Anterior cervical discectomy and fusion (ACDF) is a commonly performed spinal fusion procedure for the decompression of the cervical cord due to disc protrusions and posteriorly projecting osteophytes.
It is not to be confused with an ACDA (anterior cervical disc arthroplasty).
On this page:
Indications
Anterior cervical discectomy and fusion are generally indicated in patients with spondylosis or disc herniation of the cervical spine with myelopathy/radiculopathy that is unresponsive to conservative therapy. Furthermore, it may also be indicated in certain malignant, traumatic, or infective processes of the cervical vertebrae which result in instability 5,6.
Contraindications
A relative contraindication to anterior cervical discectomy and fusion are anatomical variants of the vertebral artery 6.
Procedure
Positioning
Patients are placed in a supine position with the neck in a neutral position 5.
Technique
The procedure is carried out via an anterolateral neck incision with a surgical approach passing between the aerodigestive tract (trachea, esophagus, pharyngeal muscles) medially and the carotid neurovascular bundle (carotid artery, internal jugular vein, vagus nerve) laterally 2.
The intervertebral disc is then resected along with the fibrocartilage covering the adjacent vertebral endplates (to allow for eventual osseous fusion). It is possible to reach back to the posterior longitudinal ligament, removing osteophytes and disc protrusion as well as extending laterally to decompress the neural exit foramina 1,2.
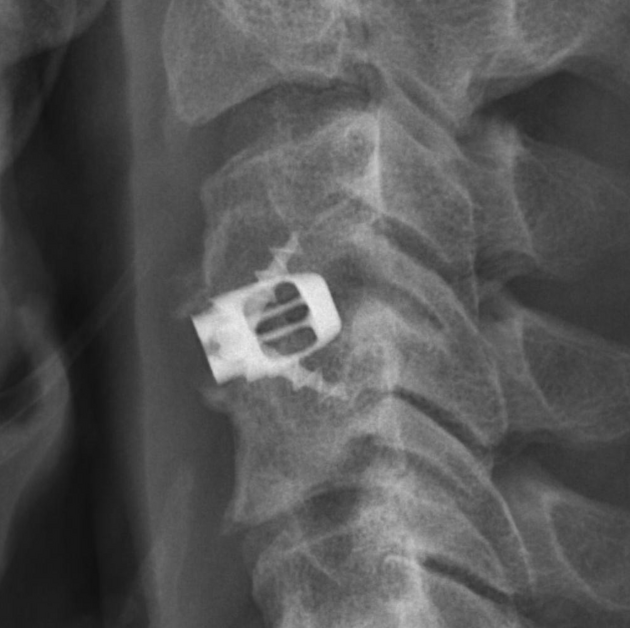
Once decompression has taken place an interbody spacer (or "cage") of some kind is introduced to assist fusion/improve stability. This can be in the form of 1,3:
-
bone
autogenous bone graft (e.g. from the anterior iliac crest of the patient harvested at the same time as the fusion is performed)
allogeneic bone graft (e.g. from cadaveric iliac bone or fibula)
animal allogeneic bone graft (e.g. bovine or calf)
-
synthetic usually packed with cancellous autobone, demineralized bone matrix or ceramics
plastic
metal (e.g. titanium or stainless steel)
ceramic
Following this, an anterior cervical plate with screws that pass into the vertebral bodies above and below the operative segment is usually introduced to provide additional stabilization 1.
Newer devices combine screw fixation and interbody spaced into one device, fitting entirely within the interbody space without the added bulk of the anterior plate 1.
Follow-up
A common way to follow up anterior cervical discectomy and fusion is the lateral cervical radiograph to assess for prevertebral soft tissue swelling. One series 4 demonstrates that soft tissue thickness at mid-C3 and C6 levels returned to baseline at the 3 months at C3 and 6 months at C6.
Anterior cervical plate alignment can be defined as "misaligned" when shifted ≥5 mm and/or angulated 20° from the midline 8.
Assessing height loss (defined ≥3 mm intervertebral disc space or total vertical height of the fused segments compared to the most recent follow-up imaging 9,10) can indicate cage subsidence, which is axial migration into the endplates 3.
Complications
Although anterior cervical discectomy and fusion are generally safe several complications can be encountered including:
-
intraoperative complications 3
vascular injury, e.g. to the carotid artery or internal jugular vein
dural tear
-
early post-operative complications
dysphagia due to plate and screws (most common) 3,11
infection
-
airway compromise (~15%) 11
from angioedema (6-12 hours), retropharyngeal hematoma (6-24 hours), pharyngolaryngeal edema (24-72 hours), and/or retropharyngeal abscess (>72 hours) 11
re-intubation required in ~3.5% (2-5%) 11
hematoma (~2.5%) 11
hoarse voice due to damage to the recurrent laryngeal nerve 3
-
late post-operative complications
non-union: lack of osseous bridging at 6 months post-operation 3
cage subsidence (~20%): can result in decreased intervertebral foraminal volume (and potentially radiculopathy), cervical spinal instability leading to adjacent segment degeneration, and/or pseudarthrosis 3,9,10
-
hardware loosening
osteolysis with PEEK cages 3
hardware failure, e.g. screw fracture 3
kyphotic cervical spine malalignment 9
adjacent segment degeneration (~50%) 3
Outcomes
Anterior cervical discectomy and fusion are associated with improvements in morbidity with one study reporting that 85% of patients self-reported that treatment had been successful at ~10-year follow-up 7.
Misaligned anterior cervical plates have increased torsional strength and have better earlier postoperative outcomes, however, no difference in outcome exists after fusion and there is no difference in hardware failure (e.g. backed-out screws) between straight and misaligned plates 8.
The effect of cage subsidence on clinical outcomes is unclear (c. 2018) 9.














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.