Cellulitis (rare plural: cellulitides) is an acute infection of the dermis and subcutaneous tissues without deep fascial or muscular involvement. It results in pain, erythema, edema, and warmth. Since the epidermis is not involved, cellulitis is not transmitted by person-to-person contact.
On this page:
Epidemiology
Risk factors
HIV/AIDS
Clinical presentation
Cellulitis can affect any region of the body, and commonly affects a lower limb. Clinical presentations include skin erythema without a well-defined border, increased skin temperature, swelling of the affected area, and regional lymphadenopathy and lymphangitis. Systemic features such as fever and rigors may also be present.
Complications
If the infection spreads to deeper tissues, complications can occur, such as soft-tissue abscess, necrotizing fasciitis, infectious myositis, and/or osteomyelitis. Occasionally sepsis may result. Special consideration should be given to geriatric patients, in whom cellulitis of the lower extremities is more likely to develop into thrombophlebitis.
Pathology
Cellulitis occurs after disruption of the skin and invasion of the subcutaneous tissues by microorganisms that may be skin flora, such as beta-hemolytic streptococci (most often), Staphylococcus aureus (including methycillin-resistant), or other bacteria 9. Patients with peripheral vascular disease or diabetes mellitus are particularly susceptible to cellulitis of the lower limbs; the compounding effect of minor (often unnoticed) injuries and poor vascular supply leads to skin breakdown that can be a point of entry for microorganisms.
Radiographic features
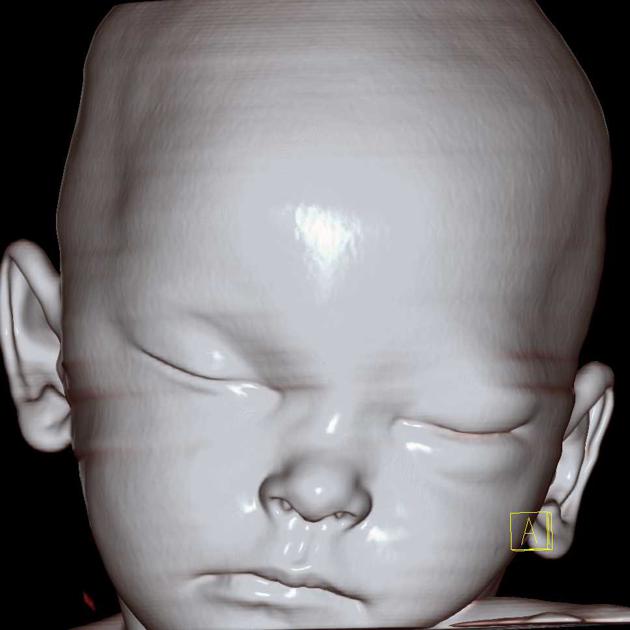
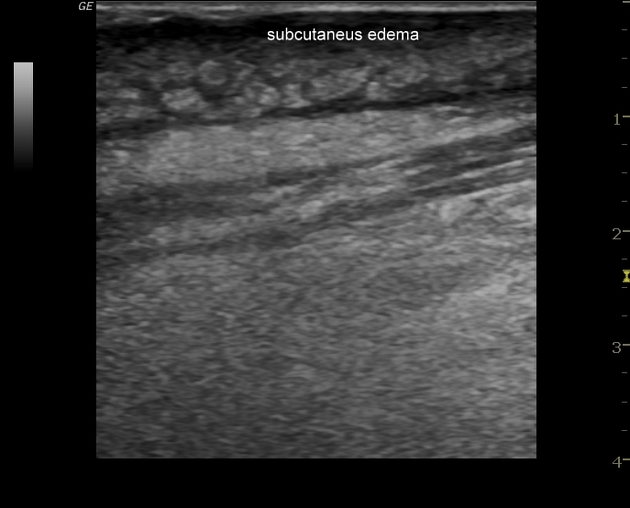
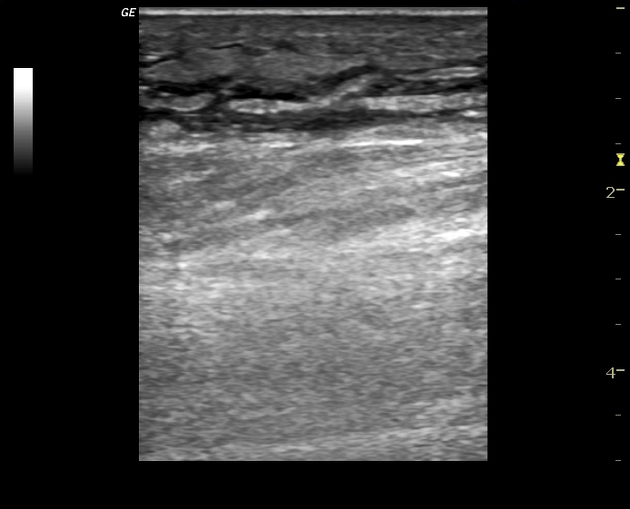
Ultrasound
Ultrasound is usually the first investigation to evaluate a clinical suspicion of cellulitis. Normally the subcutaneous tissue is hypoechoic with few hyperechoic strands (representing connective tissue). Above this, there is a narrow, relatively hyperechoic epidermal-dermal layer. Muscular fascia lies deep to the subcutaneous layer.
-
sonographic hallmarks of cellulitis include abnormal echogenicity and increased thickness of the dermis with indistinct "haziness" and increased echogenicity of the subcutaneous tissue
it is often helpful to compare the area in question to the (presumably normal) contralateral side
-
progressive accumulation of edema in the subcutaneous tissue appears as branching, anechoic striations which impart a lobulated ("cobble-stone" appearance)
this appearance is also present in other edematous states
presence of thickened and abnormally echogenic overlying skin will favor cellulitis over edema
linear anechoic bands of fluid deep to the subcutaneous layer favor lymphedema
ultrasound is more sensitive than MRI for the detection of a retained foreign body as the causative agent, especially if small and wooden 4,5
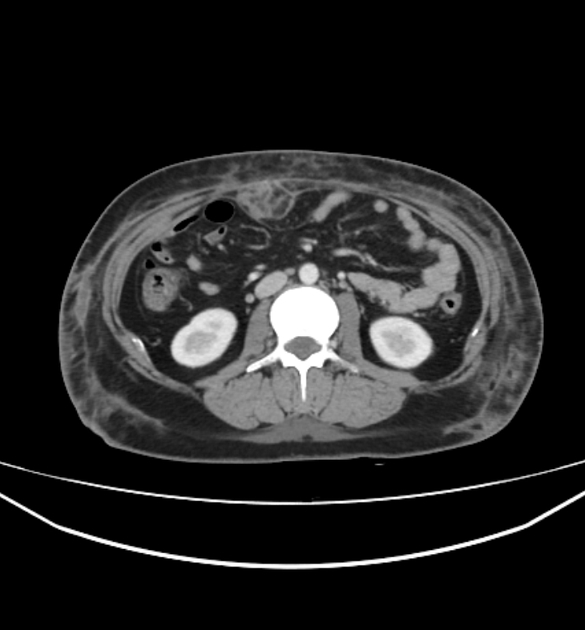
CT
CT is used to accurately differentiate between superficial cellulitis and deep cellulitis.
In uncomplicated cellulitis, CT demonstrates skin thickening, septation of the subcutaneous fat, and thickening of the underlying superficial fascia. If the infection spreads to deeper tissues, soft tissue abscess, infectious myositis, necrotizing fasciitis, and osteomyelitis can all be detected with CT.
MRI
MRI is sensitive for distinguishing cellulitis alone from necrotizing fasciitis and infectious myositis and for showing subcutaneous fluid collections and abscesses. That said, it is seldom required for diagnosing cellulitis and is therefore usually ordered for suspected complications or to rule out alternative diagnoses in cases of an atypical presentation.
Signal characteristics
-
T2 FS or STIR 1,5-9
thickening of skin and superficial fascia
diffuse subcutaneous linear/reticular or ill-defined hyperintensity tending to collect at the hypodermis
T1: corresponding low signal 1,5-9
-
T1C+ 1,5-9
contrast enhancement differentiates cellulitis from stasis edema
cellulitis is also usually unilateral
deep fascia should not enhance
areas of necrotizing cellulitis do not enhance
degree of enhancement depends on the post contrast delay
Treatment and prognosis
Uncomplicated cellulitis is usually treated conservatively with antibiotics and locally supportive measures.
Differential diagnosis
Clinical differential diagnoses include:
subcutaneous abscess
-
also superficial thrombophlebitis
myriad of non-infective erythematous rashes
snake (e.g. crotalid) envenomation
stasis dermatitis
thermal injury










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.