Dysphagia refers to subjective awareness of difficulty or obstruction during swallowing. It is a relatively common and increasingly prevalent clinical problem. Odynophagia is the term for painful swallowing.
Fluoroscopy is the mainstay of imaging assessment but manometry can help evaluate the oesophageal motor pattern and lower oesophageal sphincter function 1.
On this page:
Epidemiology
Dysphagia is common in older age groups. Women are more prone to have dysphagia than men (80% vs 20%) 2.
Pathology
Dysphagia may be classified depending on the location of this sensation as oropharyngeal or substernal.
Dysphagia can be caused by functional or structural abnormalities of the oral cavity, pharynx, oesophagus, and/or gastric cardia.
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when a patient symptomatically localises a sensation of blockage in the throat.
Functional causes
laryngeal penetration (when contrast seen entering the larynx at fluoroscopy) or aspiration (when contrast extends inferiorly through the true vocal), which are common with patients who have a history of neurologic disorders including stroke
post-operative: e.g. following thyroidectomy 8
Structural causes
oesophageal diverticula, e.g. Zenker, Killian-Jamieson, and epiphrenic diverticula
tumours
-
extrinsic compression, e.g.
anterior osteophytes from cervical spine disease
hypertrophic cartilages e.g. superior thyroid cornu syndrome
occasionally as a complication of anterior cervical spine fusion (~4%) 6
Substernal dysphagia
Substernal dysphagia occurs when a patient symptomatically localises a sensation of discomfort or blockage between the thoracic inlet and the xiphoid process.
Functional causes
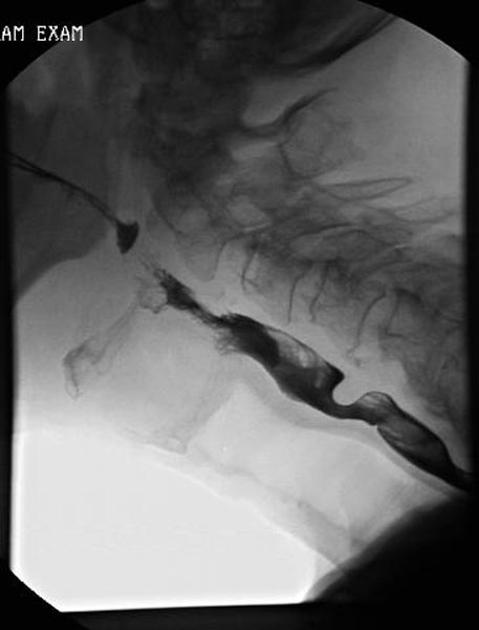
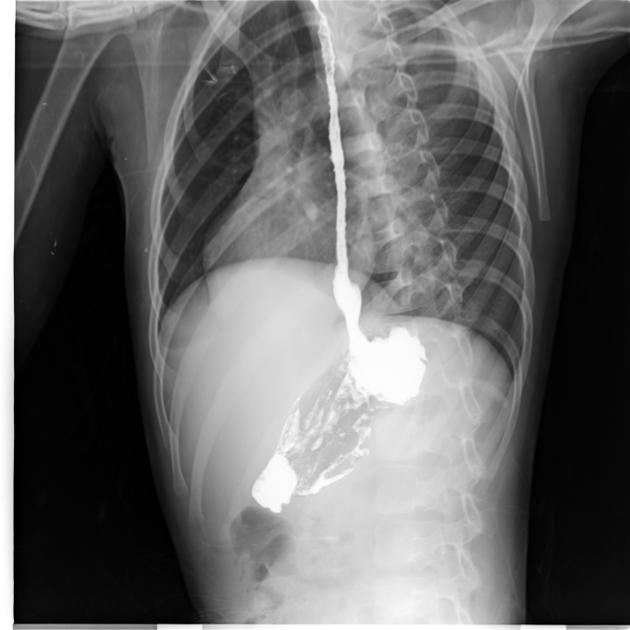
diffuse oesophageal spasm (DES): characterised by multiple spontaneous and uncoordinated oesophageal contractions which have the classic "corkscrew" appearance at oesophagogram
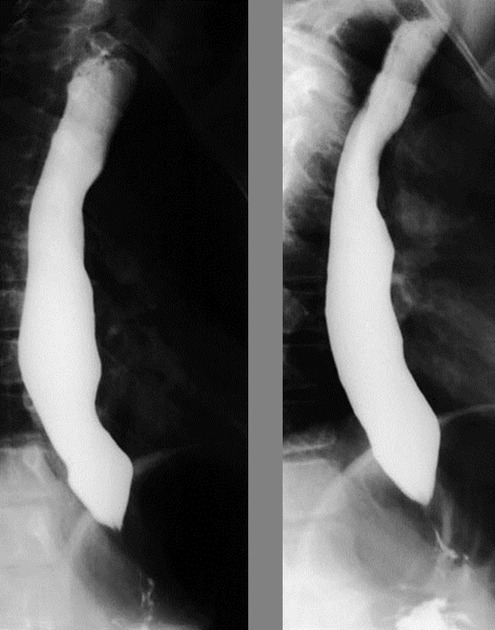
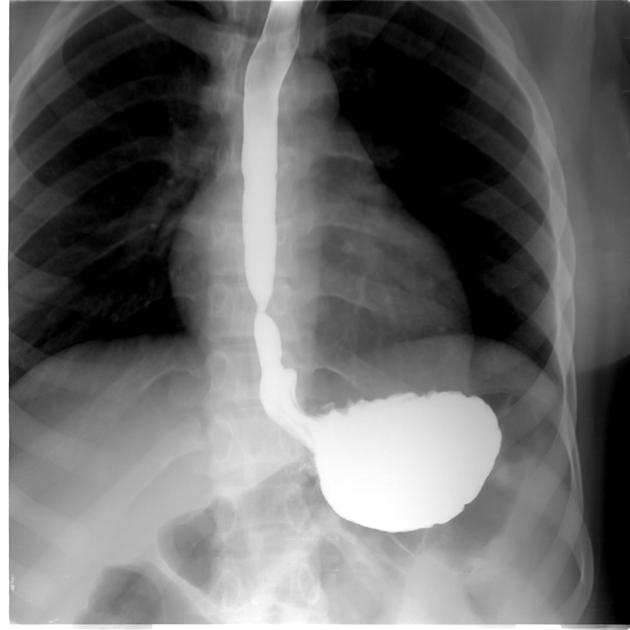
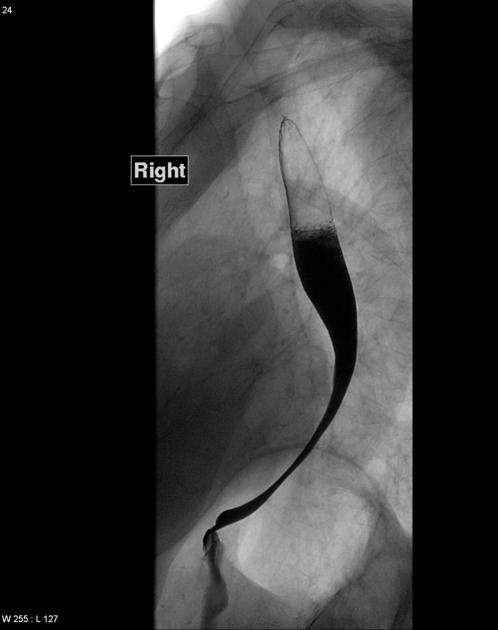
achalasia: characterised by oesophageal dilatation with distal tapered beak-like narrowing at the gastro-oesophageal junction
scleroderma: characterised by oesophageal dilatation with a patulous gastrooesophageal junction
Structural causes
-
peptic strictures most often typically appear as smooth, tapered narrowing in the distal oesophagus
Barrett oesophagus occurs often as a consequence of GORD in the mid-to-upper oesophagus
ring stricture: Schatzki ring is the most common type of oesophageal ring, associated with hiatus hernias
other less common causes of benign strictures include corrosive oesophagitis, Crohn disease, Behçet disease, and eosinophilic oesophagitis
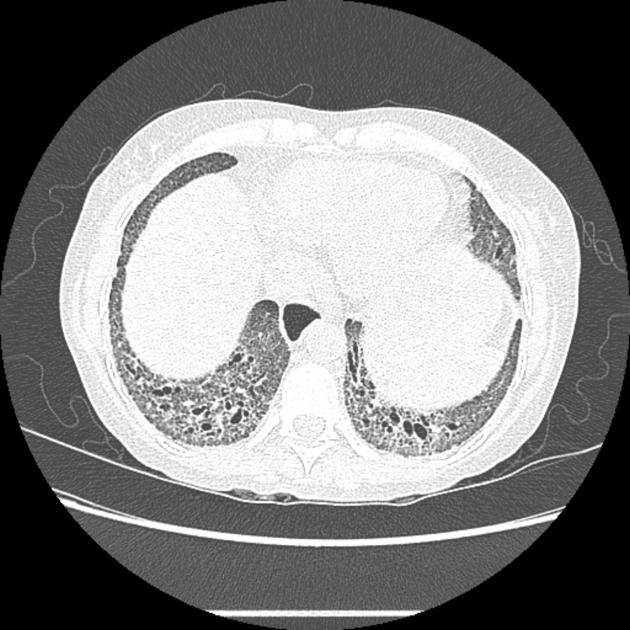
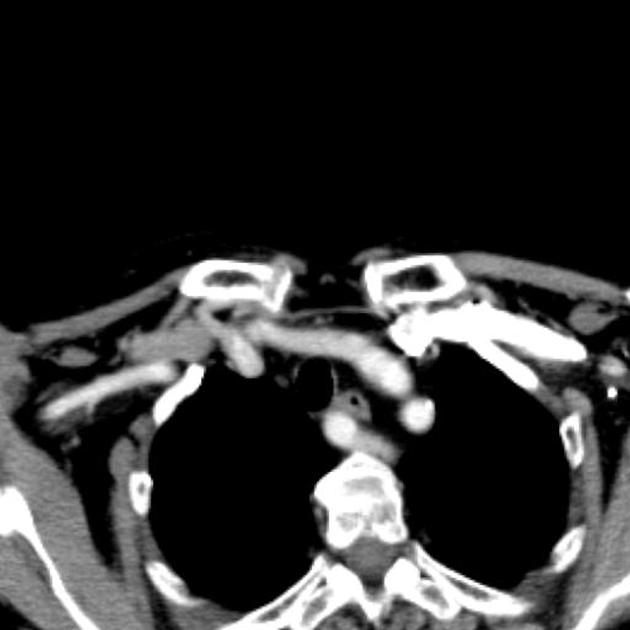
extrinsic mass such as lung cancer or vascular compression, e.g. aberrant right subclavian artery (i.e. dysphagia lusoria) or left atrial enlargement (i.e. dysphagia megalatriensis)
oesophageal infections, such as candidiasis, herpes virus, human immunodeficiency virus (HIV), and cytomegalovirus (CMV)
oesophageal carcinoma can appear infiltrative, ulcerative, polypoid, and/or varicoid at oesophagography
impacted foreign body or food bolus in the oesophagus; water-soluble contrast should be used for increased risk of perforation
Radiographic features
Fluoroscopy
modified barium swallow: used for the evaluation of swallowing mechanisms specifically for aspiration or penetration, this exam is usually performed in conjunction with a speech therapist to assess swallowing function and response to therapeutic strategies 4
barium swallow/oesophagography: provides anatomic and functional information about the pharynx, oesophagus, gastro-oesophageal junction, and gastric cardia, including evaluation of oesophageal motility and assessment for gastrooesophageal reflux
-
barium tablet: may be used to detect subtle areas of oesophageal narrowing 5
the tablet (of known 12.5 mm diameter) should be swallowed with a small amount of water and passage is observed at fluoroscopy; if the tablet becomes lodged in a particular location the patient should swallow a small amount of additional water and if the tablet remains lodged, a more detailed assessment should be performed
CT
Cross-sectional imaging may be used especially if there is a mass effect on the oesophagus seen at oesophagography or for evaluation of oesophageal tumours.
Differential diagnosis
globus pharyngeus sometimes turns out to be the cause of the presentation, this is usually a diagnosis of exclusion









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.