Presentation
Long-term history of treatment-resistant epilepsy. New episode of generalized seizure.
Patient Data
ASNR Case of the Day Winner 2021
This case was selected as the winner of the 2021 ASNR Case of the day competition winner. Runner-up and honorable mentions can be viewed in this playlist.


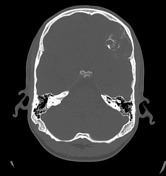

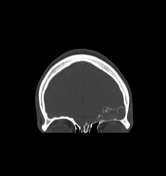

Axial non-enhanced brain CT shows a heterogeneous hyperdense lesion with peripheral calcifications in the left frontobasal region. The bone windows better demonstrates the multiple linear intralesional calcifications, resembling a “rings and arcs” pattern. The lesion causes marked bone resorption, which is evident at the orbital portion of the left frontal bone (coronal plane in bone window).
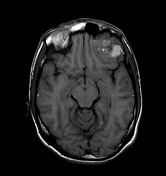

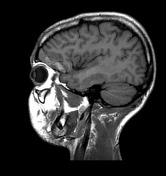

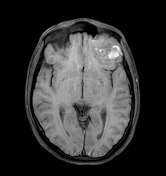



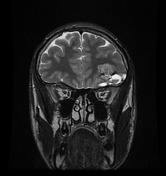

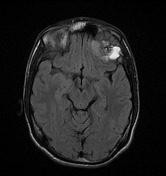

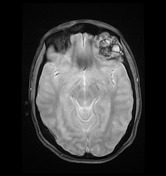

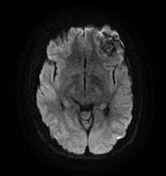

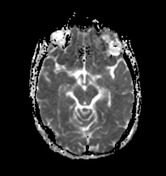



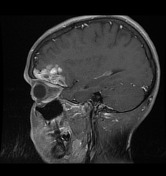

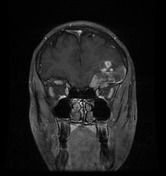

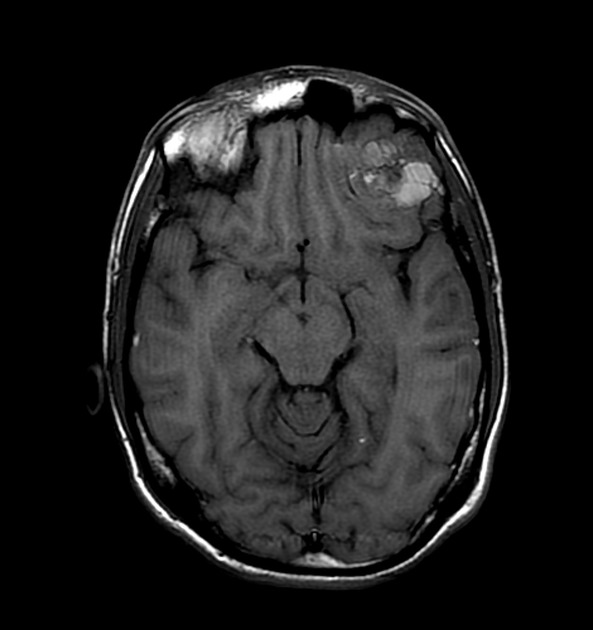
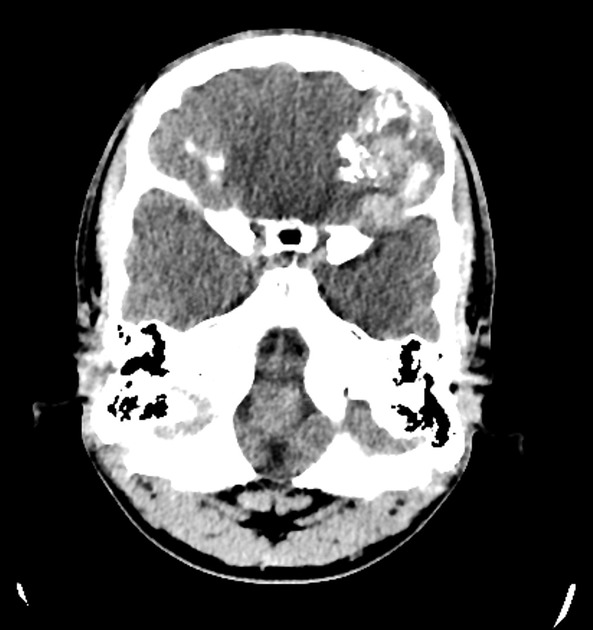
The MRI confirms the intraaxial location of the left frontobasal lesion. The T2 sequence displays both cystic and solid intralesional components, with hyperintense elements on T1 and fat-saturated sequences, resulting from subacute blood products or dense proteinaceous fluid. There is no peritumoral hyperinensity on the FLAIR images. The blooming artifacts on the GRE sequence probably correspond to calcifications, without ruling out the possibility of intralesional hemorrhages. The lesion has a heterogeneous signal on the DWI sequence, with areas of low ADC values corresponding to the cystic portions. There is vivid enhancement of the solid portions, with nodular enhancement along the lesion's inner and superior borders.
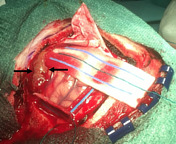

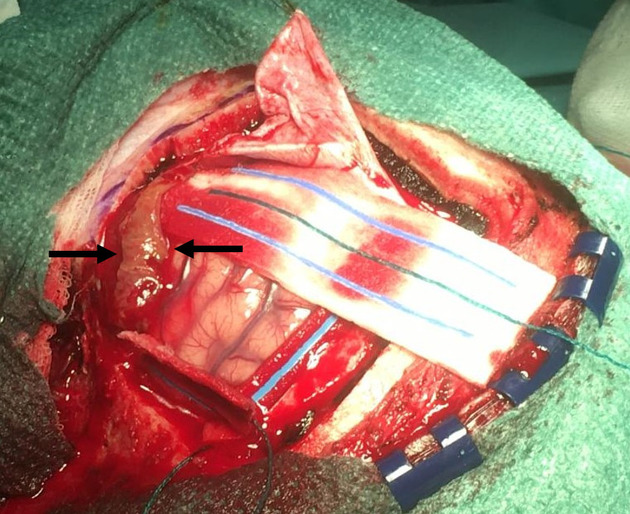
Gross pathology image shows the macroscopic appearance of the lesion (black arrows).
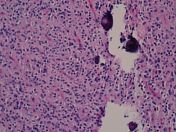
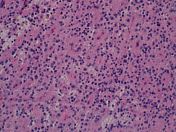
Hematoxylin-eosin (H&E) stains show multiple small round blue cells within a neuropil-like matrix, forming rosette aggregates. Some calcifications can be observed at the superior and inferior right quadrants of the second picture. There are also small disperse vessels. In the third picture, a few hemosiderin deposits can be seen at the superior left quadrant. No chondroid matrix could be appreciated.
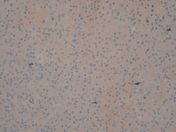
The fourth picture shows diffuse and intense synaptophysin (SYN) positivity.
The last picture demonstrates negativity for glial fibrillary acidic protein (GFAC) stain.
Inmunohystochemical analysis also revealed an absence of IDH mutations or 1p19q co-deletion.
Case Discussion
Differential diagnosis in this case would include the following entities:
Anaplastic oligodendroglioma. The principal differential diagnosis, as this lesion can also manifest with multiple calcifications, bone remodeling, and lack of perilesional edema. On the other hand, this type of neoplasm tends to have coarse and larger calcifications and it is typically encountered in middle-aged adults.
Chondrosarcoma. The presence of rings and arcs calcifications and bone destruction raised the possibility of chondrosarcoma. Also, the T2 hyperintense regions resembling the cartilaginous matrix favored this option. However, chondrosarcoma does not usually appear as an intracranial mass and is rare in young patients.
Grade III meningioma. Cystic components are less frequent in this type of lesion, and enhancement is usually more significant and homogeneous.
Gangliocytoma/ganglioglioma. Ordinarily seen in children and young adults, these tumors can have a similar clinical presentation. Nevertheless, they have a more homogeneous radiological appearance and do not show bone resorption.
Anaplastic astrocytoma/GBM. These neoplasms rarely show calcifications and bone resorption, and frequently present with marked peripheral FLAIR hyperintensity.
Metastases. Although this diagnosis should always be considered, there was no oncological history in this patient.
The patient went to have surgical resection of the lesion. No chondroid matrix was found, therefore chondrosarcoma was ruled out. There were also no IDH mutations, 1p19q co-deletion, or glial cells to consider an oligodendroglioma. Finally, the histologic appearance together with the synaptophysin positivity was in keeping with an extraventricular neurocytoma. The T1 hyperintense components could be explained either by blood products, dense proteinaceous fluid, or areas of microcalcification.
Extraventricular neurocytomas are extremely rare WHO grade II primary CNS neoplasms, only described in a few case reports. They can have significant overlap in radiologic presentation with other primary brain tumors; consequently, it is difficult to make an accurate preoperative diagnosis.
Acknowledgments to Dra. Celia Lizi Oramas Requejo and Hospital de Palamós for providing the radiological images, to Dr. Pablo Benito Peña for sharing the macroscopic picture, to Dra. Laura Ferrazza Martín for contributing with the microscopic images, and to Dr. Nerses Nersesyan for his broad knowledge and incredible support.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.