Transitional cell carcinoma (TCC) of the ureter, also called urothelial cell carcinoma (UCC) of the ureter, is uncommon compared to similar tumors elsewhere along the urinary tract but is nonetheless the most common primary tumor of the ureter.
This article concerns itself with transitional cell carcinomas of the ureters specifically. Related articles include:
general discussion: transitional cell carcinoma of the urinary tract
-
transitional cell carcinomas in other locations:
On this page:
Epidemiology
The epidemiology of transitional cell carcinomas of the renal pelvis is similar to those of the rest of the urinary tract: please refer to TCC of the urinary tract for further details.
Clinical presentation
Clinical presentation is relatively non-specific, most frequently consisting of hematuria and/or flank pain due to obstructive hydronephrosis. Clots may cause renal colic and mimic ureterolithiasis.
Pathology
Location
The ureter is the least common location for transitional cell carcinoma (TCC) of the urinary tract, 2-3 times less common than TCC of the renal pelvis, and 100 times less common than transitional cell carcinoma of the bladder. It accounts for only 1% of all upper urinary tract malignancies 1.
The distal ureter is more frequently affected, presumably due to greater stasis 3,4:
proximal third: 3%
middle third: 24%
distal third: 73%
In 2-5% of patients, bilateral tumors are found 3,4.
Macroscopic appearance
As is the case elsewhere, two main morphologic patterns are recognized:
-
papillary
account for 60% of tumors 1
multiple frond-like papillary projections
tend to be low grade and invasion beyond the mucosa is a late feature
-
non-papillary
sessile or nodular tumors
tend to be high grade with early invasion beyond the mucosa
Radiographic features
Ultrasound
Ultrasound has little role to play in the diagnosis of transitional cell carcinoma of the ureter, although it may suggest the diagnosis by diagnosing hydronephrosis.
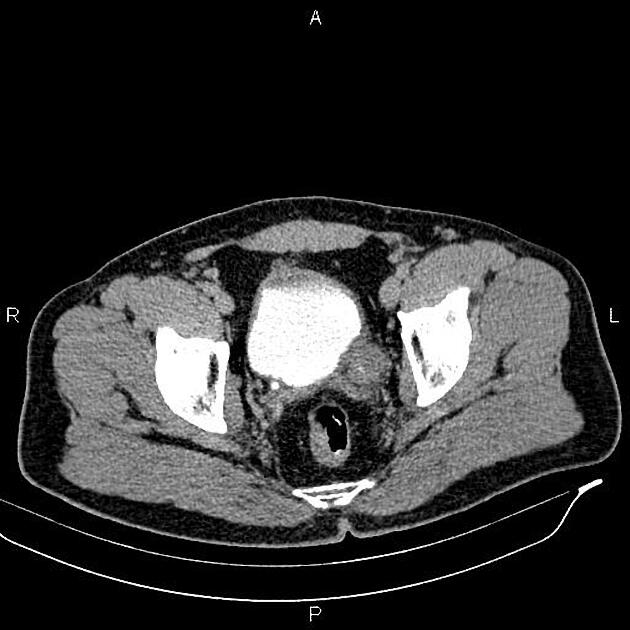
CT
Conventional CT with or without contrast medium often struggles to diagnose a small ureteral transitional cell carcinoma, as all that may be visible is focal soft tissue thickening of the ureter. If hydronephrosis and/or hydroureter are present then careful examination of the transition point for a soft tissue mass should be carried out.
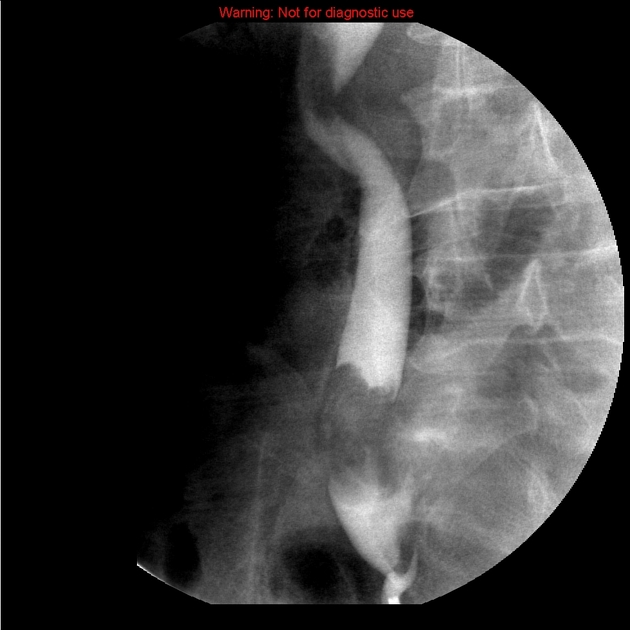
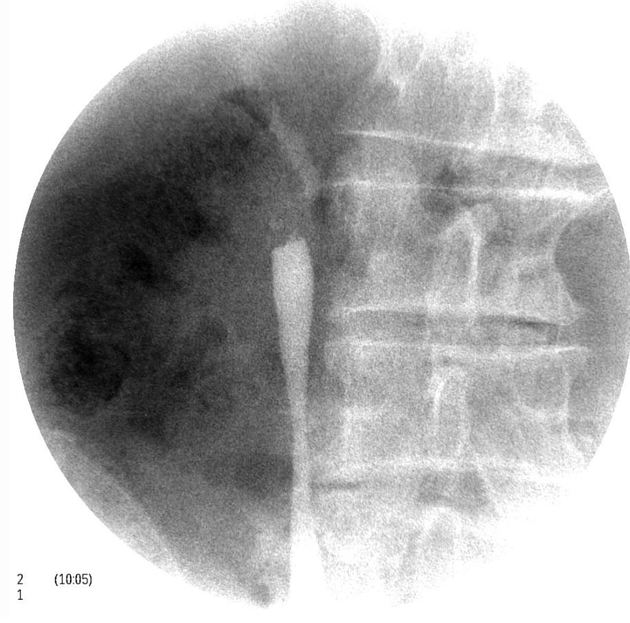
Urography/pyelography
The collecting system can be opacified by contrast medium in a number of ways:
by intravenous injection (CT IVP and conventional IVP)
-
by direct instillation of contrast into the collecting system
antegrade pyelography via a nephrostomy
retrograde pyelography via cannulation of the ureter via cystoscopy
CT urography (CT IVP) has largely replaced conventional plain film urography and is the mainstay of both diagnosis and staging (see staging of TCC of the ureter) with a sensitivity of 96% and specificity of 99% 3.
Due to the small caliber of the ureter, tumors are more likely to obstruct the kidney at a small tumor size. Obstruction may lead to hydronephrosis with or without hydroureter and may also result in a non-functioning kidney or delayed nephrogram.
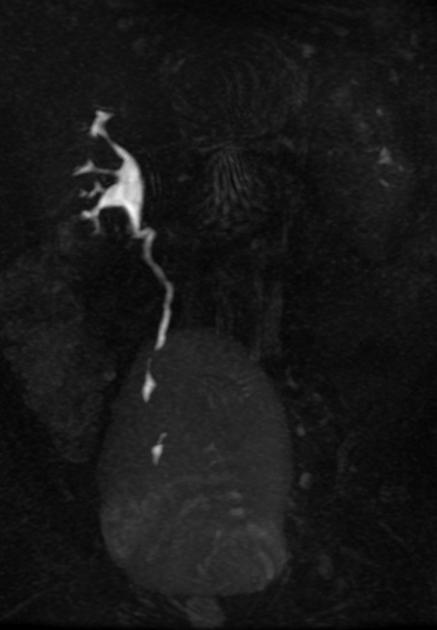
Smaller or polypoid tumors may be seen as filling defects, and if they cause partial long-standing obstruction may result in focal dilatation of the ureter at the site of the tumor. This may lead to the so-called goblet sign, best seen on retrograde ureterography 2-6.
Occasionally circumferential thickening of the ureteric wall results from diffuse infiltration and may have an apple core appearance 4.
Treatment and prognosis
Typically, and certainly, in the case of locally advanced tumors, treatment is surgical consisting of a nephroureterectomy, taking not only the kidney but also the ureter and a cuff of the bladder at the vesicoureteral junction 4,5.
In low stage tumors and especially in patients with bilateral tumors (e.g. Balkan nephropathy) or solitary kidneys, renal-sparing surgery may be attempted, in which tumors are locally excised often endoscopically (percutaneous or transurethral approach) 4,5.
Instillation of bacille Calmette-Guerin (BCG) or mitomycin C into the upper tract has been investigated as an alternative to surgery in some cases 5.
Prognosis depends on the stage of the tumor (see staging of TCC of the ureter) and histological grade (see grading of TCC) has little influence 3. Metastases are most frequently to the liver, bone, and lung 4.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.