Presentation
Known rheumatoid arthritis on treatment for approximately 15 years. A recent CXR demonstrated bilateral increased interstitial markings in the basal lung regions. Noncontrast chest CT requested to evaluate possible RA-associated interstitial lung disease.
Patient Data


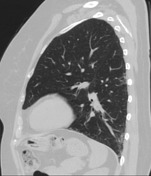
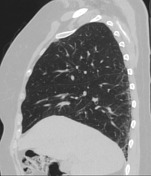

CT demonstrates a primarily peripheral, subpleural pulmonary fibrosis, which particularly affects the basal segments of the lower lobes (see representative sagittal plane images). Associated honeycombing and bronchiectasis can also be observed.
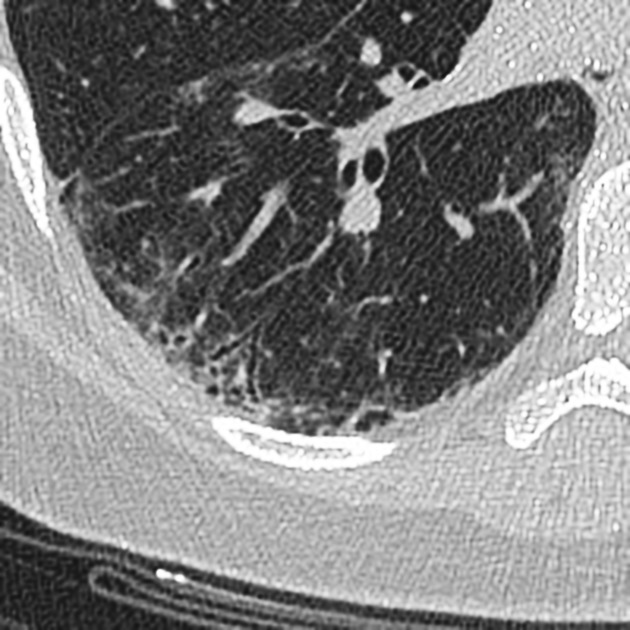
Magnified key image demonstrating bronchiectasis, subpleural reticulation and honeycombing.
Case Discussion
Altogether the findings show a distinct UIP pattern, and considering the history are in line with RA-associated ILD.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.