Orbital cavernous venous malformations or cavernous haemangiomas are the most common orbital vascular lesions in adults.
Cavernous malformations are found throughout the body. This article focuses on orbital cavernous haemangiomas. Please refer to the article on cavernous venous malformation for a general discussion.
On this page:
Terminology
NB, according to ISSVA classification of vascular anomalies, these lesions are known as slow flow venous malformations 5. However, it is helpful in reports to include the word "cavernous" (i.e. cavernous venous malformation 5) as this term is ubiquitous in the literature and most familiar to many clinicians.
Epidemiology
Cavernous haemangiomas are the most common vascular lesions of the orbit in adults, accounting for ~7.5% (range 5-9%) 5 of all orbital tumours. However, there is debate about whether these lesions should be considered tumours 3,5. They usually present in middle age (30-50 years), and there appears to be a female predilection 2,3.
Clinical presentation
Orbital cavernous venous malformations are more commonly symptomatic (70%) but can be an incidental finding 5. The clinical presentation usually involves a slowly growing orbital mass, which results in proptosis. Diplopia and visual field deficits (from optic nerve compression) may also occur 3.
Pathology
Cavernous haemangiomas are well-circumscribed masses bounded by a fibrous pseudocapsule, without prominent arterial supply (accounting for the relatively slow enhancement). They are composed of dilated large vascular spaces (thus "cavernous") lined by flattened and attenuated endothelial cells 1,3.
As flow is slow, and vascular spaces large, areas of thrombosis are common 3,4.
Unlike the name "haemangioma" suggests, these lesions may not be tumours as there is no cellular proliferation 3, but rather gradually enlarging vascular malformations and as such, some authors prefer the term cavernous malformation.
In some cases prominent fibrosis is present, and these lesions are referred to by some authors as sclerosing haemangiomas 1.
Radiographic features
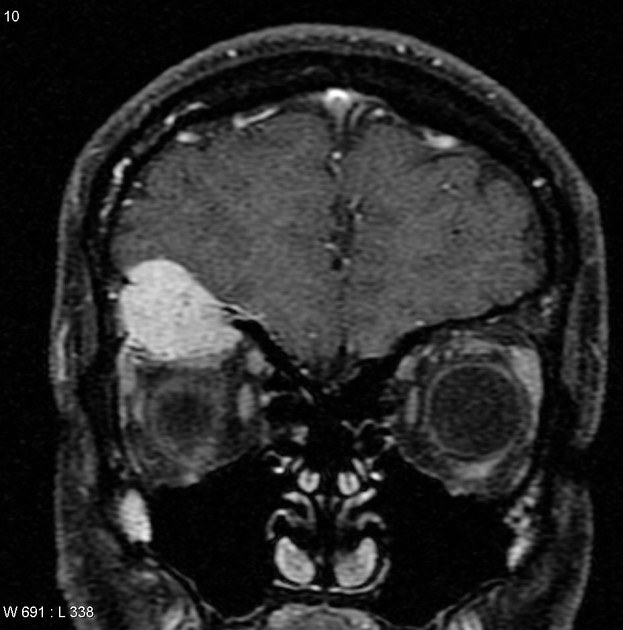
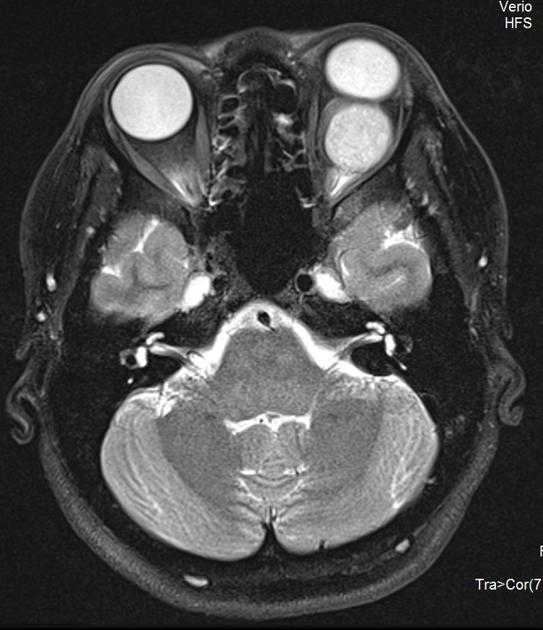
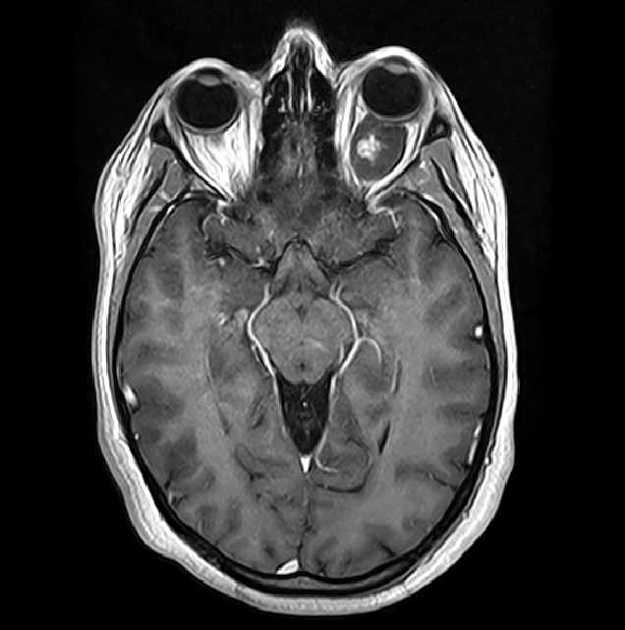
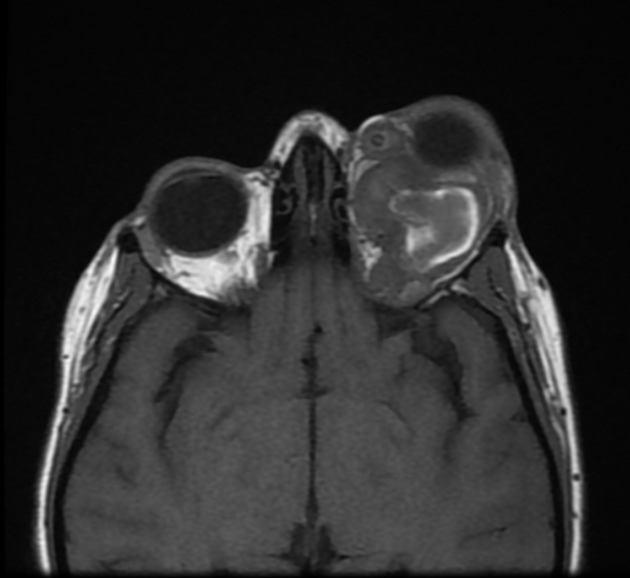
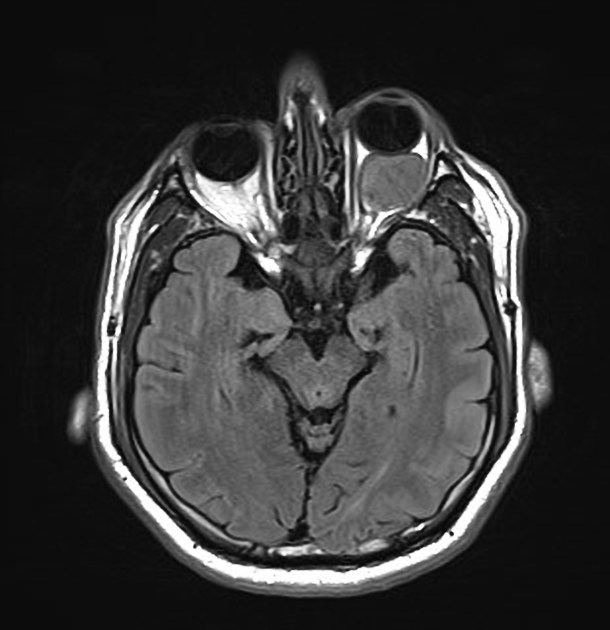
Although cavernous haemangiomas can be located anywhere within the orbit (and for that matter pretty much anywhere in the body: see cavernous venous malformation article) over 80% are located within the intraconal compartment, most commonly in the lateral aspect 1-3.
They are usually round or oval in cross-section and although frequently abut the globe, they do not deform it, but rather are deformed by the globe, on account of their soft consistency 1,3.
Large lesions may be associated with the expansion of the bony confines of the orbit 3.
Ultrasound
Ultrasound demonstrates a smoothly circumscribed retrobulbar lesion with regular moderate to high internal echogenicity 3-4. No flow can be demonstrated on Doppler scanning 4.
CT
Cavernous haemangiomas appear as a well-circumscribed, rounded or oval soft tissue density masses when they are small and become deformed due to their soft nature when getting larger; they are somewhat hypoattenuating compared to the muscle which gradually and incompletely fills in following the administration of contrast 1,2.
The orbital apex is usually spared 3.
Sclerosing haemangiomas sometimes demonstrate calcification 1.
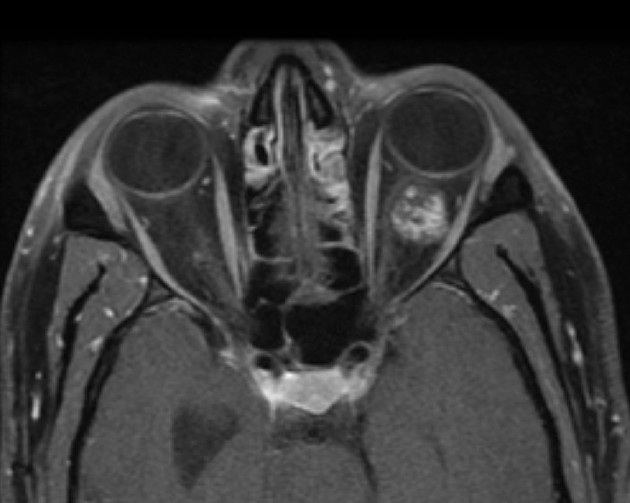
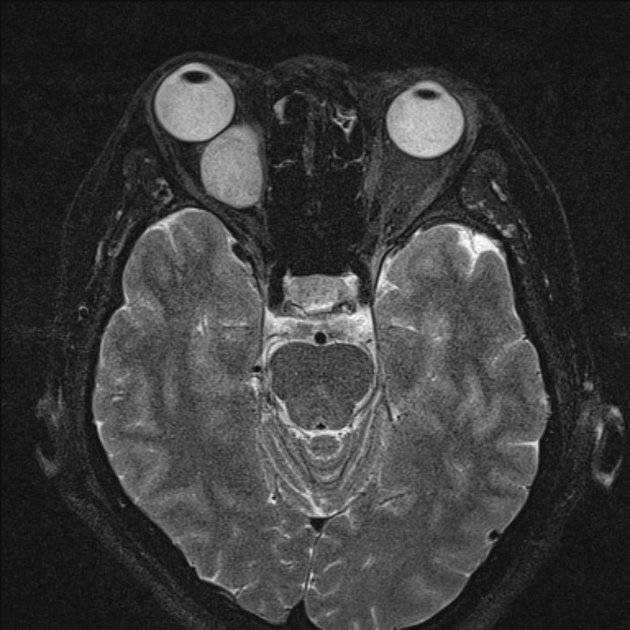
MRI
Appearance on MRI is the same morphologically as on CT, with the following signal intensities:
-
T1
isointense compared to muscle
if areas of thrombosis are present, then hyperintense regions may be visible 3
-
T2
hyperintense compared to muscle
may have low-intensity septation
pseudocapsule is of low intensity
T1 C+ (Gd): slow mild arterial enhancment with progressive fill in and subsequent homogeneous or heterogeneous enhancment on delayed phases 5-7
Angiography (DSA)
Angiographically haemangiomas are occult as enhancement occurs only in a delayed fashion 2.
Treatment and prognosis
If the lesion is found incidentally and no exophthalmos or visual complications are present then conservative management is recommended, with periodic MRI imaging 5.
In cases where symptoms are present or growth of the lesion is demonstrated on follow-up imaging, surgical removal is usually effective 5.
Differential diagnosis
The differential depends on the location but is essentially that of orbital vascular lesions with the addition of a few non-vascular tumours.
For the more common intra-conal variety the differential includes 1-3:
sclerosing haemangioma (a variant rather than a distinct entity)
If extraconal the differential also includes 1-3:












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.