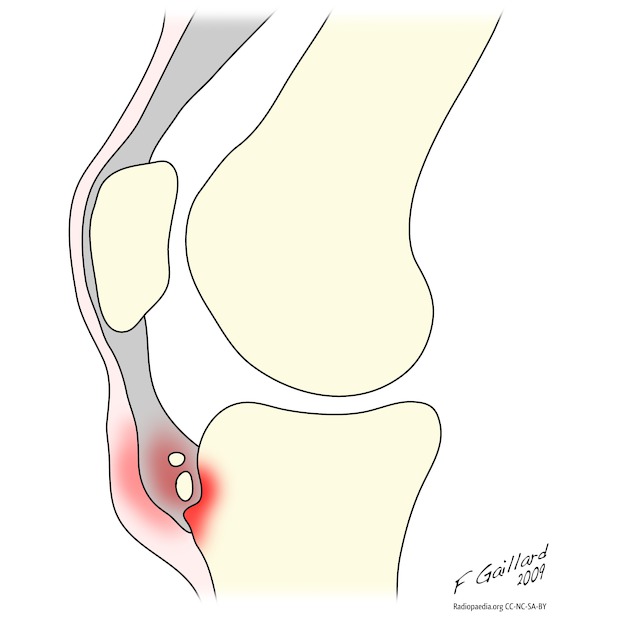
Osgood-Schlatter disease, also known as apophysitis of the tibial tubercle, is a chronic fatigue injury due to repeated microtrauma at the patellar tendon insertion onto the tibial tuberosity, usually affecting boys between ages 10-15 years.
On this page:
Terminology
Unresolved Osgood-Schlatter disease is the term given to clinical and radiological findings that persist into adulthood 10.
Epidemiology
Osgood-Schlatter disease is seen in active adolescents, especially those who jump and kick. It is bilateral in 25-50% of patients 1-3. The typical age of onset in females may be slightly earlier (boys 10-15 years; girls 8-12 years) 8.
Clinical presentation
Clinically, patients present with pain and swelling over the tibial tuberosity exacerbated with exercise.
Radiographic features
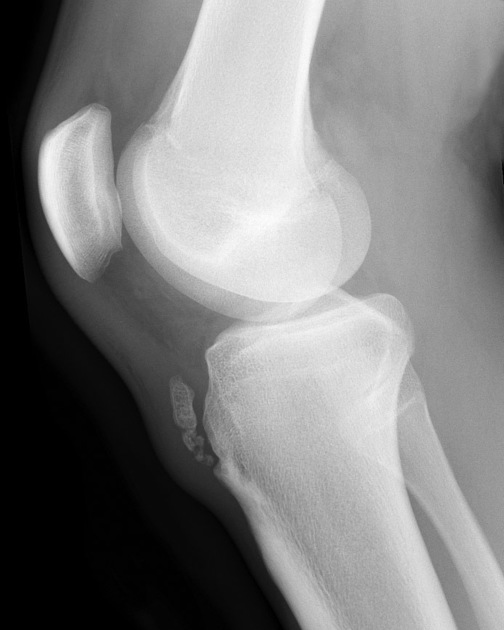
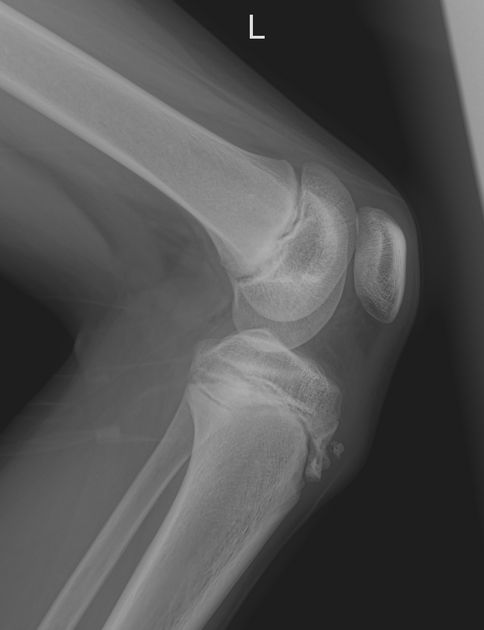
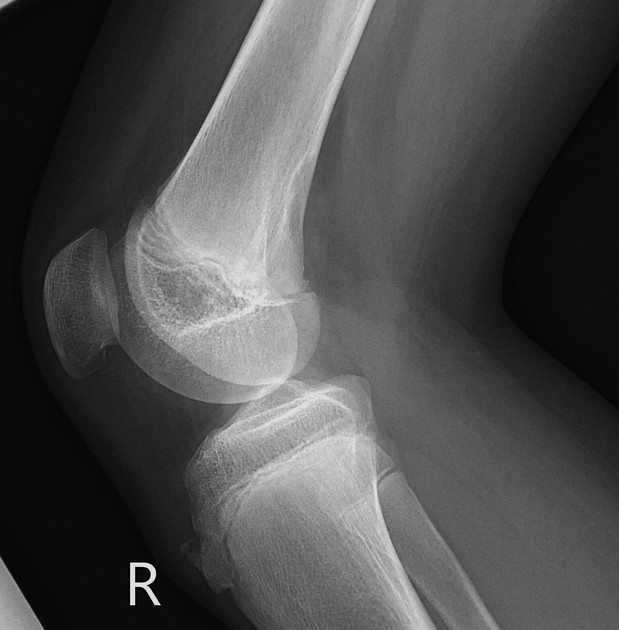
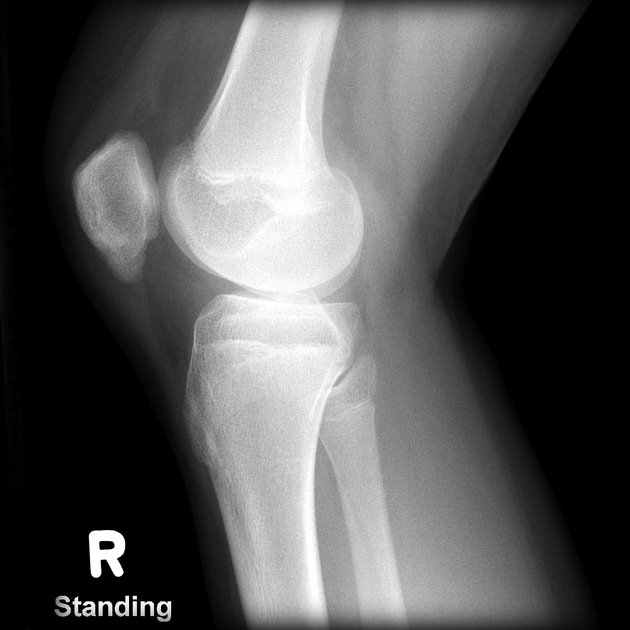
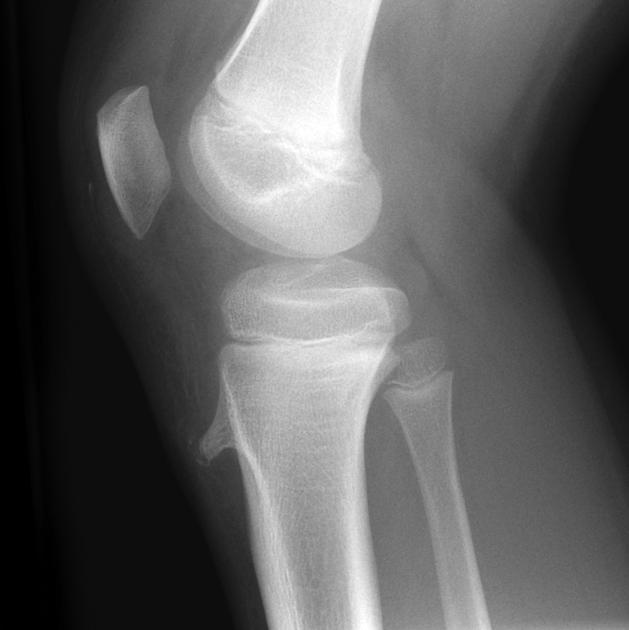
Plain radiograph
Soft tissue swelling with loss of the sharp margins of the patellar tendon is the earliest sign in the acute phase; thus, a compatible history is also essential in making the diagnosis. Bone fragmentation at the tibial tuberosity may be evident 3 to 4 weeks after the onset.
It is important not to equate isolated 'fragmentation' of the apophysis with OSD, as there may well be secondary ossification centres.
Ultrasound
Ultrasound examination of the patellar tendon can depict the same anatomic abnormalities as can plain radiographs, CT scans, and magnetic resonance images. The sonographic appearances of Osgood-Schlatter disease include 3:
- swelling of the unossified cartilage and overlying soft tissues
- fragmentation and irregularity of the ossification centre with reduced internal echogenicity
- thickening of the distal patellar tendon
- infrapatellar bursitis
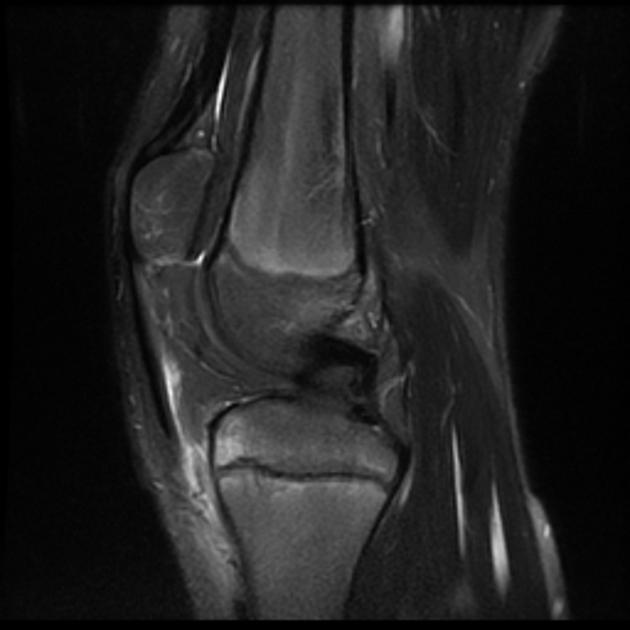
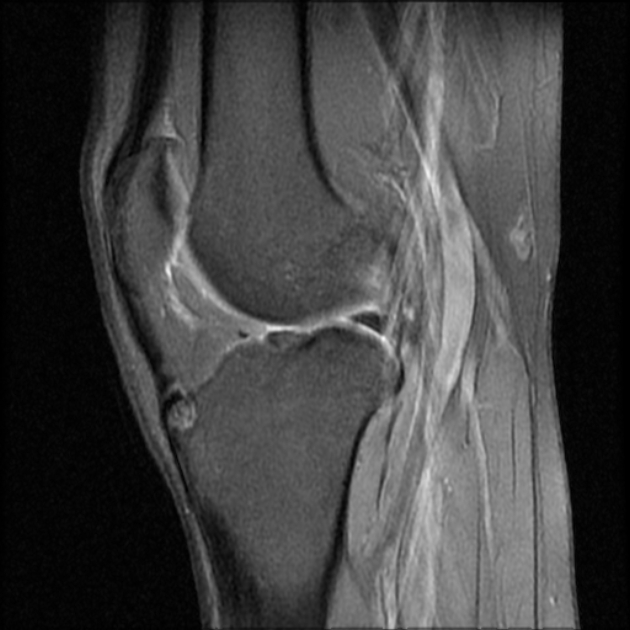
MRI
MRI, as expected, is more sensitive and specific, and will demonstrate:
- soft-tissue swelling anterior to the tibial tuberosity
- loss of the sharp inferior angle of the infrapatellar fat pad (Hoffa fat pad)
- thickening and oedema of the distal patellar tendon
-
infrapatellar bursitis (clergyman's knee)
- a distended deep infrapatellar bursa can be a frequent finding 6
- bone marrow oedema may be seen at the tibial tuberosity
Treatment and prognosis
Treatment is usually conservative and involves rest, ice, activity modification (decreasing activities that stress the insertion, especially jumping and lunging sports), and quadriceps and hamstring strengthening exercises. Analgesia and padding to prevent pressure on the tibial tuberosity are also useful. Only rarely are therapeutic casts required 4,5. The condition usually spontaneously resolves once the physis closes.
In rare cases, surgical excision of the bone fragment(s) and/or free cartilaginous material may give good results in skeletally mature patients who remain symptomatic despite conservative measures 10.
Adults with findings of prior Osgood-Schlatter disease are more likely to have patella alta and are at a higher risk of patellofemoral maltracking with subsequent chondrosis, and transient patellar dislocation 11.
History and etymology
It is named after American orthopaedic surgeon Robert B Osgood (1873-1956) and Swiss professor of surgery Carl Schlatter (1864-1934).
Differential diagnosis
Imaging differential considerations include:
- Sinding-Larsen-Johansson disease (SLJ): similar condition involving the inferior pole of the patella
- jumper's knee: involves the patellar tendon rather than the bone, and is essentially tendinopathy with focal tenderness, although it may eventually be associated with bony changes (some authors do not distinguish between SLJ and jumper's knee)
- infrapatellar bursitis
























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.