Disseminated histoplasmosis, also known as progressive disseminated histoplasmosis, is a severe form of histoplasmosis infection typically seen in immunosuppressed patients, especially in the setting of HIV infection. It results from hematogenous dissemination of the infection, involving multiple organs and systems and associating high mortality 1.
On this page:
Terminology
Although it is sometimes referred to as extrapulmonary histoplasmosis, lung involvement is one of the commonest manifestations of this condition 2.
Epidemiology
Dissemination of the disease is fairly uncommon and may occur in 1 in 2000 acute infections 3.
Risk factors
HIV infection: especially with less than 150 cells/μL CD4 1,4; disseminated histoplasmosis is considered an AIDS-defining illness
immunosuppressive medications 4
biologic immunomodulating agents: infliximab, etanercept 3
immune disorders: idiopathic CD4 lymphocytopenia, Job syndrome, common variable immunodeficiency 4
extremes of ages 4
Clinical presentation
Clinical presentation includes systemic symptoms such as fever, weight loss, and fatigue, and local systems depending on the organs involved, with frequent progressive shortness of breath and diarrhea 1,3.
Physical examination may reveal hepatosplenomegaly, lymphadenopathy, and skin and oral lesions 1.
Pathology
Location
lungs: parenchymal disease 2
bowel: any site of the digestive tube can be involved, with potential bleeding or perforation 1,4
liver and spleen: hemophagocytic lymphohistiocytosis with macrophage activation syndrome 1
kidneys: granulomatous nephritis 1
adrenal glands: adrenal insufficiency 1,3
central nervous system: meningeal, brain or spinal cord lesions 1
skin 1
Radiographic features
Although multiple organs and systems can be affected, only thoracic and abdominal manifestations have been described in detail.
Thoracic
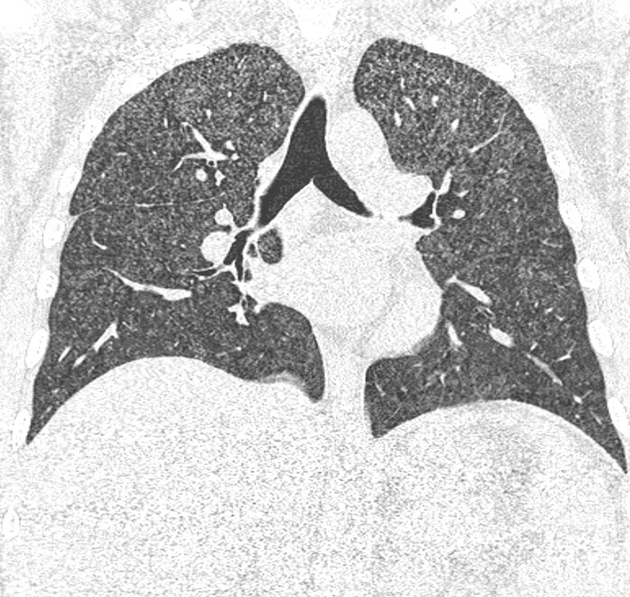
Chest radiographs show pulmonary abnormalities in about 50% of the patients 2. Diffuse multiple small nodules are the most common pattern, even though linear and irregular opacities or segmental, lobar or diffuse air-space opacities can also be observed 2,5.
CT demonstrates diffuse miliary nodules measuring 1-3 mm 3. Pleural effusions and thoracic lymphadenopathy are uncommon 2,3. Calcified lymph nodes or granulomas are described in about one-third of patients, indicating previous contact with the microorganism 2.
Abdominal
hepatosplenomegaly: (30-100% 1,4,6) the spleen may show diffuse decreased attenuation (thought to be a specific finding) and splenic infarcts 6
lymphadenopathy: (~66% 4,6) typically of homogeneous soft-tissue density, but they can also be of diffuse or central low attenuation 6
-
segmentary gastrointestinal inflammation: most common intestinal presentation
affects any site along the digestive tract, but in particular the terminal ileum
there may be associated ulcerations leading to perforation of the small or large bowel, as well as intestinal bleeding 1,4
intestinal inflammatory masses: (less common intestinal presentation) potentially causing large bowel obstruction 1,4
adrenal glands enlargement: rare 1,6
pancreatic enlargement: very rare 4
cholecystitis: very rare 4
ascites 6
Central nervous system
Central nervous system involvement occurs in 5-10% of patients, with focal mass-like lesions in the brain or the spinal cord with possible ring enhancement. Other less common features include meningitis, encephalitis, ischemic lesions, and hydrocephalus 1.
Treatment and prognosis
Initial treatment with liposomal amphotericin B is recommended in the first two weeks, followed by maintenance therapy with itraconazole for a minimum of 12 months 1,4.
Mortality without treatment reaches 80% but reduces to <25% when the appropriate drugs are administered 4.
Differential diagnosis
For pulmonary involvement consider:
miliary metastases 3,5
For hematologic involvement with hepatosplenomegaly and lymphadenopathy consider:
lymphoma 6
Kaposi sarcoma: especially in AIDS patients 6
hepatic and splenic tuberculosis: particularly if there are associated low-attenuation lymphadenopathy 6 and pulmonary nodules
Mycobacterium avium-intracellulare infection 6
For gastrointestinal involvement consider:
inflammatory bowel disease: particularly Crohn disease due to the ileal involvement 4
colonic carcinoma when inflammatory masses are present 4
tuberculous ileitis: especially if there are also pulmonary findings




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.