Chronic osteomyelitis is a form of osteomyelitis that is defined as a progressive inflammatory process resulting in bone destruction and sequestrum formation. Bacteria and fungi can cause it, and it may present as recurrent or intermittent disease.
On this page:
Terminology
Chronic osteomyelitis is where symptoms are present for >4 weeks, whereas acute osteomyelitis is where symptoms are present for <2 weeks 6.
Pathology
Chronic osteomyelitis results from osteonecrosis caused by disruption of intraosseous and periosteal blood supply during the acute stage of the disease. A dead infected bone fragment separates from viable bone (bony sequestrum). Infective agents within the devascularised sequestrum become protected from antibiotics and the endogenous immune response, forming a nidus for chronic infection. This may persist for years. It is characterized by increased inflammatory neutrophils, plasma cells, and lymphocytes.
Radiographic features
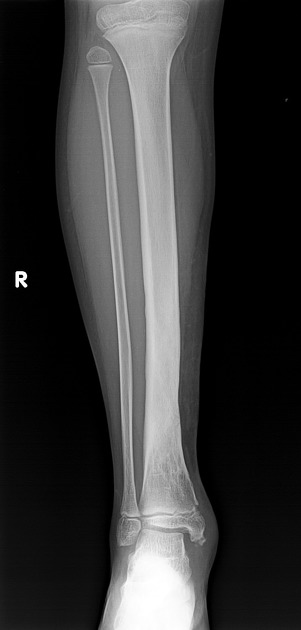
Plain radiograph
Inhomogeneous osteosclerosis and/or sequestrum formation (necrotic bone) is characteristic of chronic osteomyelitis on x-ray ref.
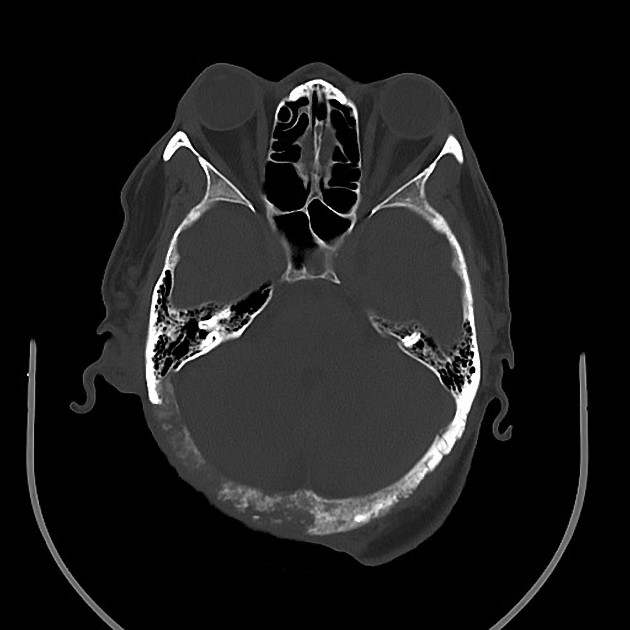
CT
CT may provide information regarding the presence of sequestra, cloaca, cortical destruction and/remodeling, and the thickness of the involucrum 6.
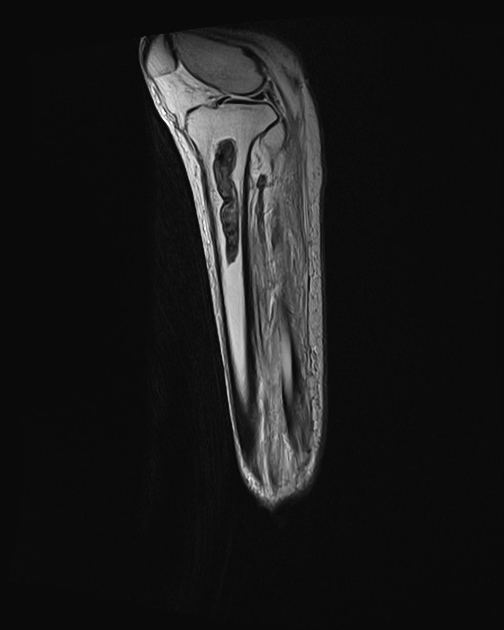
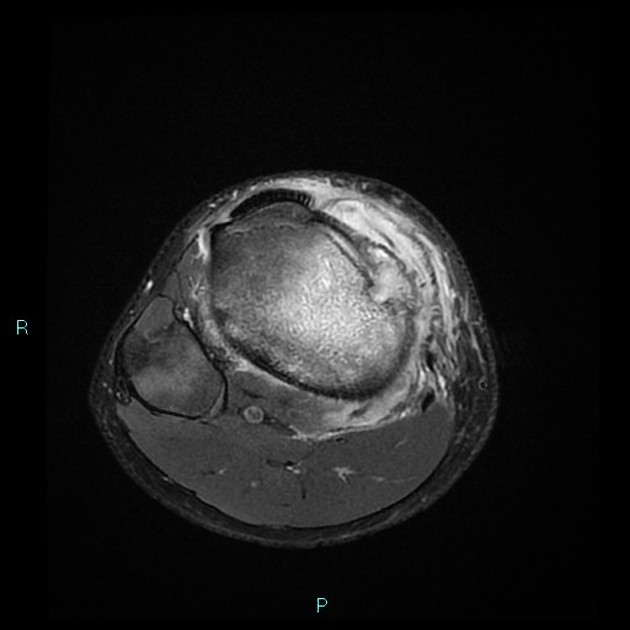
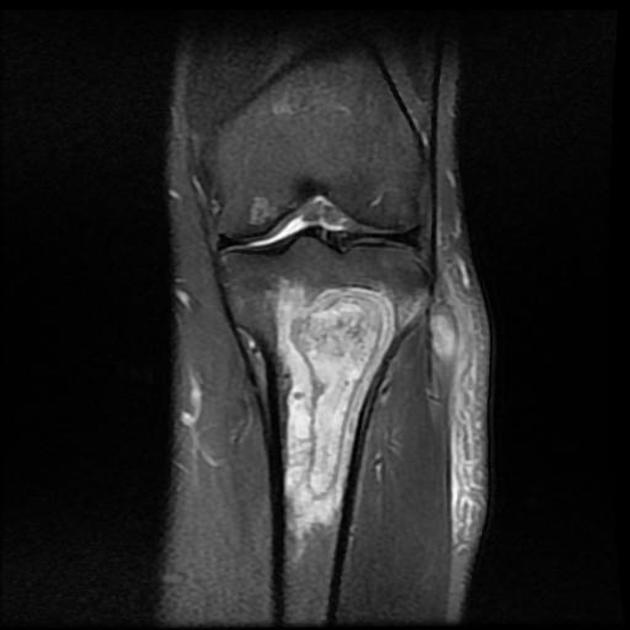
MRI
Chronic osteomyelitis consists of region of active infection and fibrosis resulting in heterogeneous signal characteristics 6. Other radiographics features mentioned above may also be present.
Signal characteristics
T1: low signal (both active infection and infection) 6
T2/T2FS/PDFS: mixed high signal (active infection) and low signal (fibrosis) 6


















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.