An ectopic posterior pituitary reflects a disruption of normal embryogenesis of the posterior pituitary and is one of the more common causes of pituitary dwarfism. Although it can be an isolated abnormality, numerous other congenital central nervous system malformations have been identified. When associated with a thin or absent infundibulum and hypoplastic or aplastic anterior pituitary gland, the term pituitary stalk interruption syndrome is used.
On this page:
Epidemiology
Ectopic posterior pituitary is a congenital abnormality due to faulty embryogenesis (see below).
Clinical presentation
Patients with ectopic posterior pituitary glands often present with features of growth hormone deficiency (pituitary dwarfism). Hyperprolactinemia has also been described 6 presumably as a result of lack of tonic inhibition by hypothalamic dopamine (see elevated prolactin differential diagnosis). In the neonatal period, hypoglycemia is also common 1.
Additional features referable any one of numerous associated malformations may also be identified, including 1,3:
-
central nervous system
microcephaly / cerebellar atrophy
-
facial abnormalities
single central incisor tooth
cardiac abnormalities
musculoskeletal abnormalities
Pathology
The clear underlying etiology of an ectopic posterior pituitary has not been established although reports suggest that it may share similar pathogenesis as septo-optic dysplasia 1,2. The HESX1 gene has been implicated in both conditions 1. Regardless of the underlying cause, an ectopic posterior pituitary results from the incomplete downward extension of the diencephalon (infundibulum). As a result, factors released by the hypothalamus which usually travels down the portal circulation to the anterior pituitary can only reach their target via the general circulation. This results in frequent growth hormone deficiency, and in some instances panhypopituitarism 5.
For more details on the development of the pituitary please refer to the pituitary gland article.
Radiographic features
MRI
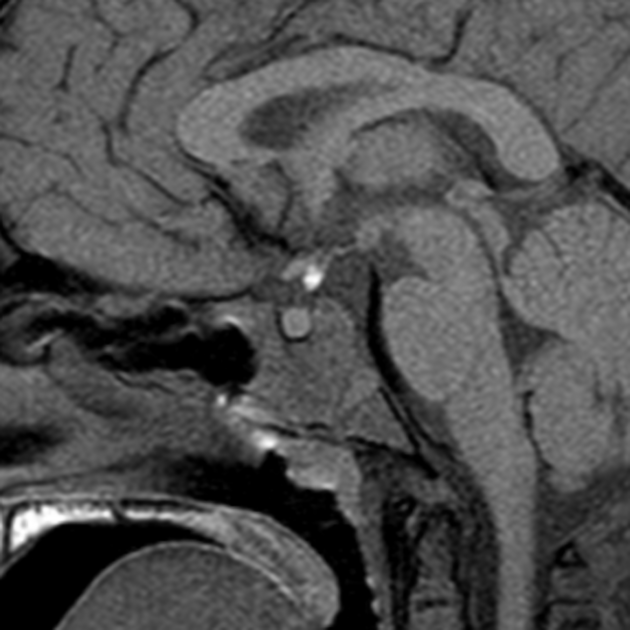
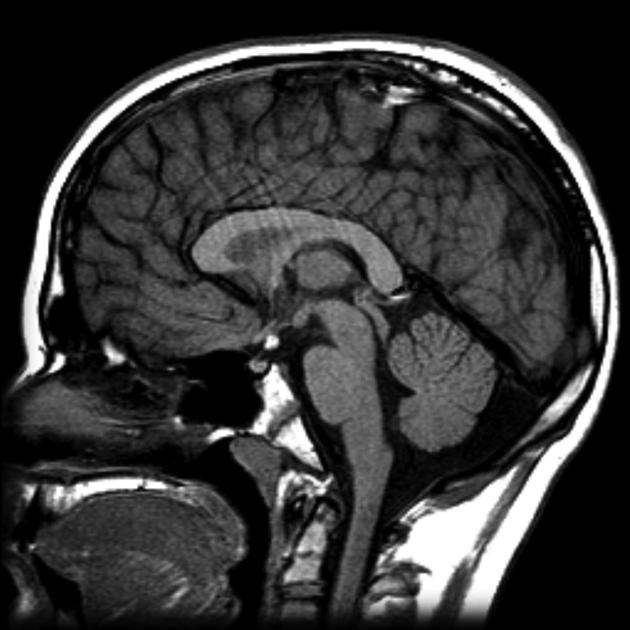
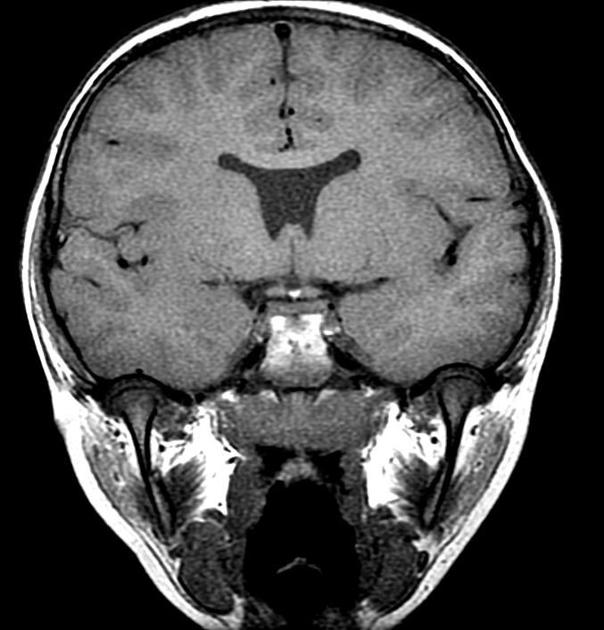
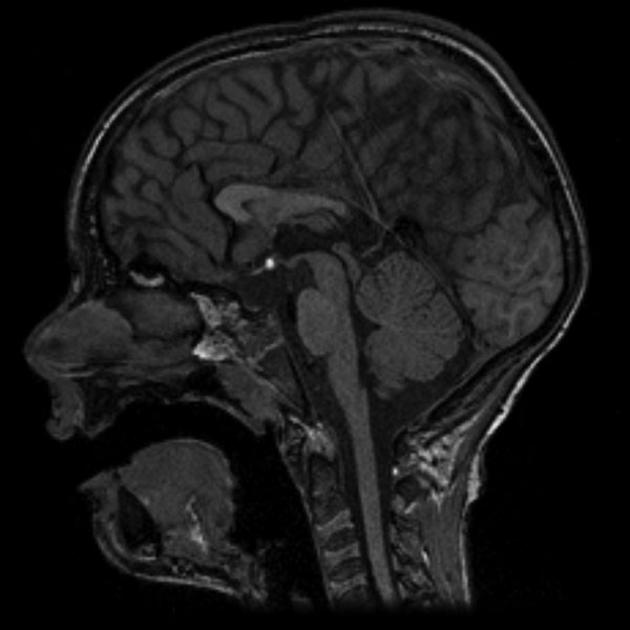
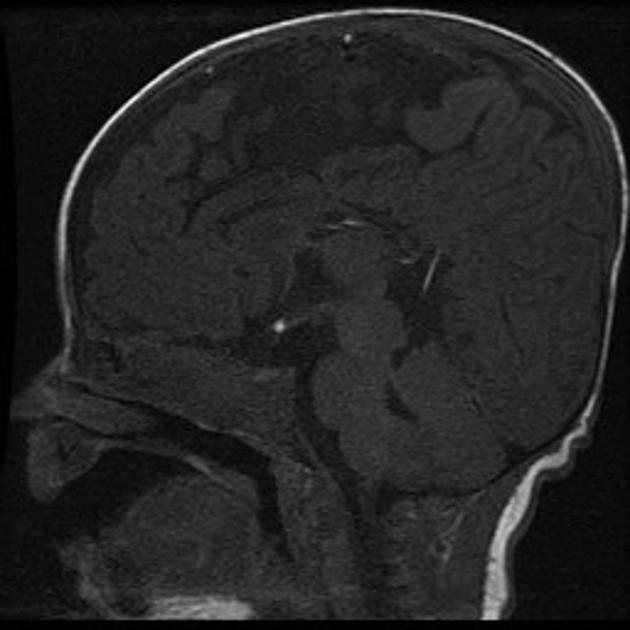
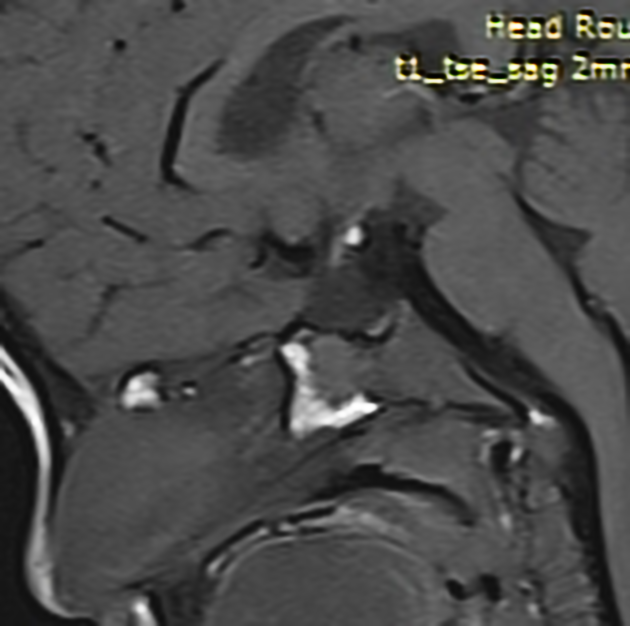
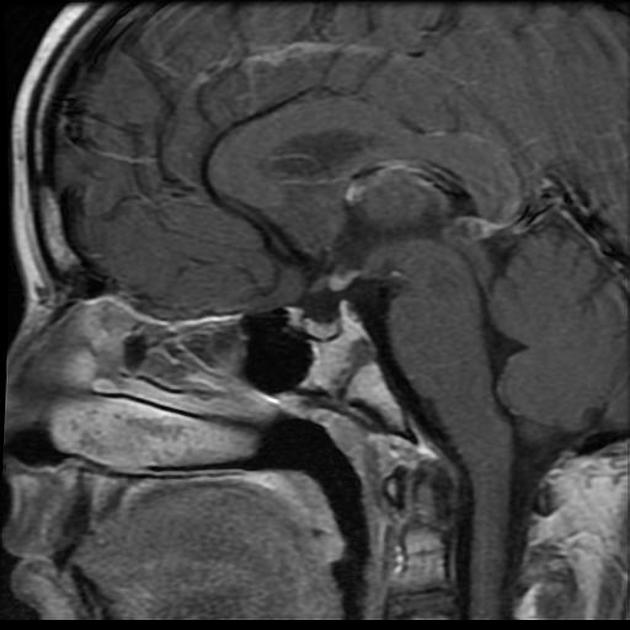
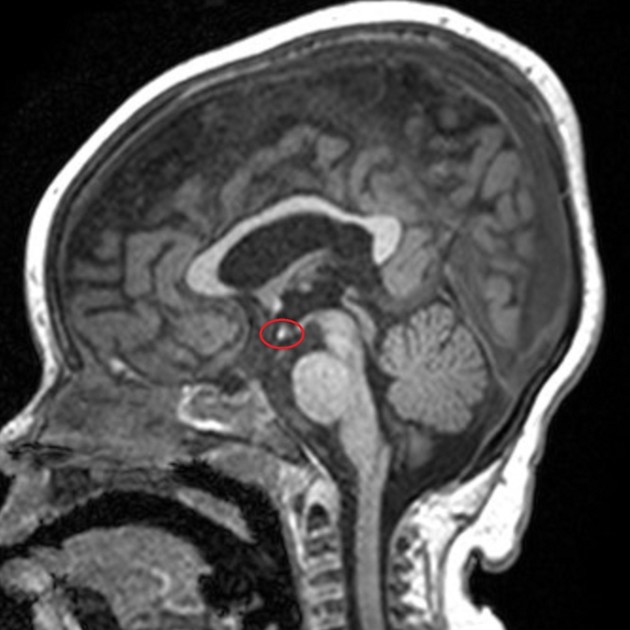
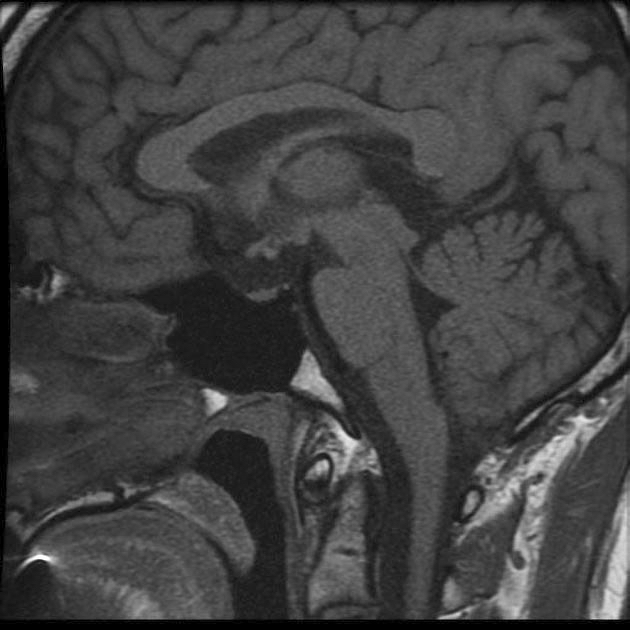
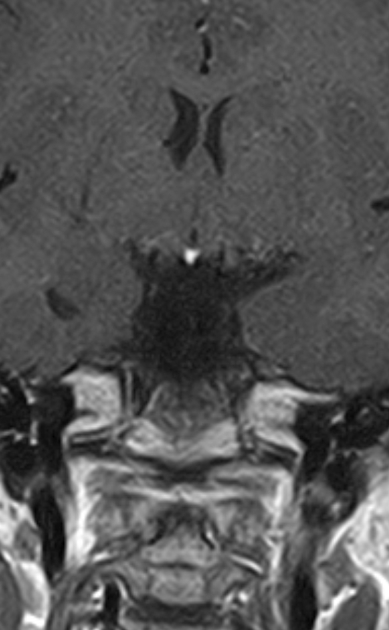
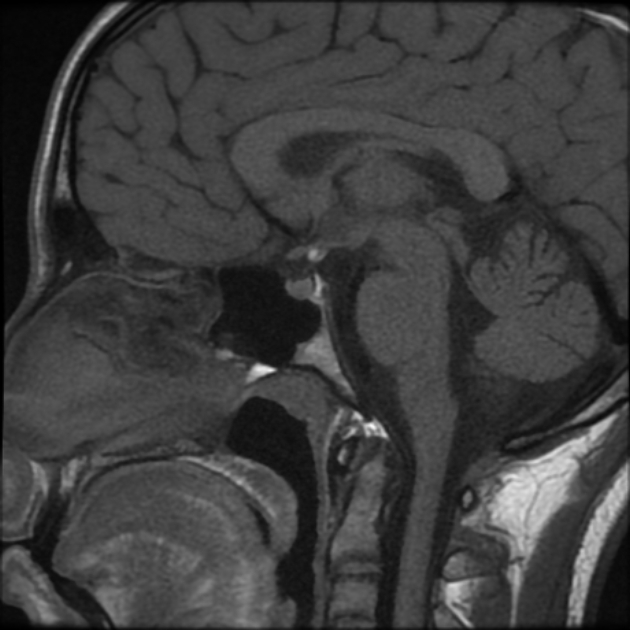
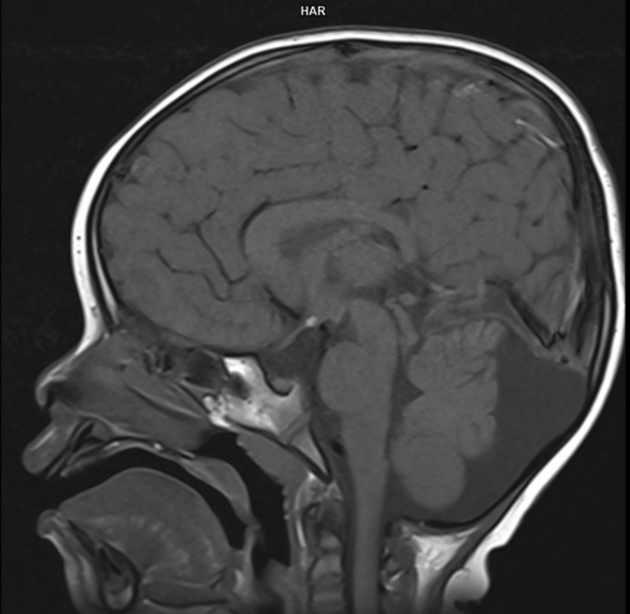
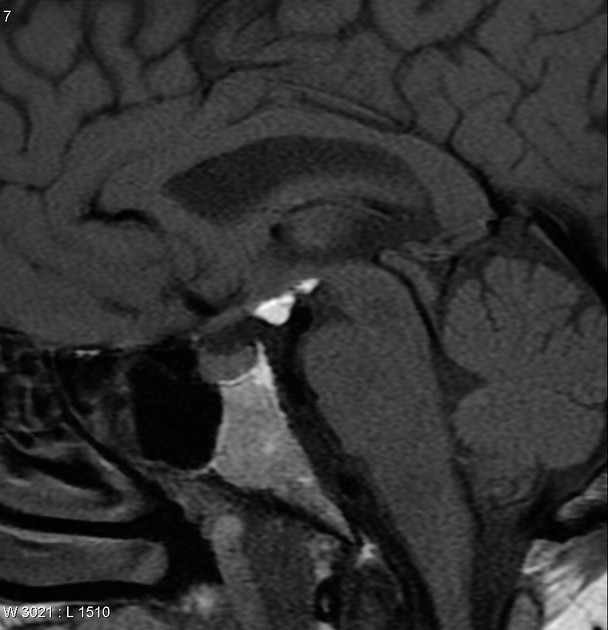
MRI is the only modality adequately able to identify ectopic posterior pituitary. The diagnosis is best made on sagittal midline T1 images, and features consists of 3:
high T1 signal 3-8 mm tissue nodule at the median eminence (floor of the third ventricle)
Very rarely a double pituitary bright spot may be seen, with both an ectopic and an orthotopic component 7.
The exact cause of high T1 signal is uncertain and may relate to neurosecretory granules or high lipid content of the posterior pituitary tissue 3.
As numerous abnormalities have been associated with ectopic posterior pituitary glands, a careful survey of the rest of the intracranial contents should be performed.
Treatment and prognosis
No treatment is required for the ectopic pituitary per se, but rather for the frequently associated growth hormone deficiency, or less frequently panhypopituitarism 5. Growth hormone replacement is available in selected patients and can improve adult height.
Differential diagnosis
The differential for an ectopic posterior pituitary is limited and essentially boils down to a subset of pituitary region mass with intrinsic high T1 signal. Possibilities include:
-
fat, e.g. lipoma, dermoid or teratoma
fat saturation sequence or chemical shift can distinguish these from the posterior pituitary
-
craniopharyngioma (usually adamantinomatous type)
usually larger
90% will have calcification
thrombosed aneurysm





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.