Otospongiosis, also known as otosclerosis, is a primary osteodystrophy of the otic capsule (bony labyrinth of the inner ear). It is one of the leading causes of deafness in adults.
On this page:
Terminology
The term otosclerosis is somewhat of a misnomer. Much of the clinical course is characterized by lucent rather than sclerotic bony changes and hence it is more appropriately known as otospongiosis which is a term preferred by many head and neck radiologists.
Epidemiology
Typically, patients present during their 4th and 5th decades. However, because the condition tends to have symptoms that gradually worsen, it is often difficult to precisely determine onset 6. Presentation during childhood is uncommon.
A female predilection is present with a F:M ratio of ~2:1. Caucasians are more frequently affected than other racial groups 6,7. In up to 50% of cases, a familial predisposition can be identified 7.
Histologic prevalence of otospongiosis has been reported between 3.4-10% in unselected Caucasian temporal bones 7.
Clinical presentation
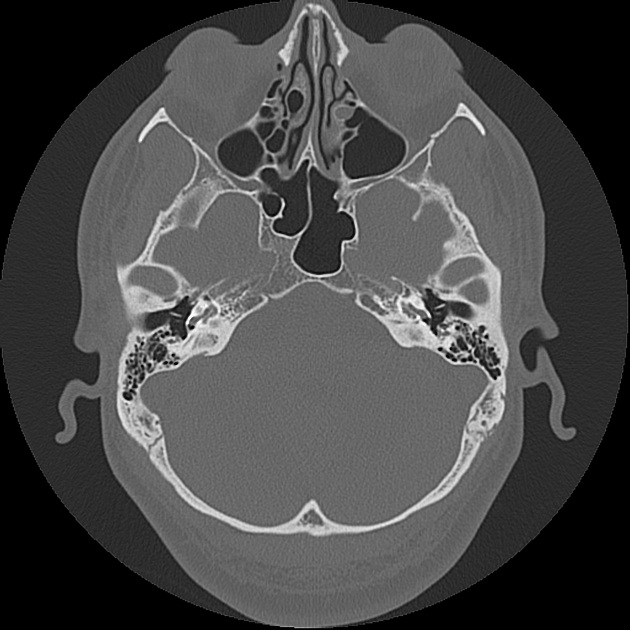
Otospongiosis most commonly presents with hearing loss, most often conductive, but can also be sensorineural or mixed, and is frequently bilateral 3,9. The clinical course is usually slowly progressive over the years. Hearing loss may be exacerbated by pregnancy 6.
On otoscopy, there are usually minimal or no findings, except in severe cases where cochlear involvement can result in hyperemia of the cochlear promontory (Schwartze sign) 1-3. On pure-tone audiometry, there may be a characteristic decrease in bone conduction at 2000 Hz (Carhart notch).
Pathology
The pathophysiology of otosclerosis is multifactorial and incompletely understood, with genetic, viral, inflammatory and autoimmune components 9,10.
Two phases are described: early/active (otospongiosis) and late/inactive (otosclerosis). In the early phase, lesions consist predominantly of histiocytes, osteoblasts and osteocytes, the latter being the most active cell group. The bone around pre-existing blood vessels is absorbed, creating a better microcirculation. Eventually, osteoblasts become more involved, resulting in the formation of irregular foci of new spongy bone 9. This new bone appears densely blue on hematoxylin and eosinophil staining and is known as the blue mantles of Manasse.
Subtypes
There are two subtypes:
-
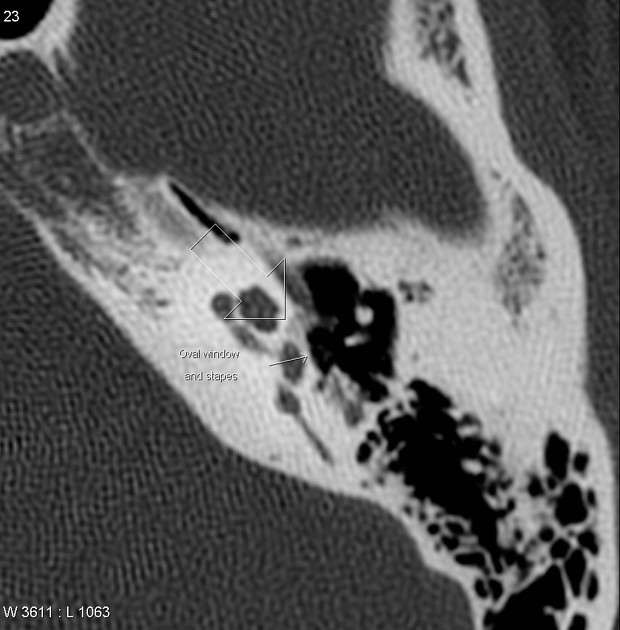
fenestral (stapedial): ~80%
involves the oval window and the stapes footplate
hearing loss is often conductive, due to stapes thickening and fixation
-
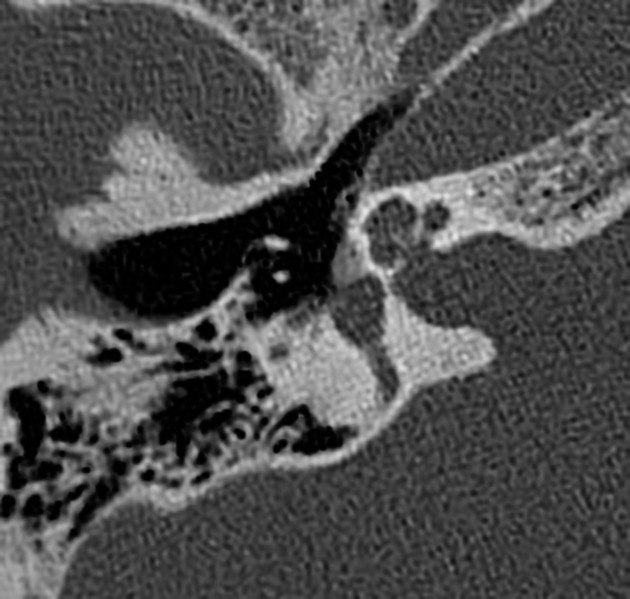
retrofenestral (cochlear): ~20%
cochlear involvement with demineralization of the cochlear capsule
hearing loss is often sensorineural, but the mechanism by which this occurs is uncertain
NB: the prefix 'retro' does not mean 'posterior' but rather 'behind', as in 'deep to', the medial wall of the middle ear from the perspective of otoscopy.
Retrofenestral otosclerosis usually occurs with fenestral involvement, so the two entities are considered a continuum rather than distinct 11.
Radiographic features
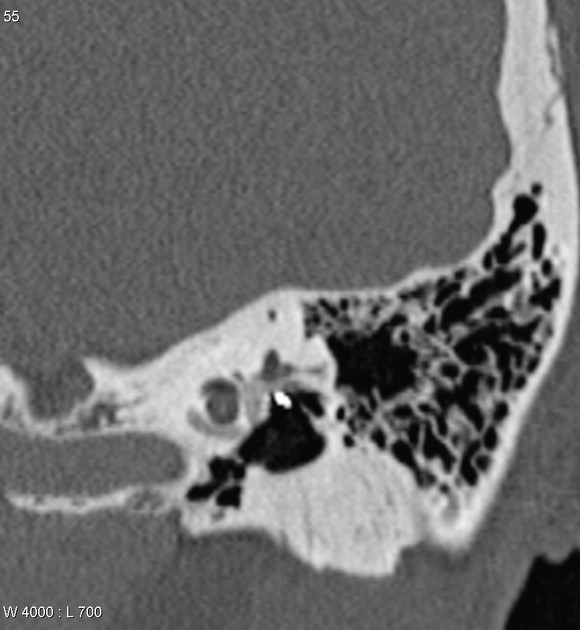
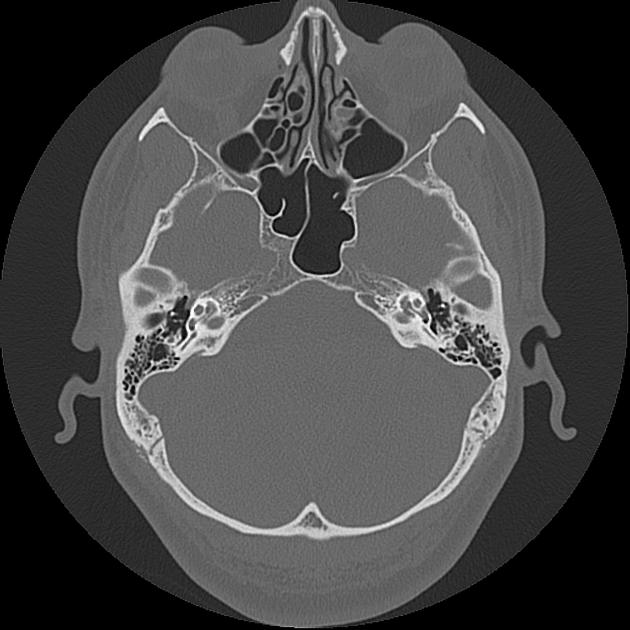
CT
Thin-slice CT scan through the temporal bones, also called high-resolution CT, is the imaging modality of choice. Axial and coronal (or preferably 20 degrees coronal) thin-slice bone algorithm non-contrast scans are needed to adequately demonstrate the inner ear structures and subtle early changes 1-3.
On imaging, two main types of presentations have been described:
-
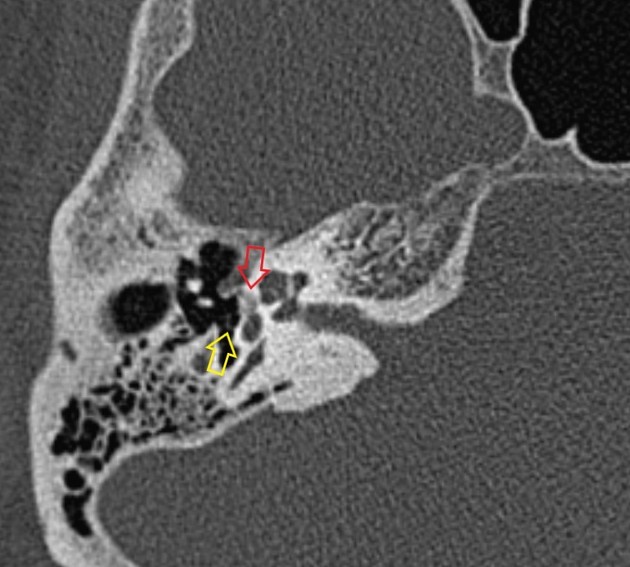
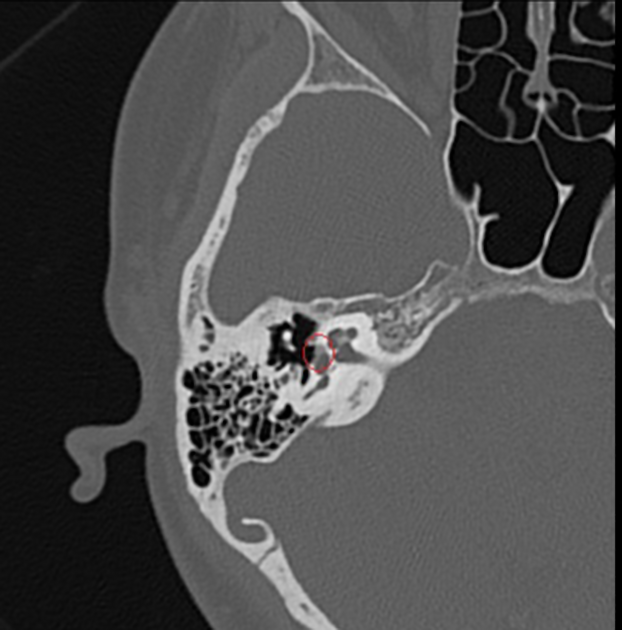
fenestral
the most common
the site of involvement is just anterior to the oval window, involving a small cleft known as the fissula ante fenestram 5
bony overgrowth can cause fixation of the stapes
-
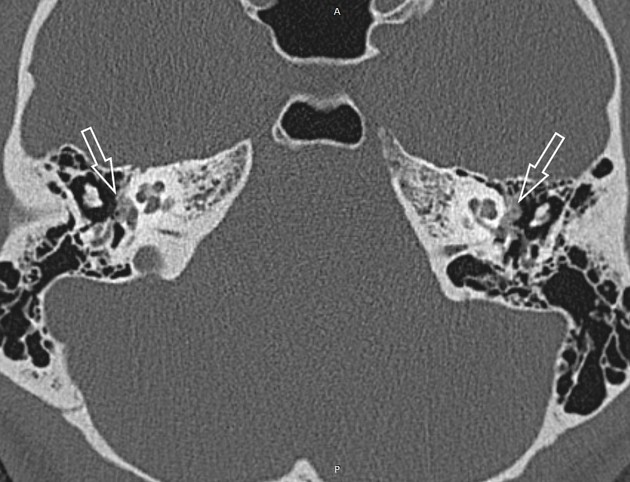
retrofenestral
the second most common
involvement of the round window niche, which when present usually accompanies fenestral disease 12, however, isolated round window otosclerosis can occur on occasion 12,13
the bone surrounding the cochlea is the site of involvement, which may be focal or circumferential 1-3, with the latter producing a "fourth turn" or "double ring" sign 14
Findings depend on the phase of the disease:
-
otospongiotic phase
there are demineralization and formation of spongy bone, manifest as decreased attenuation (lucency) within the normally homogeneously dense border of the otic capsule
-
otosclerotic phase
the region increases in attenuation
-
as otosclerotic bone may be difficult to distinguish from surrounding normal bone, some have identified diagnostic criteria using the thickness of the otic capsule or an abnormally convex contour of the otic capsule cortex anterolateral to the anterior margin of the oval window 13
in severe cases, the oval window and/or, less commonly, the round window is completely filled in by a dense bony plate (with complete fixation of the stapes)
CT grading system (Symons and Fanning)
Various authors have used CT grading systems of otosclerosis in their studies. In 2009, a Lee et al 3 article assured that the Symons and Fanning CT grading system yields excellent interobserver and intraobserver agreement:
-
grade 1
solely fenestral, either spongiotic or sclerotic lesions, evident as a thickened stapes footplate, and/or decalcified, narrowed or enlarged round or oval windows
-
grade 2
-
patchy localized cochlear disease (with or without fenestral involvement)
grade 2A: basal cochlear turn involvement
grade 2B: middle / apical turns involvement
grade 2C: both the basal turn and the middle / apical turns involvement
-
-
grade 3
diffuse confluent cochlear involvement of the otic capsule (with or without fenestral involvement)
MRI
MRI has a limited role. In retrofenestral otosclerosis, pericochlear, and perilabyrinthine soft tissue intensity signal on T1 with contrast enhancement may be demonstrated. Increased T2 signal may also be present 8.
Treatment and prognosis
A stapedectomy with stapes prosthesis is the treatment of choice for fenestral otosclerosis 4.
In the first part of the 20th century, a procedure referred to as fenestration was performed, in which a neo-window was created in the lateral semicircular canal or vestibule to allow passage of sound waves into the inner ear, bypassing the ossicular chain. These changes should not be mistaken with labyrinthine fistulae or middle and inner ear malformations 4.
Differential diagnosis
-
otic capsule lucencies similar to otosclerosis, non-deformed fragile bones, and blue sclera
-
bony expansion in elderly patients
-
occurs in the treatment field and results from vascular injury and resultant bony ischemia
History and etymology
It was first described by the Italian anatomist, Antonio Maria Valsalva (of the maneuver fame) in 1735.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.