Adrenal hemorrhage can result from a variety of traumatic and non-traumatic causes. When unilateral, it is often clinically silent. In contrast, bilateral adrenal hemorrhage can lead to catastrophic adrenal insufficiency.
On this page:
Clinical presentation
The clinical signs of adrenal hemorrhage are very non-specific, but can include abdominal pain and secondary signs of significant blood loss such as hypotension or tachycardia 4.
The large majority of patients with unilateral adrenal hemorrhage do not have clinically obvious signs of adrenal insufficiency and the diagnosis is usually made incidentally at imaging performed for another reason.
Bilateral hemorrhage often results in an adrenal crisis, with coma and death resulting if steroid replacement therapy is not administered promptly. Despite treatment, overall there is approximately a 15% mortality, and about 50% when in the setting of sepsis.
Pathology
Adrenal hemorrhage can be either unilateral or bilateral. Adrenal gland trauma is a common cause of unilateral adrenal hemorrhage. On the other hand, bilateral adrenal hemorrhage is rarely due to trauma and is frequently attributed to adrenal vein spasm or thrombosis. Predisposing risk factors include:
- sepsis, especially meningococcaemia (also known as Waterhouse-Friderichsen syndrome)
- disseminated intravascular coagulation (DIC)
- primary antiphospholipid syndrome
- heparin-induced thrombocytopenia
- steroid usage
- anticoagulation
- underlying adrenal tumor
- in neonates (birth trauma, sepsis, hypoxia, adrenal insufficiency, hemorrhagic disorders and diabetic mothers) 7,8
- adrenal vein thrombosis
Adrenal hematoma can be seen in the setting of recent ipsilateral nephrectomy in about 5% of cases 11.
Radiographic features
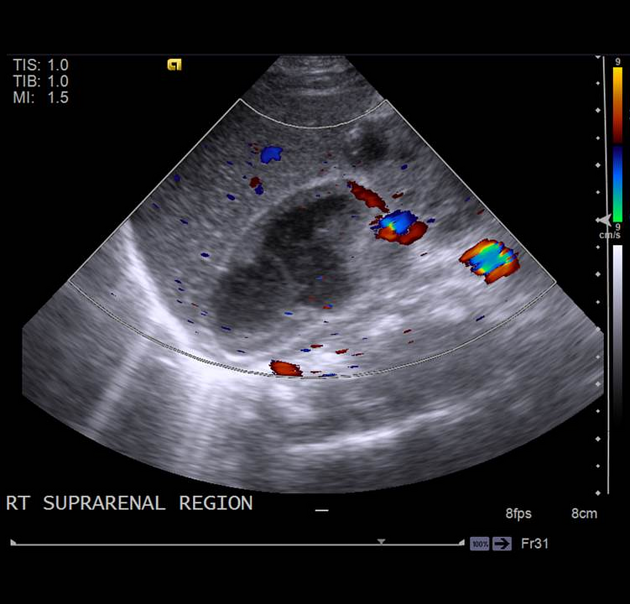
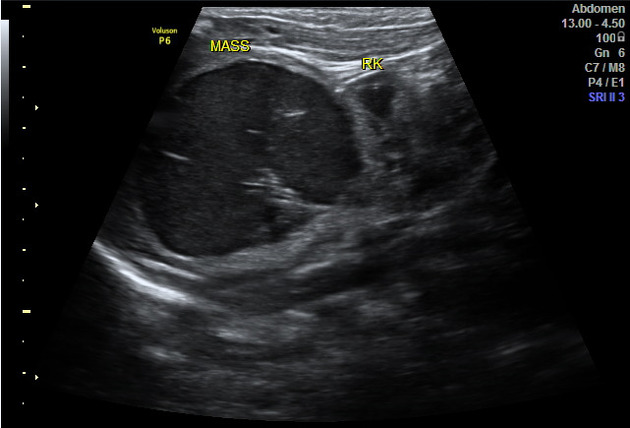
Ultrasound
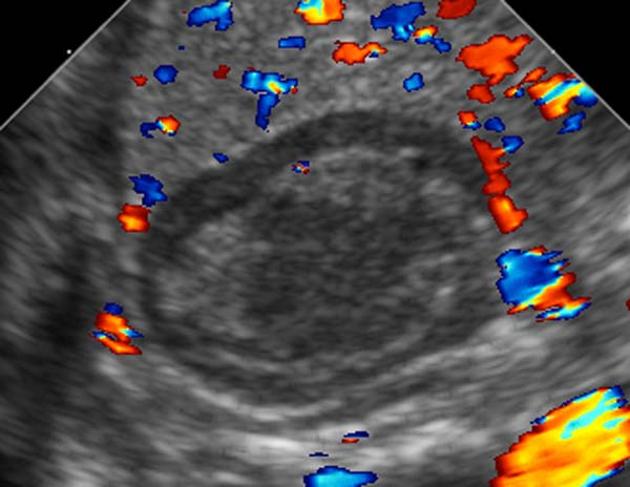
The pattern of echogenicity of an adrenal hematoma depends on its age:
- an early-stage hematoma appears solid with diffuse or inhomogeneous echogenicity
- as liquefaction occurs, the mass demonstrates mixed echogenicity with a central hypoechoic region and eventually becomes completely anechoic and cyst-like
- calcification may be seen in the walls of the hematoma as early as 1-2 weeks after onset and gradually compact as the blood is absorbed
Color Doppler and power Doppler imaging confirm that the mass is avascular.
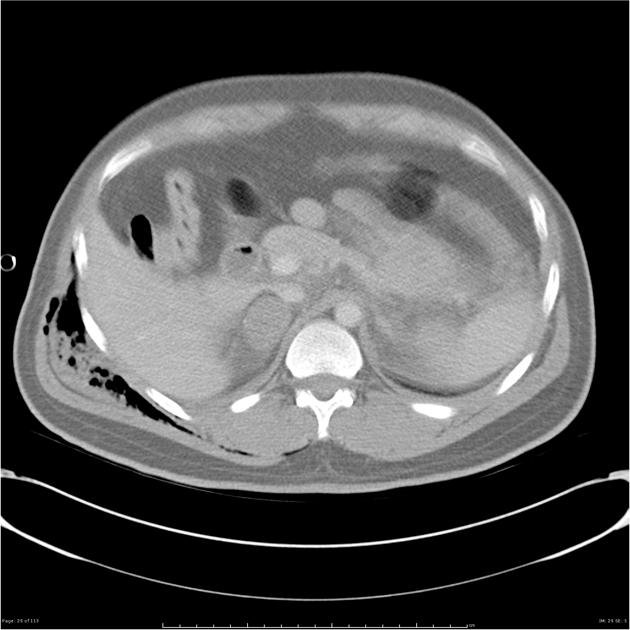
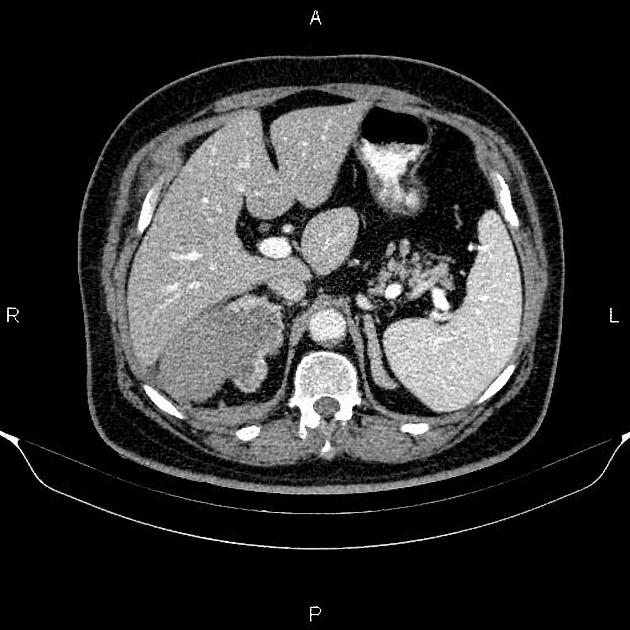
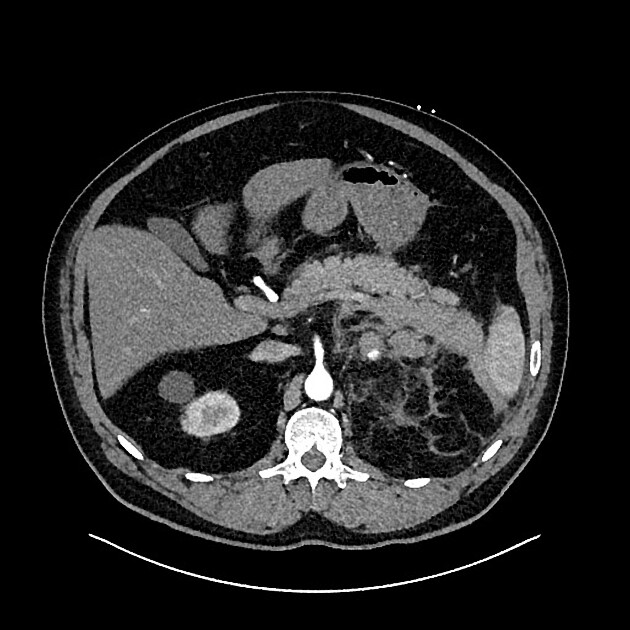
CT
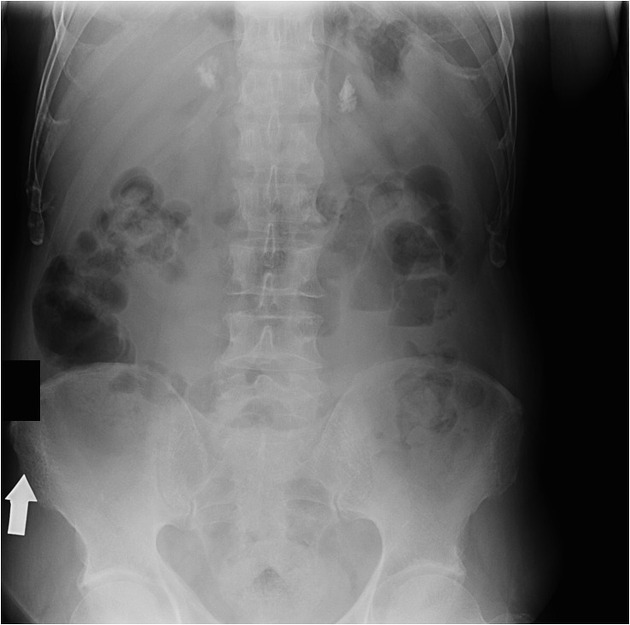
Adrenal hematomas characteristically appear round or oval, often with surrounding stranding of the periadrenal fat.
The attenuation value of an adrenal hematoma depends on its age:
- acute to subacute hematomas contain areas of high attenuation that usually range from 50-90 HU
- adrenal hematomas decrease in size and attenuation over time, and most resolve completely
- organized chronic adrenal hematoma appears as a mass with a hypoattenuating center, with or without calcifications (also known as adrenal pseudocysts)
- adrenal hematomas may calcify after one year
Of note, adrenal congestion, described as adrenal thickening and peri-adrenal stranding, has been reported to precede adrenal hemorrhage 10, although more research is needed to understand this process.
MRI
- acute stage (<7 days after onset): the hematoma typically appears isointense or slightly hypointense on T1 weighted images and markedly hypointense on T2 weighted images
- subacute stage (7 days to 7 weeks after onset): the hematoma appears hyperintense on T1 and T2 weighted images
- chronic stage (typically >7 weeks after onset): a hypointense rim is present on T1 and T2 weighted images, which is attributed to hemosiderin deposition and the presence of a fibrous capsule
Differential diagnosis
- in neonates
-
neuroblastoma
- liver metastasis
- vascularity
-
congenital adrenal hyperplasia
- bilateral
- glands are enlarged and have a cerebriform contour
-
neuroblastoma
- in adults
- if only limited images of the upper abdomen are available, it may be difficult to differentiate a rim-calcified hematoma from a splenic artery aneurysm






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.