CNS capillary telangiectasias are small, low flow vascular lesions of the brain, which are usually asymptomatic, incidental findings.
On this page:
Epidemiology
As these lesions are asymptomatic, diagnosis usually matches the age of first imaging with MRI, and as such are most frequently found in middle-aged and elderly adults.
Their prevalence varies according to the series but has been reported at 0.4% at autopsy and 0.7% on MRI 8. They can account for up to ~20% of all cerebrovascular malformations on autopsy studies 2 and are considered the second most common vascular anomaly after developmental venous anomalies on imaging 5.
Clinical presentation
The vast majority (~95%) of capillary telangiectasias are completely asymptomatic and discovered incidentally on MRI when the brain is imaged for other reasons 8. When symptomatic, patients present most commonly with with motor weakness, headache, visual disturbance, or seizures 8.
Occasionally there may be associated intracerebral hemorrhage, although a direct causative relationship has not been definitively established ref. This may be more common with cases of mixed histology ref.
Pathology
The etiology of CNS capillary telangiectasias is not fully known but may be secondary to failed involution of fetal capillary networks or cerebral irradiation 8. Any associated hemorrhage is thought to be secondary to rupture of dysplastic capillaries from venous hypertension 8.
Microscopic appearances
They are comprised of dilated capillaries and are interspersed with normal brain parenchyma with a thin endothelial lining but no vascular smooth muscle of elastic fiber lining 8. This is in contrast to cavernous venous malformations which have no normal brain within their confines ref. Histology can be mixed with a component of cavernous venous malformation ref.
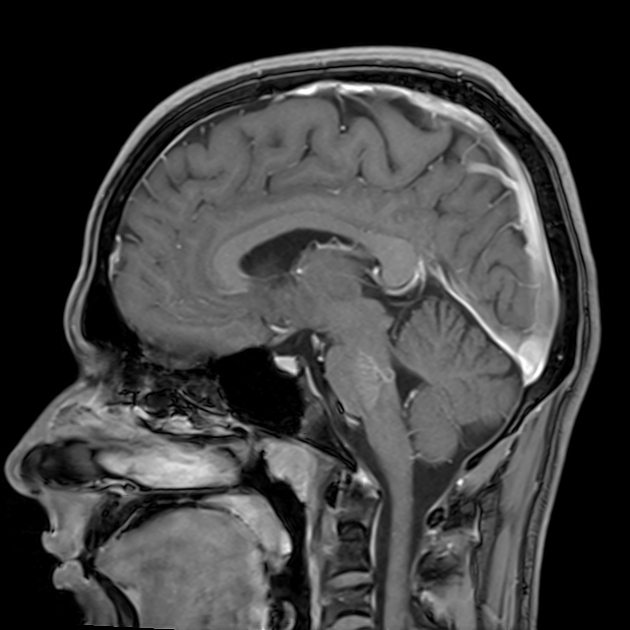
Location
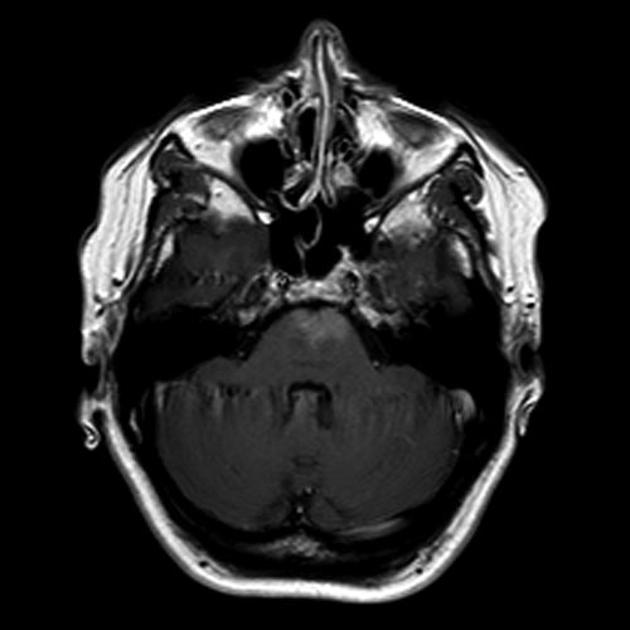
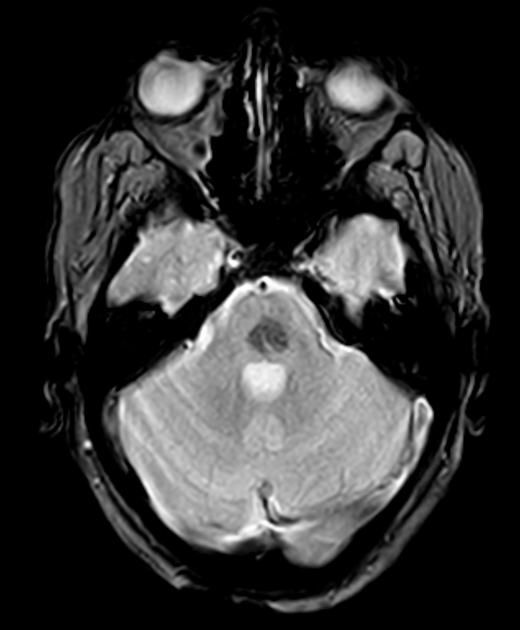
Most capillary telangiectasias occur in the pons (80%) but have been reported to occur in the midbrain, basal ganglia, insular cortex, uncus, cerebellum, and spinal cord 8.
Associations
Radiographic features
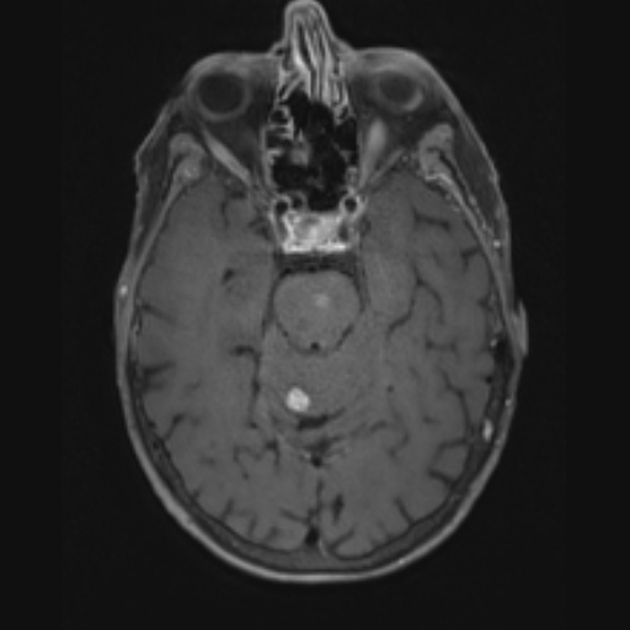
Capillary telangiectasias are mostly located in the brainstem, especially the pons. They are usually solitary but can sometimes be multiple measuring between 3 and 20 mm 8. They have only become widely recognized in the radiology community following the introduction of MRI, as they are usually not seen on CT and DSA 2-5.
MRI
They appear as subtle lesions with no mass effect.
T1: typically iso- to hypointense to brain parenchyma 8
T2/FLAIR: iso- or slightly hyperintense
-
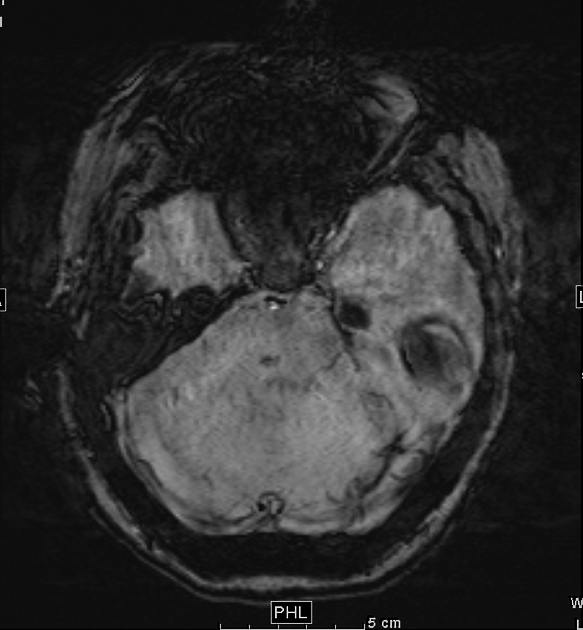
T2*
blooming artifact: ~40% of patients 6
thought to be due to deoxyhemoglobin from sluggish flow, not hemorrhage 2
SWI: more sensitive than T2*, and a low signal is seen in all patients 6-8
-
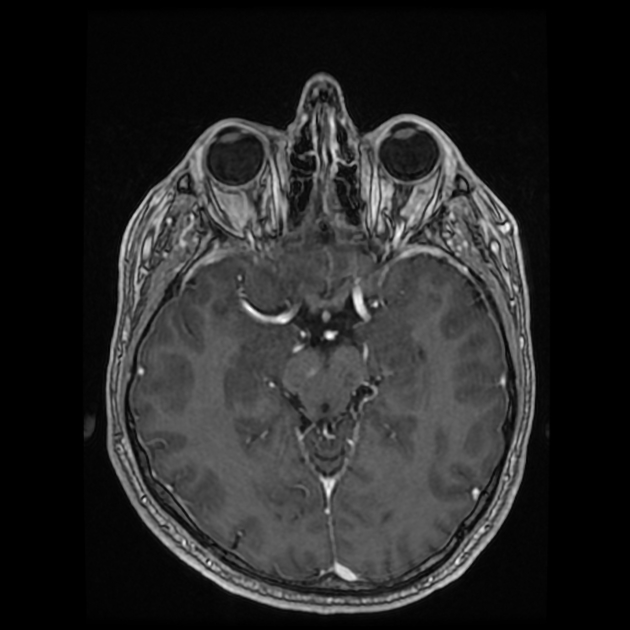
T1 C+ (Gd)
may demonstrate stippled enhancement 8
if large, can show branching/linear draining veins 8
Treatment and prognosis
These lesions are almost always asymptomatic, have interspersed normal brain tissue and are most frequently located in the pons, making treatment difficult. Surgical resection of symptomatic lesions (most commonly seizures) has been rarely reported 8.
Thus, no follow-up is required if the imaging appearances are characteristic ref.
Differential diagnoses
In the majority of cases, no differential needs to be entertained. When appearances are atypical then depending on the actual appearance, one could consider:
-
enhancing mass (usually mass effect present), e.g. diffuse glioma,
subacute ischemic stroke 8
-
vascular malformations
cavernous malformation: usually have "popcorn" appearance on T2WI 8





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.