Corticobasal degeneration (CBD) is an uncommon neurodegenerative disease and is one of the subset of tauopathies.
On this page:
Terminology
Corticobasal syndrome (CBS) represents the clinical syndrome that is diagnosed clinically, while corticobasal degeneration is only reserved for the subset of cases that are pathologically confirmed as the tauopathy 6. The corticobasal syndrome has causes in addition to corticobasal degeneration, including progressive supranuclear palsy (PSP-CBS), frontotemporal dementia, posterior cortical atrophy variant of Alzheimer disease, and Creutzfeldt-Jakob disease 7.
Epidemiology
The vast majority of cases are sporadic, although a number of familial cases have been described 2. Patients are usually in the fifth to seventh decades of life 5, with the youngest reported case being 40 years of age 3.
Clinical presentation
Corticobasal degeneration has a heterogeneous clinical presentation, often making it challenging to diagnose 5.
The classical corticobasal syndrome is a progressive disorder with various asymmetric movement abnormalities, myoclonus, as well as cortical signs including ideomotor apraxia and alien limb phenomenon 5. However, there is a broader phenotype, including 1,2:
akinetic-rigid syndrome, usually beginning in one limb, which unlike in Parkinson disease is not ameliorated by levodopa 1
limb apraxia
limb dystonia
limb myoclonus
postural instability and falls
cognitive impairment, often with pronounced frontal lobe signs 2
cortical sensory loss
alien limb phenomenon 1,2,4
Pathology
The characteristic histopathological findings are neuronal loss and numerous "ballooned" achromatic neurons 1. Although these features are seen throughout the brain, certain regions are more severely affected. They include:
frontoparietal cortex
-
subcortical structures
striatum
substantia nigra
Radiographic features
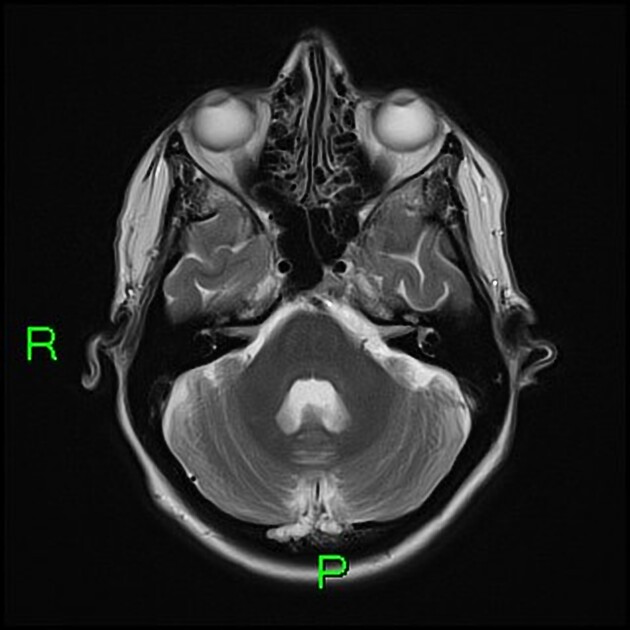
MRI is the modality of choice for assessing corticobasal degeneration, although similar findings can, only to a certain degree, be seen on CT.
MRI
Typical findings include 1,2:
-
asymmetric cortical atrophy
superior parietal lobule: most constant feature
-
perirolandic gyri
precentral gyri
bilateral atrophy of the basal ganglia
atrophy of the corpus callosum 2
-
T2 hyperintensity
subcortical white matter of affected gyri
posterolateral putamen
The pattern of atrophy in corticobasal degeneration may be distinguishable from that of progressive supranuclear palsy. Patients with corticobasal degeneration tend to have atrophy in posterolateral and medial frontal cortical regions, but relatively preserved brainstem anatomy 5.
Research is ongoing regarding the use of techniques such as 3D volumetric MRI and diffusion tensor imaging 5.
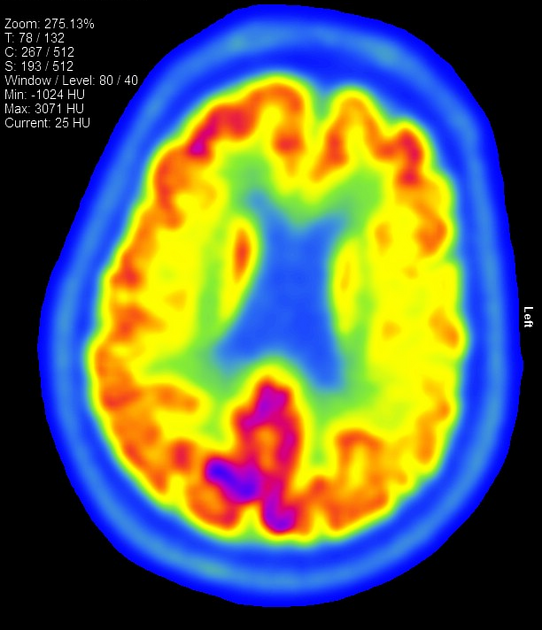
Nuclear medicine
SPECT and PET studies tend to demonstrate hypometabolism in the superior parietal and superior frontal areas, as well as (but less frequently) in the basal ganglia and thalamus 2,5. Early metabolic changes tend to be asymmetrical similar to the clinical presentation.
Treatment and prognosis
There are no drug therapies available to modify the course of corticobasal degeneration. Treatment is often focused on symptomatic relief. Supportive services such as speech and occupational therapy should not be overlooked 5.
Unfortunately, the overall prognosis is poor, with patients demonstrating gradual neurological decline. Death occurs typically 5 to 10 years after the diagnosis is first made 3.
Differential diagnosis
Clinically there is overlap with other conditions, some of which also cause corticobasal syndrome 1,7:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.