Chronic pancreatitis represents the end result of a continuous, prolonged, inflammatory, and fibrosing process that affects the pancreas. This results in irreversible morphologic changes and permanent endocrine and exocrine pancreatic dysfunction.
On this page:
Epidemiology
The most common cause of chronic pancreatitis in adults is excessive alcohol consumption in developed countries 5. It was formerly thought that malnutrition in developing countries was a cause of chronic pancreatitis, but this myth has since been dispelled 14.
Risk factors
The major risk factors for the development of chronic pancreatitis may be categorised according to the TIGAR-O system 9:
T: toxic-metabolic (e.g. alcohol)
-
I: idiopathic
guidelines recommend that cystic fibrosis needs to be ruled out in these patients before calling it idiopathic 10
-
G: genetic
more commonly seen in the paediatric population
A: autoimmune
R: recurrent
O: obstructive (e.g. choledocholithiasis, pancreatic head tumour)
Clinical presentation
Exacerbations (episodes of acute pancreatitis) may present with epigastric pain. These may recur over a number of years.
Symptoms may be attributable to the failure of:
biliary outflow: jaundice
exocrine function: malabsorption
endocrine function: type 3c diabetes mellitus
Pathology
Acute pancreatitis and chronic pancreatitis are assumed to be different disease processes, and most cases of acute pancreatitis do not result in chronic disease.
In early stages of the disease, there is patchy fibrosis in the pancreatic gland, followed by diffuse fibrosis in later stages. As the disease advances, the pancreatic parenchyma is replaced by sclerotic tissue, causing atrophy. Parenchymal fibrosis leads to progressive strictures, dilatation of the side branches and ectasia of the main pancreatic duct. Severe pancreatitis is characterised by parenchymal calcifications with complications such as pseudocysts, vascular aneurysms and venous thromboses 15.
Radiographic features
Please refer to the article on mass-forming chronic pancreatitis, for further details in this atypical presentation.
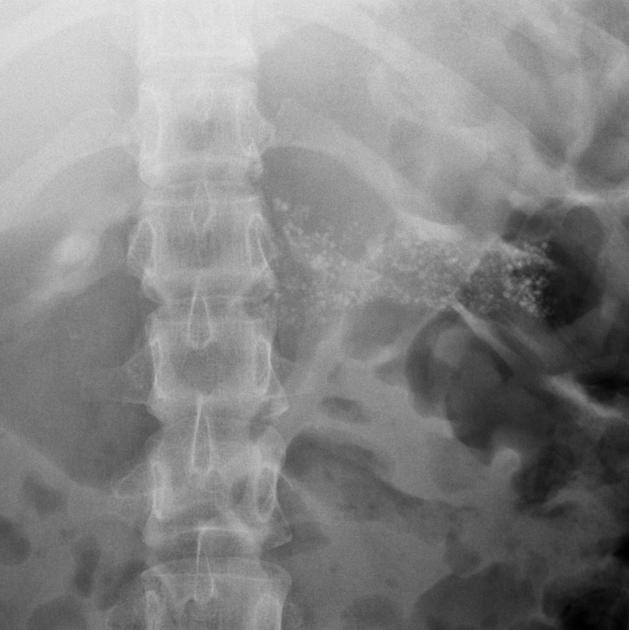
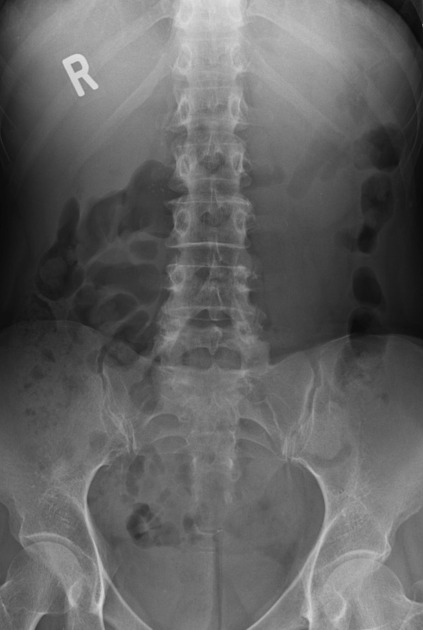
Plain radiograph
While not very sensitive, plain radiographs may show calcification in the pancreas
Ultrasound
The pancreas might appear atrophic, calcified, or fibrotic (advanced stages). Findings that may be present on ultrasound include:
hyperechogenicity (often diffuse) often indicates fibrotic changes
presence of ascites
In moderate to severe stages, pancreatic gland echotexture can be inhomogeneous and rough due to coexistence of fibrotic hyperechoic and hypoechoic focal inflammation 12
Ultrasound may also assist to differentiate between the autoimmune type vs acquired:
pancreas is enlarged (either focally or diffusely) in the autoimmune type
calcifications are visible in acquired types 4 (either parenchymal or intraductal)
Endoscopic ultrasound may also be used to visualise the parenchymal and ductal changes better. EUS guided FNA can also be done.
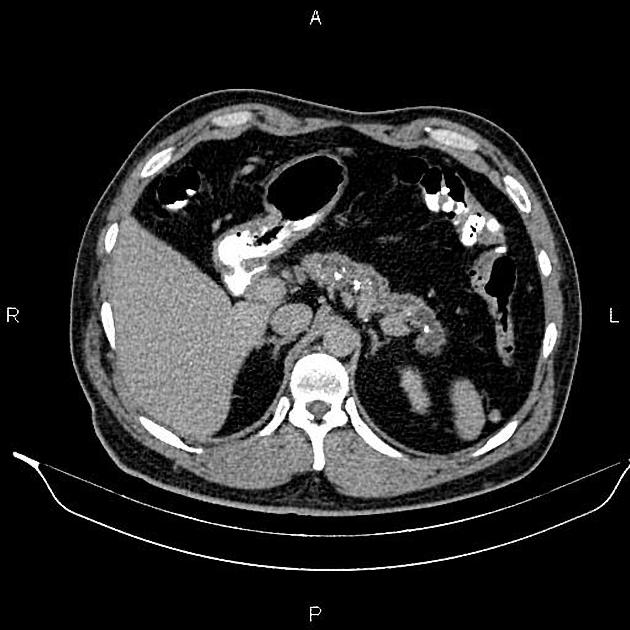
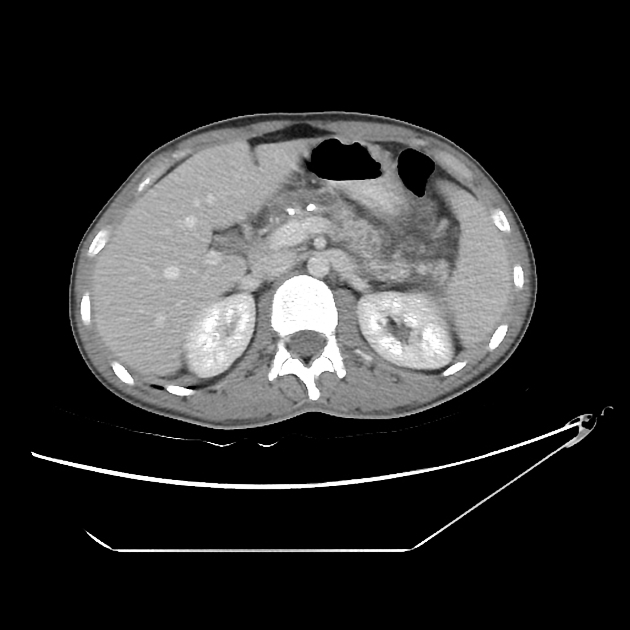
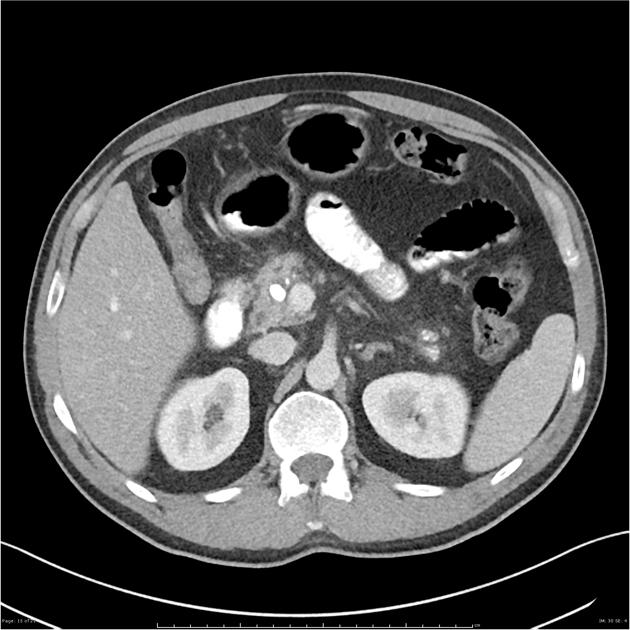
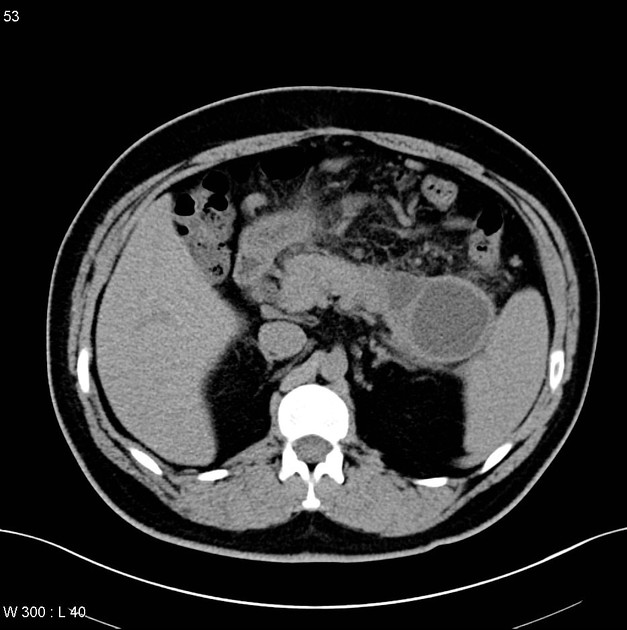
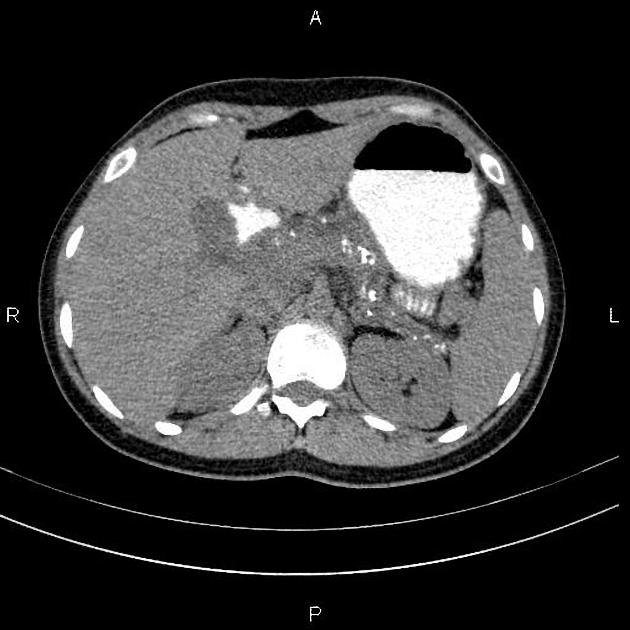
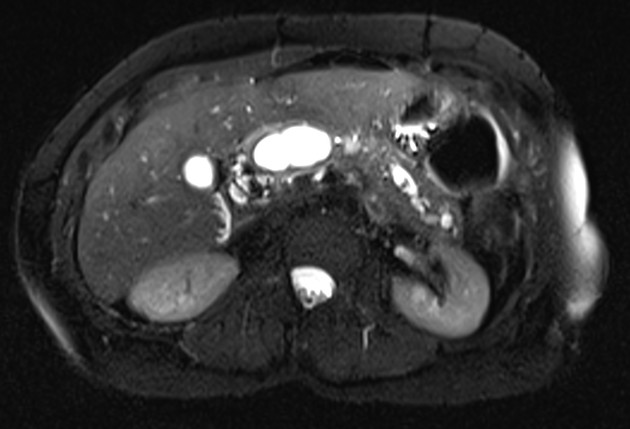
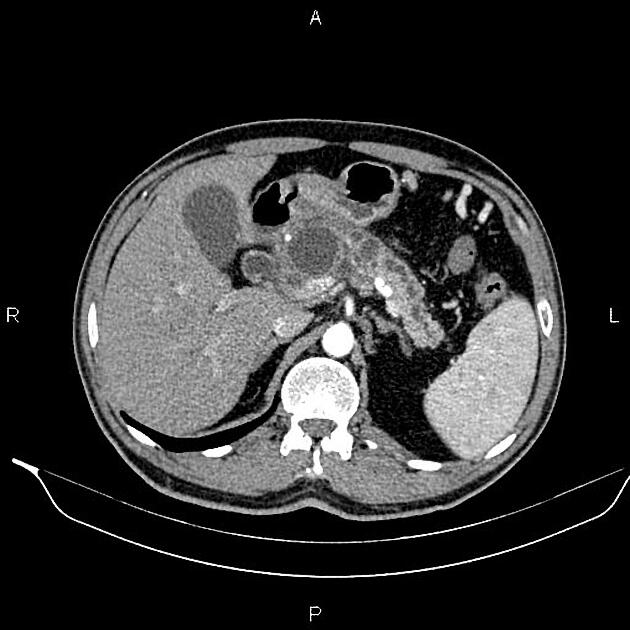
CT
Diagnostic criteria of CT features of chronic pancreatitis are 15:
Moderate pancreatitis (≥2 of the following)
pancreatic enlargement (up to 2x of normal)
irregular head or body of pancreas
focal acute pancreatitis
heterogenous parenchyma
small cavities (less than 10 mm)
dilatation of the main pancreatic duct (2 to 4 mm)
irregular ducts
increased density of main pancreatic ductal wall
Marked pancreatitis (≥1 of the following)
gross enlargement of pancreas (2x of normal size)
large cavities (more than 10 mm)
filling defects within pancreatic duct or calculus within duct
ductal obstruction, stricture, irregularity
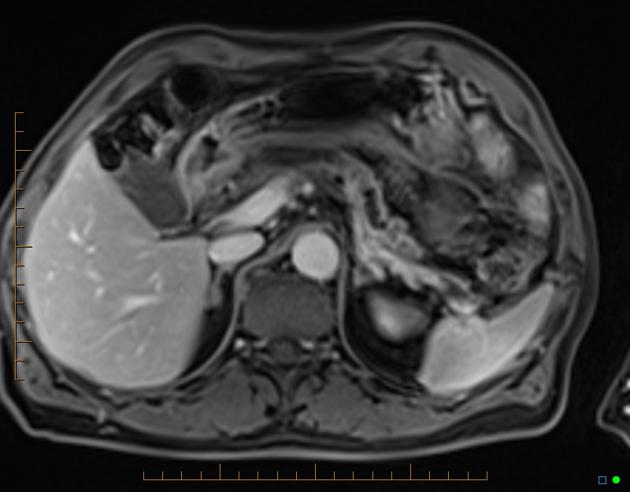
MRI
May be undertaken both as morphological and functional imaging 1,6-8:
Morphological
Features of chronic pancreatitis can be divided into early and late findings:
-
early findings
low-signal-intensity pancreas on T1-weighted fat-suppressed images
decreased and delayed enhancement after IV contrast administration
dilated side branches
-
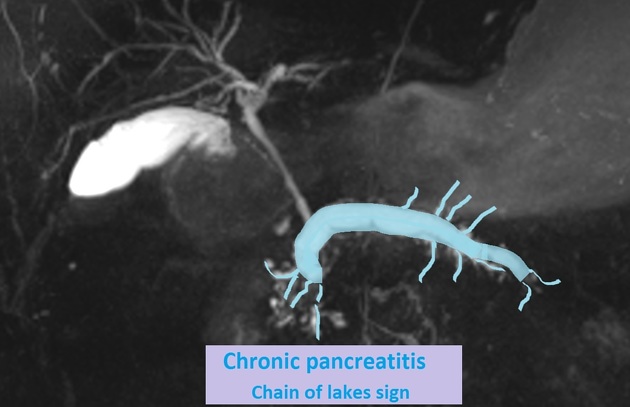
late findings
parenchymal atrophy or enlargement
pseudocyst formation
dilatation and beading of the pancreatic duct often with intraductal calcifications, could give a 'chain of lakes' appearance.
Functional
The exocrine function may be assessed by secretin-enhanced magnetic resonance cholangiopancreatography, SMRCP (a.k.a. MRCP-S). This relatively new technique has shown promising results and may replace endoscopic measuring techniques in the near future 6-8. Imaging protocols to assess exocrine function may contain:
measurement of secretory volume after intravenous secretin-stimulation by assessing T2-high signal changes in the duodenum
post-enhanced dynamic assessment of ADC maps of pancreatic parenchyma, revealing delayed and reduced peak values
Radiology report
Standardised reporting terminology has been suggested for chronic pancreatitis 11. The most used classification is the Cambridge classification, based on the status of the main pancreatic duct (PD) and the presence of side branches abnormalities.
Cambridge classification
-
grade 0, normal:
main PD: normal
abnormal side branches: none
-
grade 1, equivocal:
main PD: normal
abnormal side branches: <3
-
grade 2, mild chronic pancreatitis:
main PD: normal
abnormal side branches: ≥3
-
grade 3, moderate chronic pancreatitis:
main PD: abnormal
abnormal side branches: >3
-
grade 4, severe chronic pancreatitis:
main PD: abnormal
abnormal side branches: presence of filling defect, severe dilatation, irregularity, obstruction or one (or more) large cavity
Treatment and prognosis
Pancreatic enzyme replacement therapy (PERT) has been recommended when there are clinical symptoms or laboratory signs of malabsorption 10. In those patients with refractory pain, in the presence of a dilated main pancreatic duct, endoscopic treatment should be considered, and surgery usually reserved as a second option.
After 20 years of chronic pancreatitis, there is a 6% cumulative risk of developing pancreatic adenocarcinoma.
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.