Acetabular dysplasia is referred to as a shallow acetabulum, not being able to provide sufficient coverage for the femoral head and thus leading to instability of the hip joint.
On this page:
Terminology
Acetabular dysplasia is a form of developmental dysplasia of the hip (DDH) often referred to in the adolescent and adult population 1.
Epidemiology
Adult hip dysplasia has an estimated prevalence of 0.1% and is more common in women 2,3. Male sex is apparently associated with posterosuperior deficiency 3.
Associations
Acetabular dysplasia is associated with the following conditions 2,3:
infantile developmental dysplasia of the hip
excessive femoral anteversion
femoroacetabular impingement morphology in ~50%: more commonly cam than pincer morphology 12,13
Risk factors
Risk factors for acetabular dysplasia include the following 2,3:
previous septic arthritis
previous trauma
Clinical presentation
The clinical presentation of acetabular dysplasia has been described as variable 11. Patients can present with hip pain or groin pain especially with extreme positions e.g. high hip flexion and hyperextension. In addition, there may be limping or signs and symptoms of hip instability 11. Clinical signs include a positive hip impingement test 11 and/or anterior apprehension test.
Complications
25-50% of patients with acetabular dysplasia will develop early hip osteoarthritis if left untreated 1-6.
Other complications include2-4:
hip instability
Pathology
Acetabular dysplasia is characterized by a smaller weight-bearing surface than the normal acetabulum, which ultimately leads to increased contact stress and static overload due to under-coverage of the femoral head and structural instability. This adds to cartilage and/or labral injury as well as damage to the joint capsule 2-4.
Etiology
Acetabular dysplasia might be the result of abnormal growth after treatment or missed developmental dysplasia of the hip during childhood, the etiology of which is multi-factorial in nature. It may be also due to other hip pathologies that have occurred during childhood as septic arthritis, trauma or Legg-Calve-Perthes disease ref.
Subtypes
Acetabular dysplasia can be divided into different patterns concerning 3-D morphology. One grading scheme subdivides the acetabular dysplasia into the following patterns with lateral acetabular deficiency being constantly present 3:
global acetabular deficiency
anterosuperior acetabular deficiency
posterosuperior acetabular deficiency
Other schemes differentiate anterior, posterior and global or lateral deficiencies 2.
Radiographic features
Radiographic assessment of acetabular dysplasia or adult hip dysplasia includes plain radiographs of the pelvis and additional planes as the false profile view of Lequesne, cross-table lateral or frog-leg lateral views.
Cross-sectional imaging is advised for better three-dimensional characterization, preoperative planning 3 and the detection of chondral and labral lesions.
Plain radiograph
The most common measurement in acetabular dysplasia is the lateral center-edge angle on a plain anterior-posterior radiograph of the pelvis 2,4. Patients should be in the supine position with both legs in 15° of internal rotation to maximize femoral neck length 2. A value of ≤25° is considered abnormal or borderline and a value of ≤20° is an indicator for dysplasia 2,4,5. The cut-off should be also adapted to the measurement and whether the lateral bony acetabular rim or the lateral edge of the acetabular sourcil was taken to measure the lateral center-edge angle 7.
Further measurements to confirm insufficient acetabular coverage are the following 2,4,5:
acetabular angle (less commonly used 14)
medial center edge angle
acetabular arc
the anterior center-edge angle of Lequesne (assessed on false profile view – moderate reproducibility)
femoral head-neck-shaft angle (to assess for coxa valga and surgical planning)
CT
The main role of CT is improved characterization of the three-dimensional acetabular morphology in a setting of preoperative planning. It should also comprise the assessment for excessive acetabular anteversion or acetabular retroversion. Other than the crossover sign on the anterior-posterior view of the pelvis, CT can also differentiate posterior under-coverage in the setting of acetabular dysplasia from anterior overcoverage in the setting of pincer morphology or plain acetabular retroversion and it can better assess the grade of posterior deficiency than the posterior wall sign 3.
CT measurements for the assessment of acetabular dysplasia include the following and are conducted one cut above the greater trochanters 2:
anterior acetabular sector angle: a value of ≤50° indicates dysplasia
posterior acetabular sector angle: a value of ≤90° indicates dysplasia
horizontal acetabular sector angle: a value of ≤140° indicates dysplasia
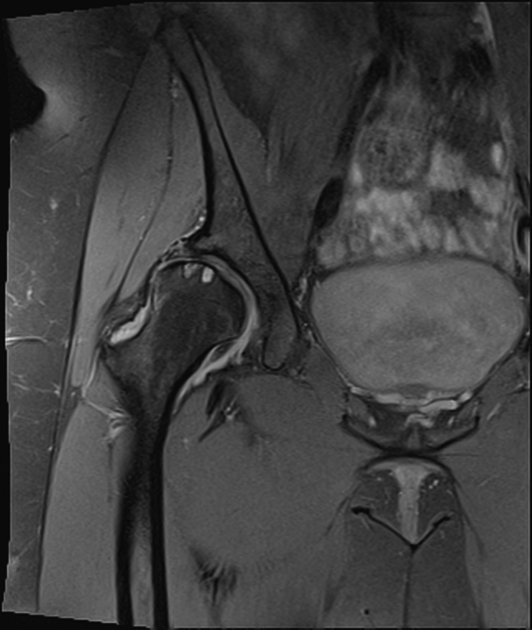
MRI
In addition to the three-dimensional assessment of the acetabular and femoral morphology, which highly benefits from 3D imaging in this situation, MRI allows for assessment of concomitant labral, chondral or ligamentum teres injury as well as the evaluation of the joint capsule 1.
Radiology report
The radiological report should include the description of the following 2,3:
acetabular morphology
measurements: e.g. lateral center-edge angle, acetabular index and/or extrusion index
signs of early osteoarthritis: subchondral sclerosis, cysts, osteophytes and Tonnis grade
labral and/or chondral injury or ligamentum teres injury
fovea alta (if present)
Treatment and prognosis
Treatment options of acetabular dysplasia include in particular periacetabular osteotomy 1,6 and other acetabular osteotomies (e.g. Salter) which reorient the acetabulum in a fashion that provides better coverage for the femoral head. Another surgical option is acetabuloplasty, which alters the morphology of the acetabulum (e.g. Pemberton) 6,8. Periacetabular osteotomy is in particular indicated in patients with a preserved range of motion.
Salvage osteotomies (e.g. Chiari or shelf osteotomy) do not preserve articular cartilage and can be considered if the hip needs to be stabilized in incongruous joints 8.
In the case of a severely arthritic hip, joint replacement surgery might be considered and include total hip replacement and resurfacing arthroplasty 2.
The role of conservative management is limited due to the early progression to osteoarthritis and should decrease pain and can be chosen in very mild dysplasia with mild symptoms. Non-operative treatment includes weight loss, activity and lifestyle modifications as well as nonsteroidal anti-inflammatory drugs, specialized physical therapy intra-articular injections ref.
Treatment complications
Operative complications include the following:
femoroacetabular impingement in case of overcorrection 2,9
Differential diagnosis
other forms of hip impingement








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.