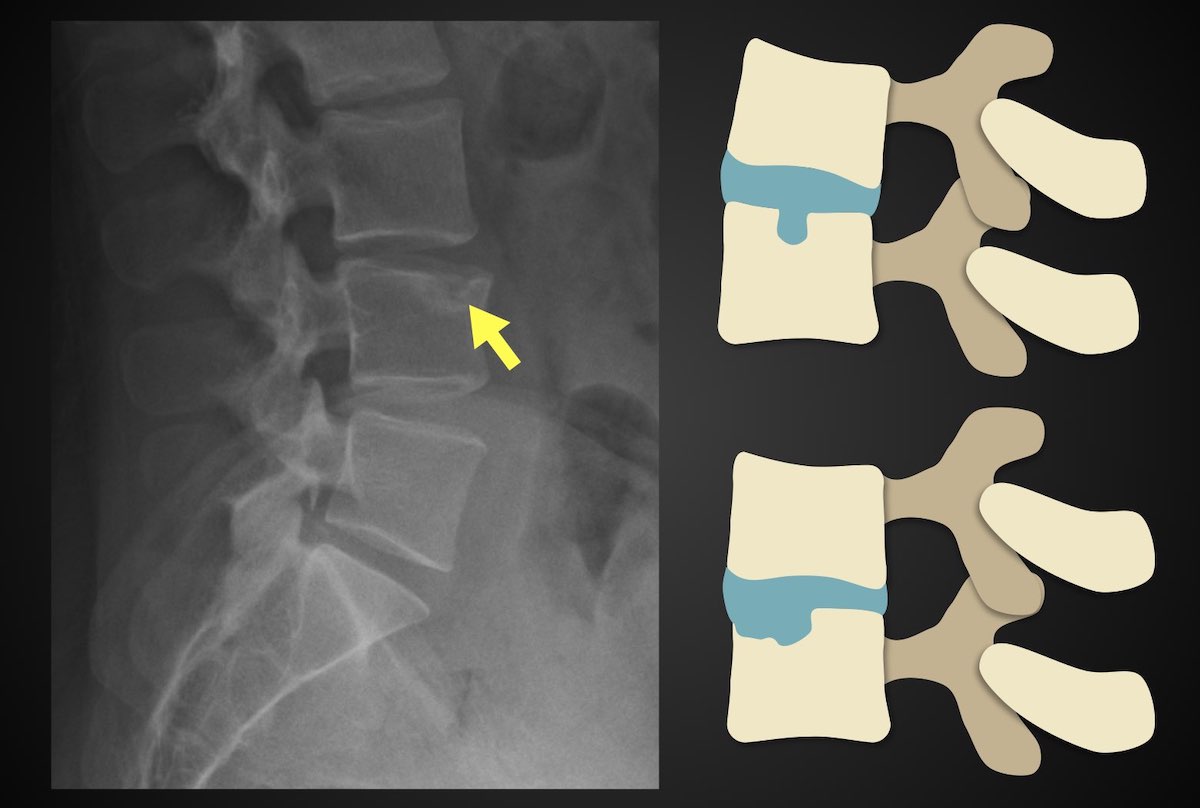
Illustration: Matt Skalski
Schmorl nodes, also known as intravertebral disc herniations, refer to protrusions of the cartilage of the intervertebral disc through the vertebral body endplate and into the adjacent vertebra. The protrusions may contact the marrow of the vertebra, leading to inflammation.
Quiescent Schmorl nodes are extremely common found in around 75% of autopsies, at all ages, more frequently in males 9.
Chronic Schmorl nodes are usually asymptomatic, and their etiological significance for back pain is controversial. Acute Schmorl nodes, in contrast, are uncommon and are associated with inflammation and symptoms 9.
Schmorl nodes are among the diagnostic criteria of Scheuermann disease 6. A limbus vertebra is closely related to a Schmorl node as well.
It is believed that Schmorl nodes develop following back trauma, although this is incompletely understood. Nucleus pulposus pressure on the weakest part of the endplate or vertebral development process during early life may be a possible explanation 7.
In the acute stage, Schmorl nodes can be difficult to diagnose on plain radiography or detect due to sclerosis around the margin of the herniation not having had time to develop.
Plain radiograph
Usually, they are small nodular lucent lesions involving the inferior endplate of lower thoracic and lumbar vertebral bodies. However, the involvement of both the inferior and the superior endplates is not uncommon. A sclerotic margin may be present.
CT
Schmorl nodes are better identified on CT images, showing the same pattern observed on radiographs.
MRI
Schmorl nodes are best seen on the sagittal sequences and usually exhibit the same signal characteristics as the adjacent disc, with a thin rim of sclerosis at the margins.
Acute herniation can appear more aggressive with surrounding bone marrow edema and peripheral enhancement 9. The gas extrusion sign may be present which refers to hypointensity in the intervertebral disc space across all pulse sequences 10. These acute features evolve gradually over months but may take over a year 9,10.
Nuclear medicine
FDG-PET
Acute Schmorl nodes have been reported to be FDG-PET avid 9.
History and etymology
It is named after Christian Georg Schmorl (1861-1932), a German pathologist who first described them in 1927 9.
For chronic Schmorl nodes, there are few differentials as they have characteristic appearances.
For acute Schmorl nodes consider:
spondylodiscitis: compared with infection, acute Schmorl nodes will have more focal endplate changes, no fever, and no epidural or prevertebral phlegmonous changes 10
malignancy 9
From article: Schmorl nodes
Report problemMENUNEXT




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.