Chemical shift artifact or misregistration is a type of MRI artifact. It is a common finding on some MRI sequences and used in magnetic resonance spectroscopy (MRS). This artifact occurs in the frequency-encoding direction and is due to spatial misregistration of fat and water molecules.
Chemical shift is due to the differences between resonance frequencies of fat and water. It occurs in the frequency-encode direction where a shift in the detected anatomy occurs because fat resonates at a slightly lower frequency than water. Essentially it is due to the effect of the electron cloud to a greater or lesser degree shielding the nucleus from the external static magnetic field (Bo). Oxygen atoms in water molecules attract electron clouds and reduce electron clouds around hydrogen atoms while no significant such effect occurs in hydrogen atom of fat. The lesser the electron cloud, the higher the effect of static magnetic field, so higher the precession frequency. So precession frequency is higher in hydrogen atoms in water compared to hydrogen in fat.
The Larmor frequency which determines the frequency at which a particular nucleus resonates is established at the nucleus, and therefore different tissues will have slightly different Larmor frequencies depending on their chemical composition.
A chemical shift artifact can occur in the slice select direction for an analogous reason to the frequency encoded artifact. Since the slice position depends on the frequency of the spins, the "fat image" is shifted compared to the "water image". The slice thickness is larger than the shift of the water and fat images making it difficult to detect the effect on routine imaging 2.
The amount of chemical shift is often expressed in arbitrary units known as parts per million (ppm) of the main magnetic field strength. Its value is always independent of the main field strength and equals 3.5 ppm for fat and water; however, the precessional frequency is proportional to the main magnetic field strength Bo. For example, at 1.5 T the difference in precessional frequency is 224 Hz. That is, fat precesses 224 Hz less than water. At 1.0 T this difference is 147 Hz. At lower field strengths (0.5 T or less), it is usually insignificant.
In MR spectroscopy the shift in Larmor frequency allows separation of different chemical peaks. The actual amount of chemical shift as an absolute value is difficult to measure, so instead, it is represented relative to a reference and expressed in parts per million (ppm).
Subtypes
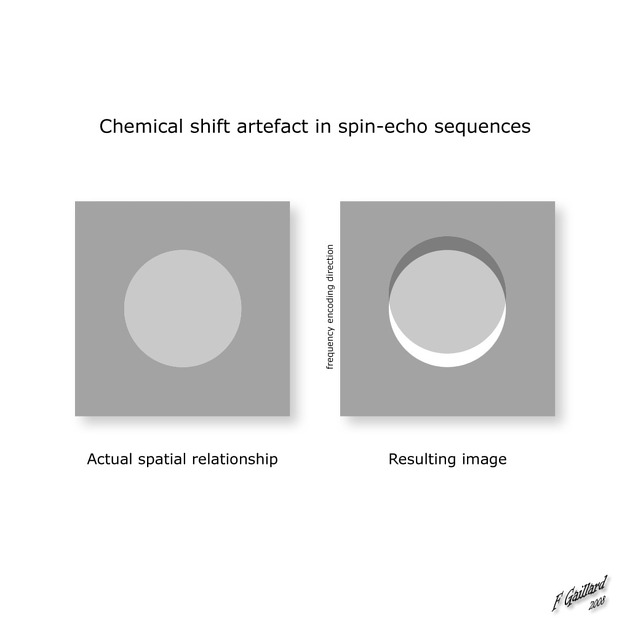
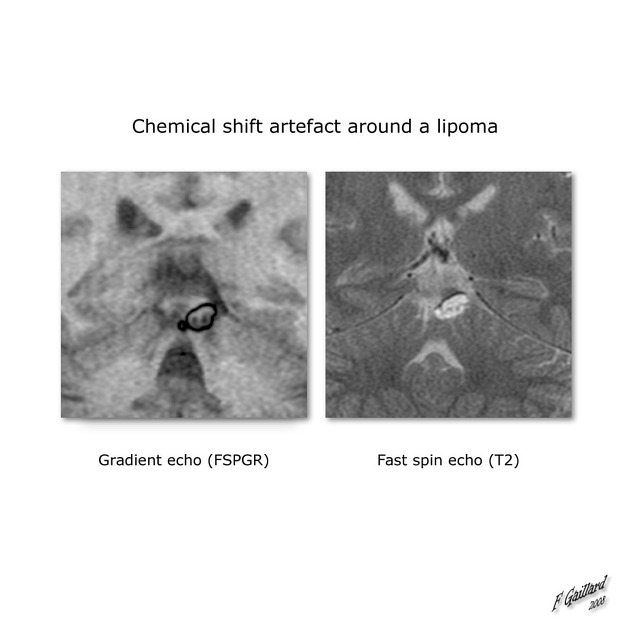
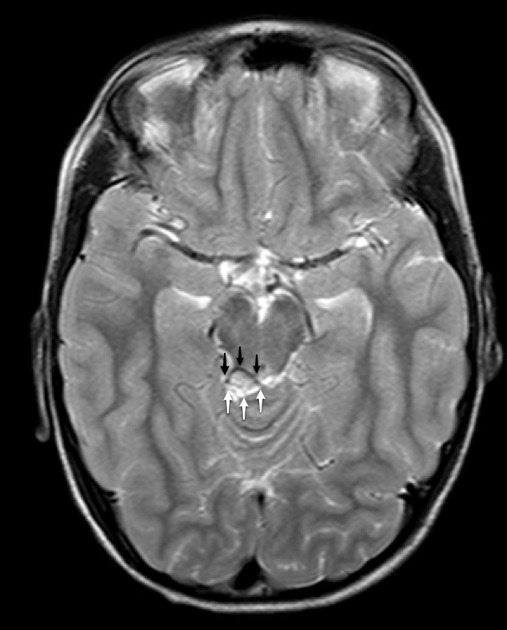
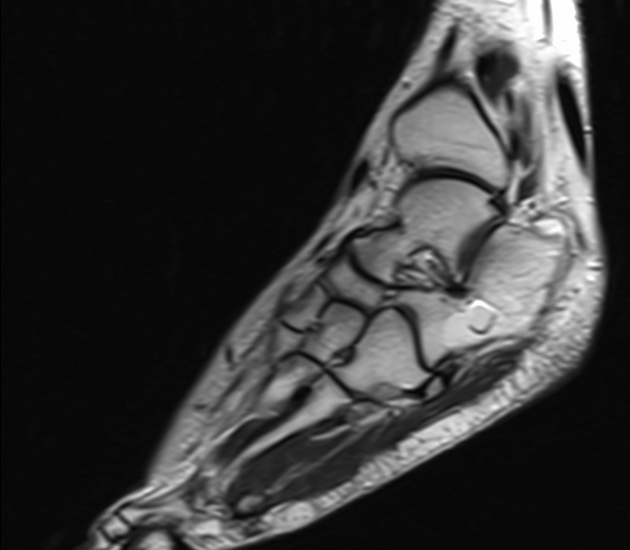
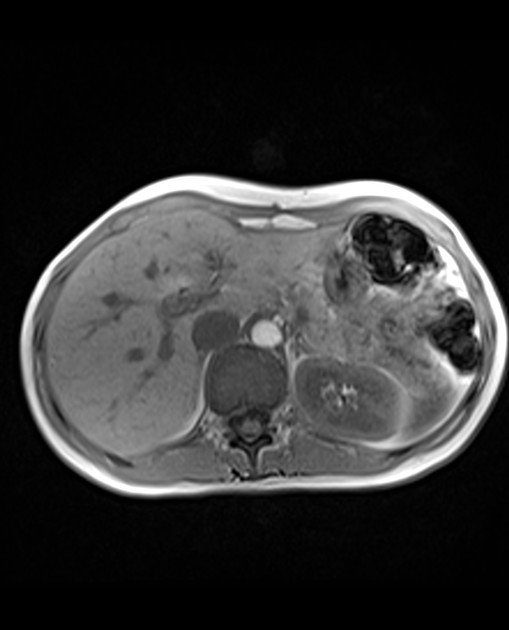
On MRI, both spin echo sequences (SE) and gradient echo sequences (GE) may demonstrate chemical shift misregistration or mismapping (type 1 chemical shift artifact). The mismapping will occur in the frequency-encoding direction and show up as a bright band on one side and a dark band on the other side of a fat-soft tissue interface.
In addition to mismapping, GE sequences can show another type of chemical shift induced artifact known as the black boundary or India ink artifact (type 2 chemical shift artifact). The artifact causes a black line in all directions at fat-water interfaces. In pixels with roughly equal amounts of fat and water, the fat and water spins are 180o out of phase at certain echo times because of their chemical shift or frequency difference causing cancelation of signal.
These effects can be used to confirm, for example, the presence of intracellular fat in a lesion.
Remedy
chemical shift increases with magnetic field strength
chemical shift increases with decreasing gradient strength
chemical shift artifact depends upon the bandwidth; the narrower the bandwidth, the higher the chemical shift; increasing the bandwidth will decrease the artifact
fat suppressed imaging can be used to eliminate the chemical shift misregistration and the black boundary artifact
use of a spin echo sequence instead of a gradient echo can eliminate the black boundary artifact but not chemical shift misregistration






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.