Heterotopic ossification refers to the presence of bone in soft tissue where bone normally does not exist (extraskeletal bone). Lesions range from small clinically insignificant foci of ossification to large deposits of bone that cause pain and restriction of function.
On this page:
Clinical presentation
The most common presentation is with pain around the ossification site. Associated features can include fever, soft tissue swelling, and poor mobility of the affected joint.
Pathology
The pathophysiology is unknown but most theories describe a cellular response to local tissue injury which leads to the release of chemical mediators that stimulate exaggerated bone proliferation. Muscle trauma seems to be a significant triggering event. Heterotopic ossification is histologically identical to normal cortical and cancellous bone.
Acquired heterotopic ossification can be secondary to:
musculoskeletal trauma
spinal cord injury
burns
traumatic brain injury
-
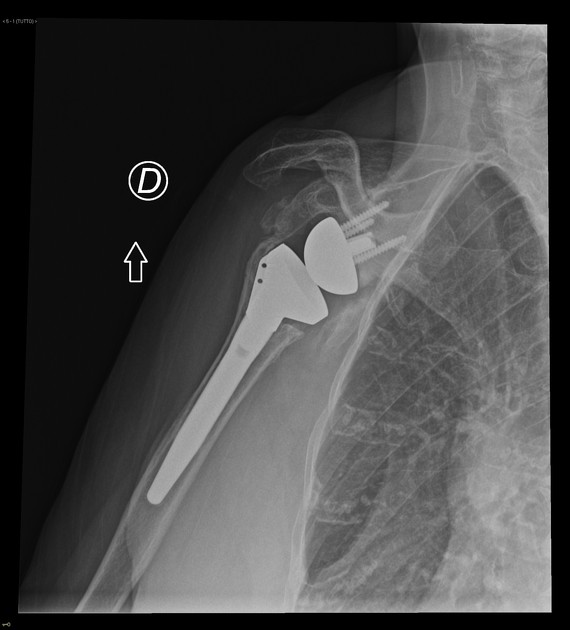
postoperative
mainly seen post joint replacement (approximately 90% of hip joint replacement patients may have heterotopic ossification 12)
often forms adjacent to metal hardware
Rare genetic diseases can cause heterotopic ossification such as fibrodysplasia ossificans progressiva.
Classification
The severity of heterotopic bone formation post total hip arthroplasty has been graded according to several systems.
The Brooker classification is one of the oldest and most widely used systems for grading heterotopic ossification 7,15,16:
grade 1: islands of bone within the soft tissues around the hip
grade 2: bone spurs arising from the proximal femur or pelvis with at least 1 cm of bone between the opposing bony surfaces
grade 3: bone spurs arising from the proximal femur or pelvis with less than 1 cm of bone between the opposing bony surfaces
grade 4: ankylosis of the hip joint
The Della Valle classification is a simpler modified classification system with three grades 7:
grade A: absence of heterotopic ossification (maybe ≥1 island of bone of <1 cm in length)
grade B: presence of ≥1 island of bone of at least 1 cm in length and bone spurs from the pelvis or femur; 1 cm distance between opposing bone surfaces
grade C: bone spurs arising from the pelvis or femur with <1 cm between opposing surfaces or apparent bone ankylosis
The important distinction in reporting the presence of heterotopic ossification is therefore whether the space between opposing bone surfaces is greater or smaller than 1 cm.
Radiographic features
Plain radiograph
The plain film is often the initial imaging investigation. Imaging features evolve as the ossification process progresses.
-
early stage
a typical finding is a soft tissue mass without calcific changes
these can often be missed since radiographs are typically done for vague symptoms of pain
-
mineralization
can occur within 10 days after the causative insult
calcification usually starts peripherally, though cases associated with fibrodysplasia ossificans progressiva can calcify from the central zone towards the periphery
lesions can also be poorly organized without a recognisable mineralization pattern
-
maturation
mature cortical bone is formed if the evolving heterotopic ossification is left untreated
CT
Findings on CT mirror those of plain radiographs but CT is able to identify lesion mineralization earlier and has good overall specificity. It can sometimes be difficult to distinguish the soft tissue lesion seen early on in the evolution of heterotopic ossification from other causes and serial imaging may be required to confirm the evolution of the lesion along the typical course for heterotopic ossification.
-
early stage
low-attenuation soft tissue mass with indistinct surrounding soft tissue planes
it may show contrast enhancement
-
mineralization
zonal mineralization pattern as described previously
a central fatty marrow component can occasionally be seen
-
maturation
mature cortical bone at the periphery
MRI
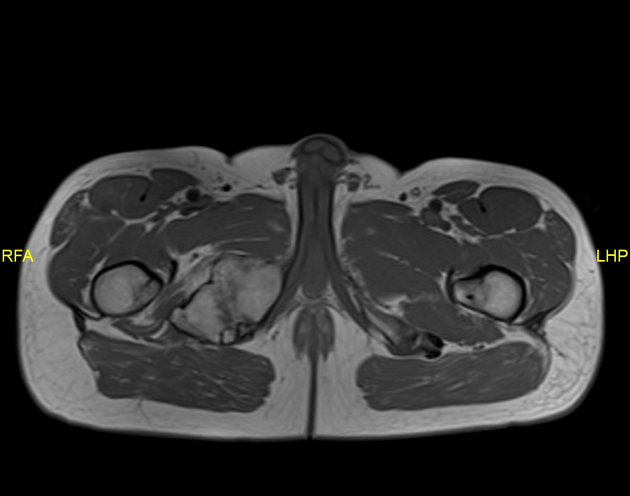
There is no specific role for MRI once the diagnosis of heterotopic ossification has already been made. Instead, MRI is usually used in the assessment of a soft tissue mass. It has the added advantage of evaluating for other possible causes such as neoplasms (i.e. sarcoma) or underlying osteomyelitis.
-
early stage
soft tissue mass with heterogeneous high T2 signal
lesion may manifest simply as enlargement of an involved muscle
surrounding ill-defined high T2 signal representing edema
enhancement of the soft tissue lesion and surrounding edematous tissue
-
mineralization
peripheral low T1 signal in the zonal pattern described
high T1 signal centrally representing fatty marrow change
-
maturation
low T1 signal peripherally in keeping with cortical bone
persisting T2 signal components within the lesion
-
delayed
low signal on STIR with little residual edema












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.