Citation, DOI, disclosures and article data
Citation:
Weerakkody Y, Thibodeau R, Kearns C, et al. Peritesticular lipoma. Reference article, Radiopaedia.org (Accessed on 25 Feb 2025) https://doi.org/10.53347/rID-77256
A peritesticular lipoma, or lipoma of the spermatic cord, is the most common benign tumor of the paratesticular tissues and spermatic cord (representing ~45% of paratesticular masses 4).
The term 'spermatic cord lipoma' is variably used to mean a true lipoma of the spermatic cord (originating from adipose cells and with no communication with the inguinal canal), or in surgical literature referring to intraperitoneal fat extending through the inguinal canal 5.
Usually an incidentally discovered non-tender soft scrotal mass 4.
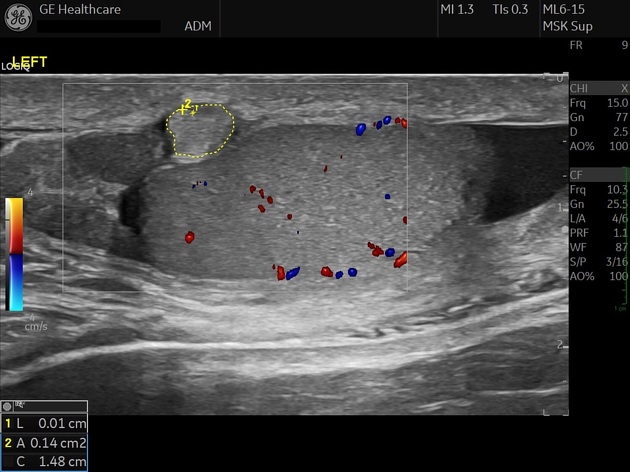
Ultrasound
Typically a well-circumscribed, homogeneous, hyperechoic, and relatively avascular mass 4,6.
The absence of communication with the inguinal canal, reducibility, and bowel content/peristalsis help to differentiate from an inguinal hernia or lipoma, although a strangulated or incarcerated hernia may be aperistaltic and irreducible 4. The presence of a poorly circumscribed mass, heterogenous echotexture, or vascularity, should raise the possibility of liposarcoma 4,5.
CT
While sometimes an incidental finding, this modality may also be used to help evaluate lesions with unclear or concerning characteristics on ultrasound 5,6. Characteristic homogenous, circumscribed fat attenuation, without inguinal canal communication or contrast enhancement, may be appreciated 5.
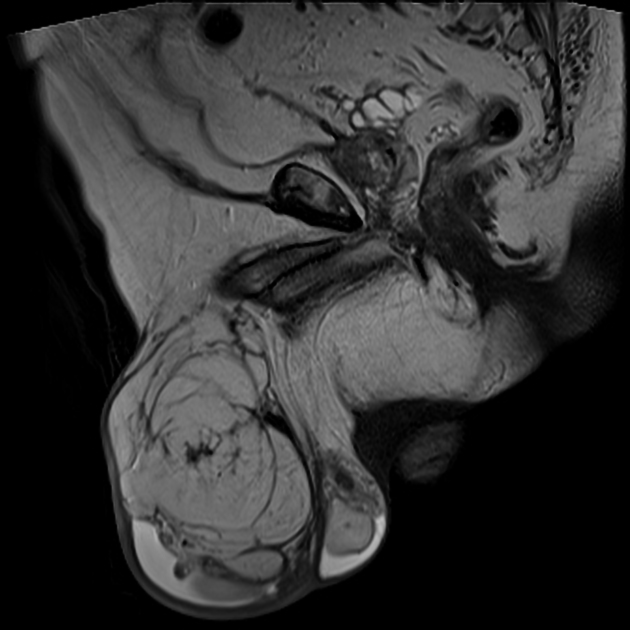
MRI
-
1. Syed Ali Akbar, Tawfeeq Amjadali Sayyed, Syed Zafar Hasan Jafri, Farnaz Hasteh, James Simeon Adams Neill. Multimodality Imaging of Paratesticular Neoplasms and Their Rare Mimics1. (2003) RadioGraphics. 23 (6): 1461-76. doi:10.1148/rg.236025174 - Pubmed
-
2. Rafailidis V, Robbie H, Konstantatou E, Huang DY, Deganello A, Sellars ME, Cantisani V, Isidori AM, Sidhu PS. Sonographic imaging of extra-testicular focal lesions: comparison of grey-scale, colour Doppler and contrast-enhanced ultrasound. (2016) Ultrasound (Leeds, England). 24 (1): 23-33. doi:10.1177/1742271X15626195 - Pubmed
-
3. Wibmer A & Vargas H. Imaging of Testicular and Scrotal Masses: The Essentials. IDKD Springer Series. 2018;:257-64. doi:10.1007/978-3-319-75019-4_24
-
4. Gabriel H, Hammond N, Marquez R et al. Gamut of Extratesticular Scrotal Masses: Anatomic Approach to Sonographic Differential Diagnosis. Radiographics. 2023;43(4):e220113. doi:10.1148/rg.220113 - Pubmed
-
5. Köckerling F & Schug-Pass C. Spermatic Cord Lipoma—A Review of the Literature. Front Surg. 2020;7:39. doi:10.3389/fsurg.2020.00039 - Pubmed
-
6. Smereczyński A, Kołaczyk K,. Differential Diagnosis of Fat-Containing Lesions in the Inguinal Canal Using Ultrasound. J Ultrason. 2019;19(78):222-7. doi:10.15557/jou.2019.0033 - Pubmed
-
7. Karbasian N, Segaran N, Solomon N et al. Pathologic Conditions at Imaging of the Spermatic Cord. Radiographics. 2022;42(3):741-58. doi:10.1148/rg.210161 - Pubmed
Promoted articles (advertising)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.