Autoimmune encephalitis, also known as autoimmune limbic encephalitis, is an antibody-mediated brain inflammatory process. While typically involving the limbic system, any part of the brain or central nervous system more broadly, can be involved.
Autoimmune encephalitis can be divided broadly into two groups, based on whether or not antibodies are the result of an underlying tumour:
paraneoplastic encephalitis: usually antibodies are against intracellular antigens, poor response to immunotherapy
non-neoplastic autoimmune encephalitis: antibodies are against extracellular antigens, usually with a reversible neuronal dysfunction and better response to immunotherapy
On this page:
Terminology
Unfortunately, there is considerable heterogeneity in how the term limbic encephalitis is used. Most authors limit the term to autoimmune limbic encephalitis, including both paraneoplastic and non-paraneoplastic causes. Some, however, include viral encephalitides (especially HSV encephalitis) under the broad term limbic encephalitis.
For the purpose of this article, we will restrict the term to autoimmune encephalitis, both paraneoplastic and non-paraneoplastic causes. HSV and other viral encephalitides are discussed separately.
Epidemiology
The epidemiology of tumour-related autoimmune encephalitis mimics that of the underlying malignancy. Those with non-tumour related autoimmune encephalitis have a variable epidemiology. Overall, the most common encephalitis with antibodies to intracellular antigens is anti-Hu encephalitis 7, whilst the most common encephalitis with antibodies to cell surface antigens is anti-LGI1 encephalitis 43,44. Some autoimmune encephalitides have a sex and age predilection, for example, anti-NMDA encephalitis is more common in young females, while anti-LGI1 and anti-CASPR2 encephalitides are more common in older males 44.
Associations
Various autoimmune encephalitides may be associated with an underlying malignancy or tumour, more commonly in those with antibodies against intracellular antigens 21.
Clinical presentation
The clinical presentation of autoimmune encephalitis is incredibly varied, with potential manifestations including subacute development of 2,8:
seizures and epilepsy, including new-onset refractory status epilepticus (NORSE)
mental status change
-
psychiatric symptoms (e.g. psychosis, depression and behaviour disorder)
the presence of psychiatric symptoms is particularly helpful in distinguishing limbic encephalitis from herpetic encephalitis, which otherwise can present similarly, albeit usually more acutely 8
memory disturbance
focal neurological deficits (e.g. cerebellar dysfunction, signs localising to the brainstem)
movement disorders
sleep disorders
Additionally, patients may have other neurological clinical features not directly attributable to encephalitis alone, such as syndromes of the peripheral nervous system.
Pathology
Autoimmune encephalitis can be divided according to the presence or absence of an underlying tumour, or on the type of antibody responsible.
Associated tumours
Causes of paraneoplastic autoimmune encephalitis include 8,9:
small cell lung cancer (classic cause): e.g. anti-Hu antibodies
testicular germ cell tumours: e.g. anti-Ma antibodies
ovarian tumours (e.g. ovarian carcinoma and ovarian teratoma)
haematological malignancies (e.g. Hodgkin lymphoma)
gastrointestinal malignancies
Causes of non-paraneoplastic autoimmune encephalitis include:
specific antibodies (see below)
systemic autoimmune conditions, e.g. systemic lupus erythematosus (SLE)
Specific antibodies
An alternative way of dividing autoimmune encephalitis is on the grounds of whether the antibodies are against intracellular antigens or cell surface antigens 21. The antibodies, in turn, correlate both to an underlying cause and pattern of involvement 8,9. As a general rule, antibodies targeted to intracellular antigens are more frequently associated with an underlying tumour 9.
-
group I - antibodies to intracellular antigens
-
anti-Hu (ANNA-1) antibodies 21
most common encephalitis with antibodies to intracellular antigens 7
associated with small cell lung cancer (in 75% of cases)
presents with encephalomyelitis, subacute sensory neuronopathy, or cerebellar degeneration
-
anti-Ma (Ta) antibodies 21
associated with small cell lung cancer (anti-Ma1), testicular tumours (anti-Ma2)
presents with limbic encephalitis, rhombencephalitis, or cerebellar degeneration
better prognosis than anti-Hu encephalitis
-
anti-CRMP-5 (collapsin response-mediator protein-5) (CV2) antibodies 21,34,35
associated with small cell lung cancer and malignant thymoma
involvement of the striatum prominent
presents with encephalomyelitis, cerebellar degeneration, choreiform movement disorders, peripheral neuropathy, or optic neuropathy (see anti-CRMP-5 optic neuropathy)
-
anti-GAD65 (glutamic acid decarboxylase 65) antibodies 21
rarely associated with tumours, may also be associated with type 1 diabetes mellitus
presents with stiff person syndrome, limbic encephalitis, or cerebellar ataxia
-
anti-amphiphysin antibodies 21
associated with small cell lung cancer, breast cancer
presents with stiff person syndrome or limbic encephalitis
-
anti-Ri (ANNA-2) antibodies 21
associated with small cell lung cancer, breast cancer
presents with opsoclonus-myoclonus syndrome, encephalomyelitis, or cerebellar ataxia
-
anti-Yo (PCA-1) antibodies 21
associated with ovarian cancer, breast cancer
presents with cerebellar degeneration
-
anti-Tr (DNER) antibodies 21
associated with Hodgkin lymphoma
presents with cerebellar degeneration
-
anti-Zic4 antibodies 14
associated with small cell lung cancer
presents with cerebellar degeneration
-
anti-KLHL11 (Kelch-like protein 11) antibodies 13,21,32
associated with testicular tumours, ovarian cancer
presents with rhombencephalitis, brachial amyotrophic diplegia
-
anti-LUZP4 (leucine zipper 4) antibodies 32,33
associated with testicular tumours
presents with rhombencephalitis, brachial amyotrophic diplegia
often co-exists with anti-Ma2 and/or anti-KLH11 antibodies
-
anti-SOX1 (Sry-like high mobility group box 1) antibodies 21
associated with small cell lung cancer
presents with cerebellar degeneration
-
anti-ANNA-3 antibodies 21
associated with small cell lung cancer
presents with limbic encephalitis, encephalomyelitis, or cerebellar degeneration
-
anti-PCA-2 (Purkinje cell cytoplasmic antibody type 2) (MAP1B) antibodies 24
associated with small cell lung cancer
presents with cerebellar ataxia, limbic encephalitis, or neuropathy
-
anti-Homer-3 antibodies 23
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia
-
anti-GFAP (glial fibrillary acid protein) antibodies (autoimmune GFAP astrocytopathy) 15
usually not associated with tumours, but ovarian teratoma is most common
broad clinical phenotype including meningoencephalitis or meningoencephalomyelitis
-
anti-neurochondrin antibodies 25,26
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia, rhombencephalitis, chorea, neuropathy, or myelitis
-
anti-ITPR-1 (inositol trisphosphate receptor 1) antibodies 25,27
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia or neuropathy
-
anti-ARHGAP26 (RhoGTPase-activating protein 26) antibodies 25,28
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia or psychosis
-
anti-AP3B2 (adaptor protein-3 beta-2) antibodies 25,30
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia or neuropathy
-
anti-AK5 (adenylate kinase 5) antibodies 18,36
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with limbic encephalitis
-
anti-PDE10A (phosphodiesterase 10A) antibodies 36,37
very rare but may have an association with lung cancer
presents with chorea
-
anti-RGS8 (regulator of G-protein signalling 8) antibodies 36,38
very rare but may have an association with lymphoma
presents with cerebellar ataxia
-
anti-TRIM46 (tripartite motif-containing protein 46) antibodies 36,39
very rare but may have an association with small cell lung cancer
presents with cerebellar ataxia or encephalomyelitis
-
anti-TRIM9/67 (tripartite motif-containing proteins 9 and 67) antibodies 36,40
very rare but may have an association with non-small cell lung cancer
presents with cerebellar ataxia
-
anti-CAMKV (calmodulin kinase-like vesicle) antibodies 41
very rare but may have an association with uterine cancer
presents with limbic encephalitis or movement disorders
-
-
group II - antibodies to cell surface antigens
-
anti-NMDAR (N-methyl-D-aspartic acid receptor) antibodies 21
second most common encephalitis with antibodies to cell surface antigens 44
may be associated with underlying tumours (e.g. ovarian teratoma) in older patients, but younger patients may not have any underlying tumour
presents with psychiatric symptoms initially, followed by limbic encephalitis, movement disorders, and dysautonomia
mild or often absent imaging changes are common
-
anti-VGKC (voltage-gated potassium channel) antibodies 21
common
-
two types:
-
anti-LGI1 (leucine-rich-glioma-inactivated 1) antibodies 42
most common encephalitis with antibodies to cell surface antigens 43,44
usually not associated with underlying tumour or malignancy
presents with limbic encephalitis with often specific seizure types (e.g. faciobrachial dystonic seizures, autonomic seizures), hyponatraemia
-
anti-CASPR2 (contactin-associated protein 2) antibodies
may be associated with thymoma
presents with limbic encephalitis, Isaacs syndrome, Morvan syndrome
-
-
anti-GABA (gamma-aminobutyric acid) antibodies 21
-
two types:
-
anti-GABAA antibodies
usually not associated with underlying tumour or malignancy
presents with refractory epilepsy
-
anti-GABAB antibodies
may be associated with small cell lung cancer
presents with limbic encephalitis or opsoclonus-myoclonus syndrome
-
-
-
anti-AMPAR (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor) antibodies 21
may be associated with small cell lung cancer, breast cancer, thymoma
presents with limbic encephalitis
-
anti-D2R (dopamine-2 receptor) antibodies 21
usually not associated with underlying tumour or malignancy
presents with parkinsonsim (basal ganglia encephalitis)
-
anti-GlyR (glycine receptor) antibodies 21
usually not associated with underlying tumour or malignancy
presents with stiff person syndrome or progressive encephalomyelitis with rigidity and myoclonus (PERM)
-
anti-mGluR1 (metabotropic glutamate receptor 1) antibodies 21
may be associated with Hodgkin lymphoma
presents with cerebellar ataxia
-
anti-mGluR5 (metabotropic glutamate receptor 5) antibodies 21
may be associated with Hodgkin lymphoma
presents with limbic encephalitis (known as Ophelia syndrome in this setting)
-
anti-GluR3 (glutamate receptor 3) antibodies 22
associated with Rasmussen encephalitis
-
anti-DPPX (dipeptidyl-peptidase–like protein 6) antibodies 16,21
usually not associated with underlying tumour or malignancy
presents with encephalopathy with hyperekplexia, myoclonus, tremor; often has a prodrome of gastrointestinal upset and weight loss (similar syndrome to progressive encephalomyelitis with rigidity and myoclonus (PERM))
-
anti-IgLON5 (immunoglobulin LSAMP, OBCAM, neurotrimin 5) antibodies 17,21
usually not associated with underlying tumour or malignancy
presents with a broad phenotype including sleep disorder, bulbar dysfunction, and cognitive impairment
-
anti-VGCC (voltage-gated calcium channel) antibodies 21
may be associated with small cell lung cancer
presents with cerebellar ataxia and Lambert-Eaton myasthenic syndrome
-
anti-SEZ6L2 (seizure-related 6 homolog like 2) antibodies 19
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia
-
anti-neurexin-3-alpha antibodies 20
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with a clinical phenotype that may mimic anti-NMDAR encephalitis
-
anti-septin-5 antibodies 25,29
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with cerebellar ataxia
-
anti-septin-7 antibodies 31
very rare and unclear if there are any associations with underlying tumour or malignancy
presents with encephalopathy
-
Radiographic features
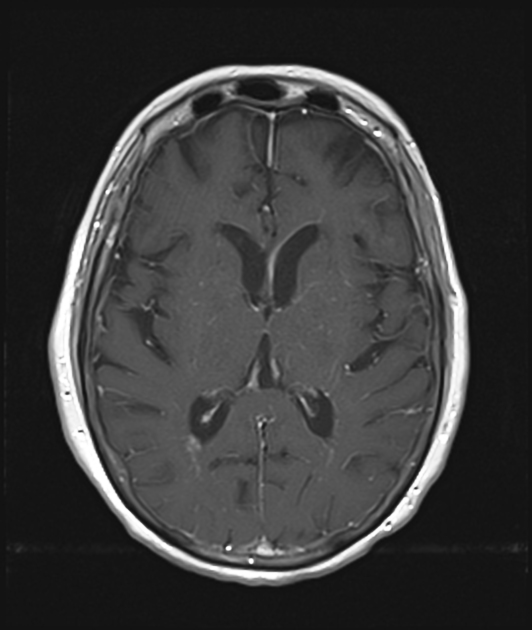
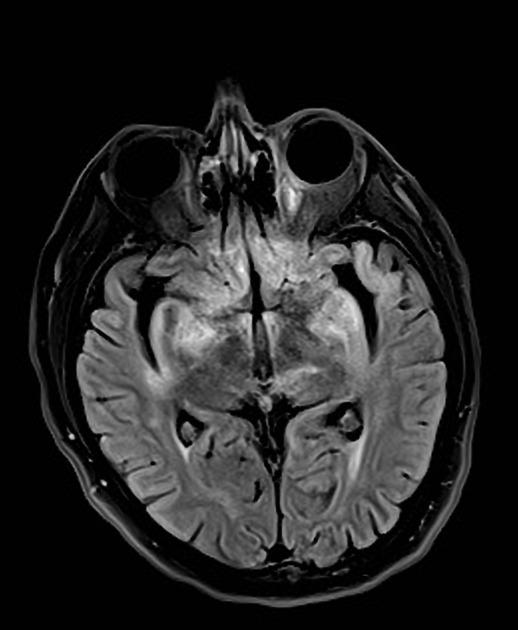
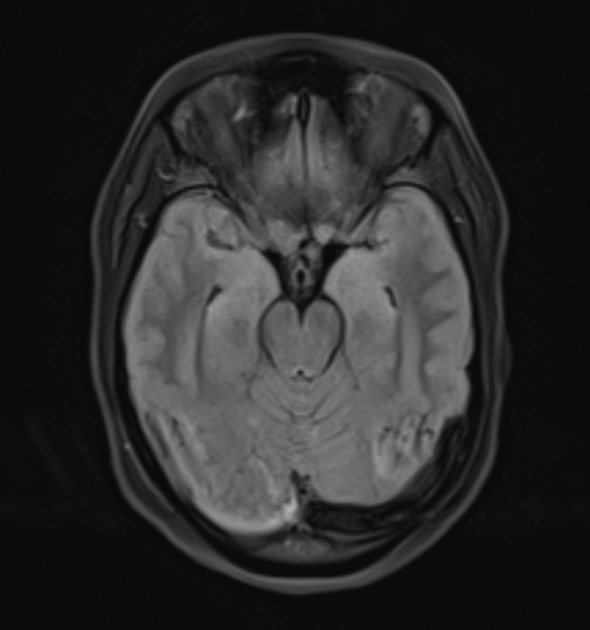
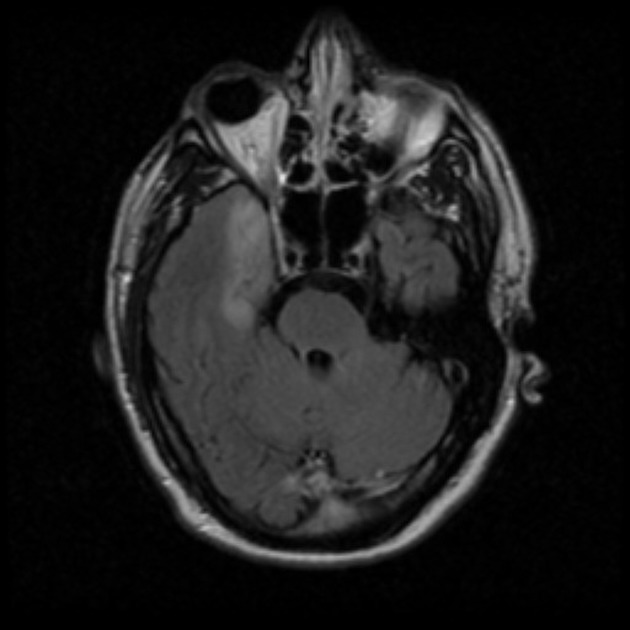
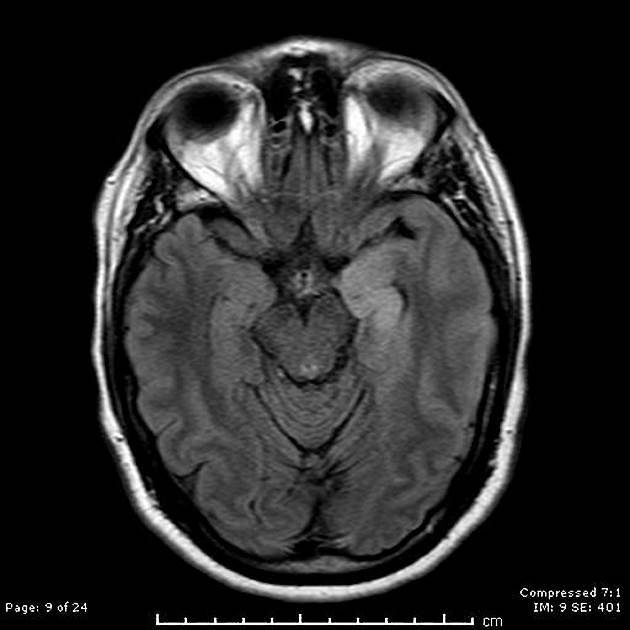
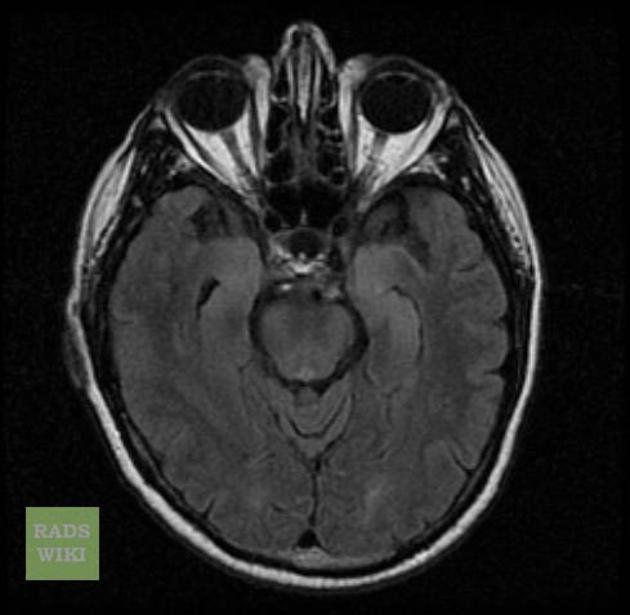
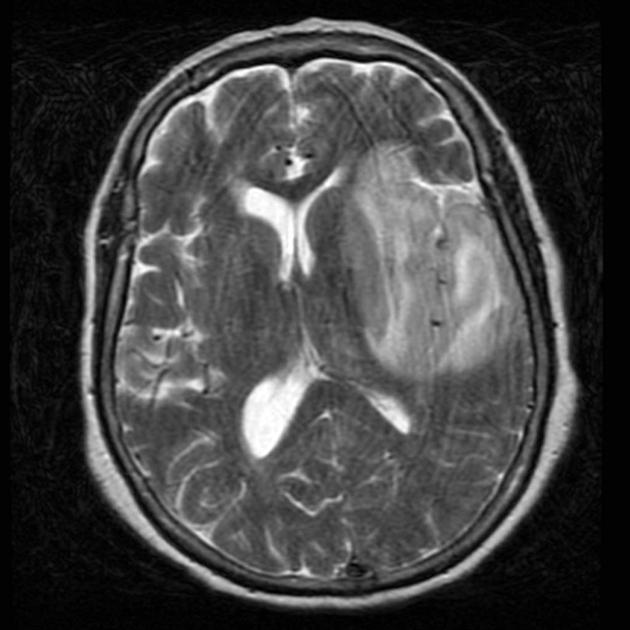
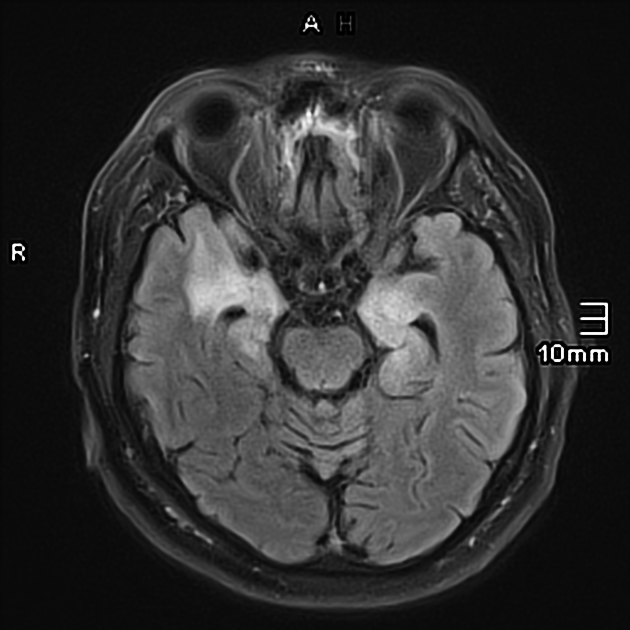
MRI
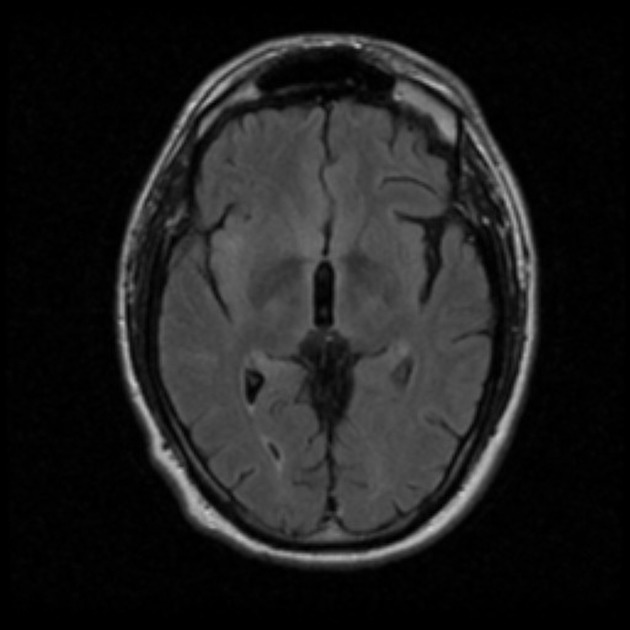
Many cases have no imaging findings, especially early in the course of the disease. However, MRI with contrast is considered the most sensitive imaging modality, and findings are present in over half of individuals 8.
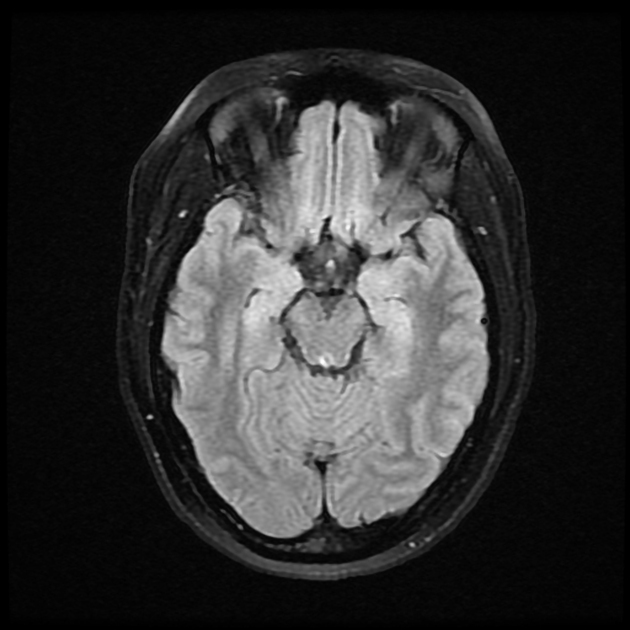
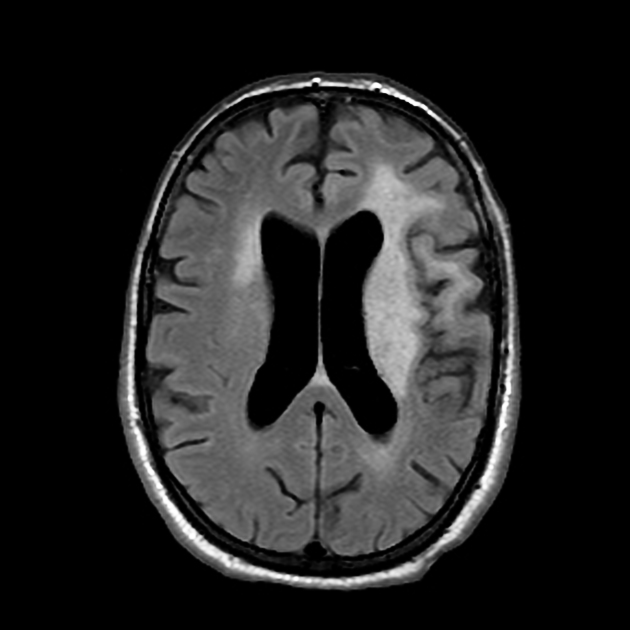
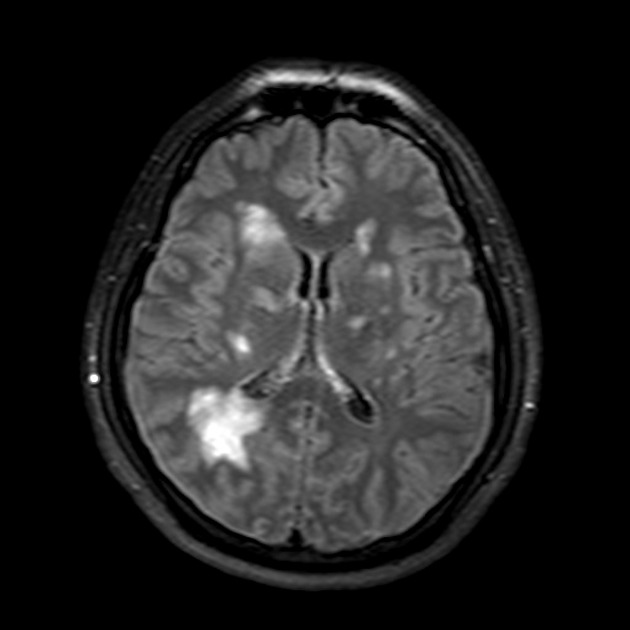
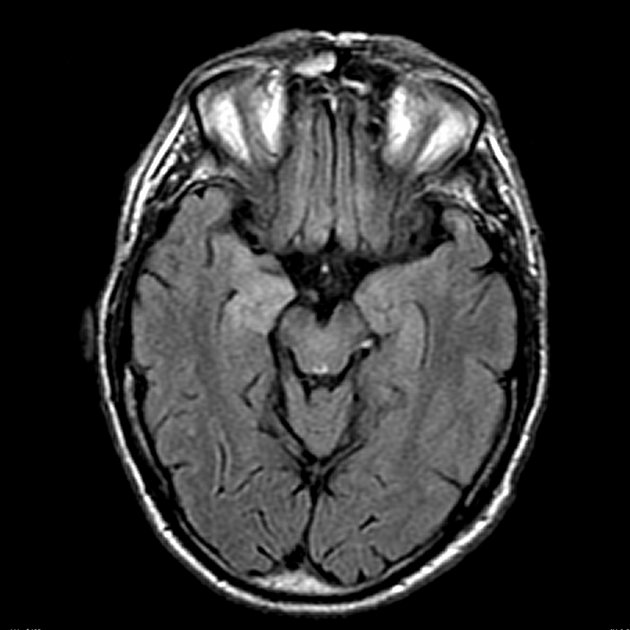
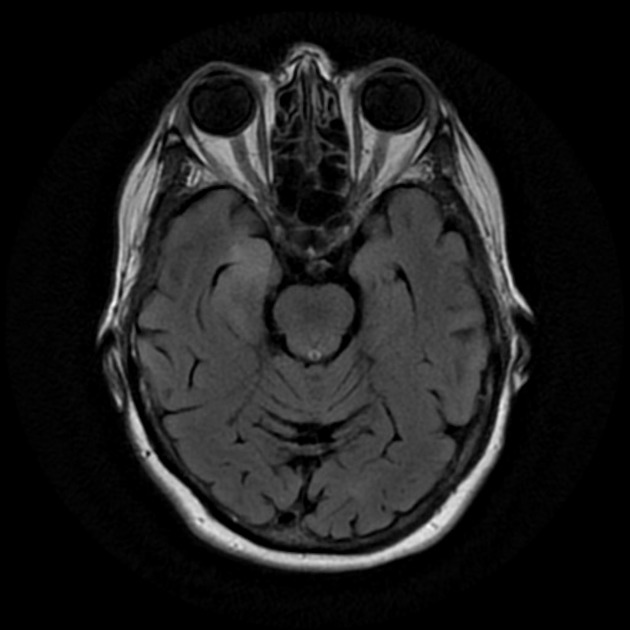
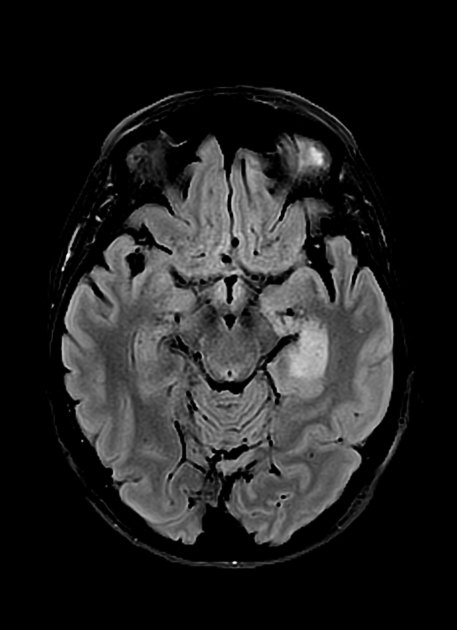
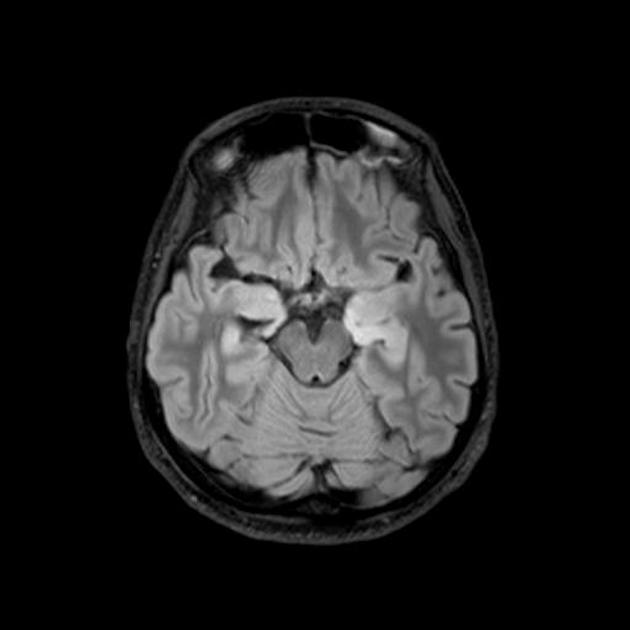
As the older term limbic encephalitis implies, the most common location of involvement is the mesial temporal lobes and limbic systems, typically manifested by cortical thickening and increased T2/FLAIR signal intensity of these regions. Bilateral involvement is most common (60%), although often asymmetric 8. The lateral temporal lobe and insula are less commonly involved, whereas the basal ganglia and thalami, in contrast, are frequently involved, helpful in distinguishing it from HSV encephalitis which characteristically spares the basal ganglia 8.
In addition to the aforementioned T2/FLAIR changes, patchy areas of enhancement can be seen post-gadolinium ref. True diffusion restriction (i.e. low ADC values) and haemorrhage are not common and suggest alternative diagnoses ref. The presence of haemorrhage on SWI, for example, favours other diagnoses such herpes simplex encephalitis.
Although less common, essentially any part of the central nervous system can be involved in autoimmune encephalitis 9. This is particularly important in autoimmune encephalitides which are not presenting with the classic limbic encephalitis phenotype.
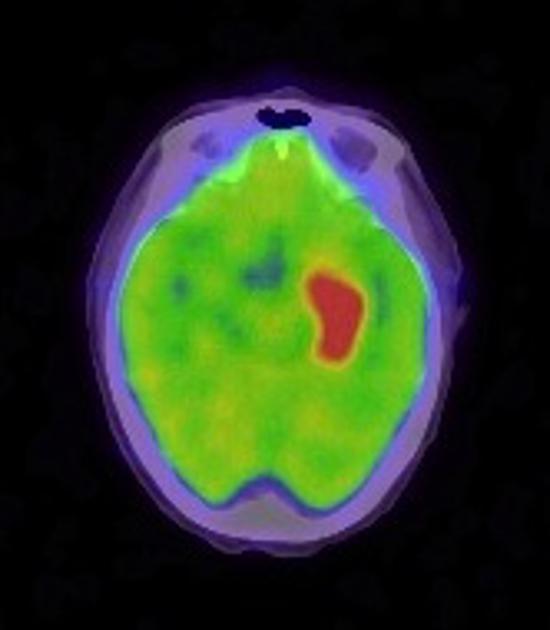
Nuclear medicine
PET-CT may show increased FDG uptake 4.
Treatment and prognosis
In patients with underlying malignancy, treatment of this underlying malignancy is important. Otherwise, management is predominantly with immunosuppression, with options including high-dose glucocorticoids, intravenous immunoglobulin, plasmapheresis, cyclophosphamide, and rituximab 11,12. Symptomatic management (e.g. of seizures with antiseizure medications) and neurological rehabilitation are also important aspects of therapy 11.
Differential diagnosis
General imaging differential considerations include:
-
acute, often dramatic time course
fever
psychiatric symptoms uncommon
basal ganglia spared
may have haemorrhage
-
acute, often dramatic time course
-
tumour
-
low-grade astrocytoma
if localised to the temporal lobe, appearances can be very similar
-
diffuse T2 hyperintensity involving multiple contiguous lobes
no predilection for the limbic system
-
-
Hashimoto encephalopathy (steroid-responsive encephalopathy associated with autoimmune thyroiditis)
sometimes considered to be a form of autoimmune encephalitis






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.