Buried bumper syndrome is a rare but important complication in patients with a percutaneous gastrostomy tube, occurring by migration of the internal bumper along its track. The tube may get lodged anywhere between the gastric wall and the skin and lead to life-threatening complications that may include hemorrhage, peritonitis, hollow viscus perforation, abscess formation, and necrosis.
On this page:
Epidemiology
The reported incidence is ~2% (range 0.3-4%) of patients. Most commonly seen as a late complication, it has been reported as early as 1 week after tube placement 4-5. Not surprisingly, the risk of buried bumper syndrome varies between various models/types.
Clinical presentation
Symptoms and signs may comprise:
simple PEG tube malfunction
leakage from peristomal areas
erythema and edema of the peristomal skin
abdominal pain
frank peritonitis
Patency of the tube does not rule out migration of the bumper; aspiration may only be limited initially with complete blockage being a late symptom 10.
Pathology
The most accepted theory is that of high-grade tension between the external and internal plate, leading to necrosis of the gastric wall and allowing for wandering of the bumper along its track, where it can get lodged anywhere. The development of an epithelial-covered channel may prevent overt tube malfunction and/or visualization of contrast leak by fluoroscopy (see below).
Important factors
Many risk factors have been identified, including
obesity: single most important factor 2
reduced space between external bumper and skin
rapid weight gain
frequent manipulation of the tube in the early post-insertion period
frequent patient and tube manipulation, possibly by inexperienced personnel
gauze placement beneath external bumper
chronic cough
Complications
Complications range from malfunction to malnutrition, bleeding, peritonitis, abscess formation, necrosis including necrotizing soft-tissue infection and eventually death 3.
Radiographic features
Although the most sensitive test is considered to be endoscopy, allowing for both the diagnosis and possible treatment, also imaging studies play a pivotal role both in suggesting the diagnosis and depicting the degree of this potentially fatal complication.
Fluoroscopy
Although upper gastrointestinal studies may suggest pneumoperitoneum and/or contrast leak from the tube, there have been examples where they failed in diagnosing the entity, possibly attributable to the development of an epithelisied channel.
Ultrasound
May allow for assessing the location of the internal bumper and depict local or peritoneal collections.
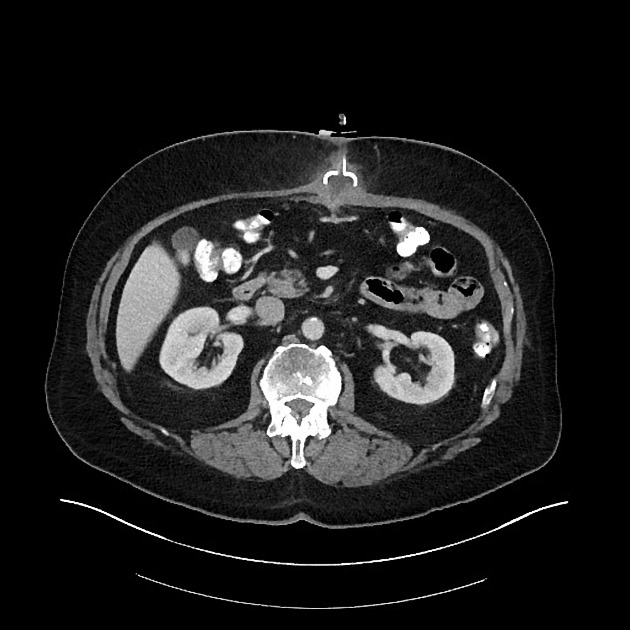
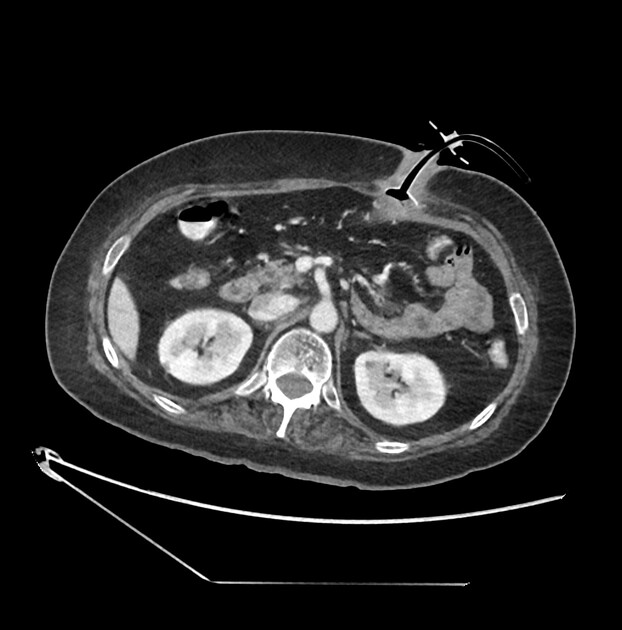
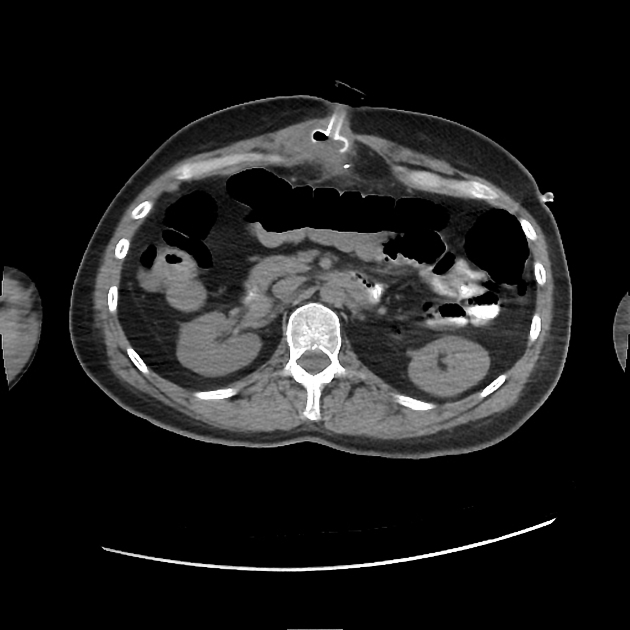
CT
Allows for accurate assessment of both the internal bumper's location and potential additional findings 7.
Treatment and prognosis
Initially considered a surgical emergency, treatment choices now largely depend on patient state and range broadly. Surgery, endoscopic removal/replacement, local incision followed by replacement using the existing track or a new track, dependent on inflammatory changes 6.
Practical points
maintaining a high level of clinical suspicion of this potentially life-threatening complication may be life-saving
cross-sectional imaging should be pursued/offered readily by the radiologist, possibly even as first-line imaging 7




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.