Encephalocele, also known as meningoencephalocele, is a form of neural tube defect and a type of cephalocele where brain tissue and overlying meninges herniate out through a defect in the cranium.
On this page:
Terminology
Although the terms encephalocele and meningoencephalocele are often used interchangeably, strictly speaking there is a distinction; meningoencephalocele specifically indicates that both brain tissue (encephalo-) and meninges (meningo-) are involved in the protrusion, whereas encephalocele merely indicates the presence of brain tissue in the protrusion without specifying the involvement of meninges, and thus can include brain tissue alone or brain tissue with meninges.
Having said that, since cranial meninges include dura mater, arachnoid mater and pia mater it can be argued that all encephaloceles also contain some meningeal elements even if the dura mater is deficient. As such for the sake of expediency the term encephalocele is usually favored if brain tissue is involved.
Furthermore, encephaloceles should be distinguished from extracranial brain herniation in which brain tissue herniates through a dural and skull defect (e.g. post-trauma or surgery).
Epidemiology
They are thought to occur in one of every 4000 live births. Frontoethmoidal encephaloceles are more common in the south and south-east Asian populations. There is no recognized gender predilection.
Associations
Occipital encephaloceles may be associated with a number of additional abnormalities:
Clinical presentation
Frontoethmoidal encephaloceles manifest as a clinically visible mass along with the nose. The intracranial root of most frontoethmoidal encephaloceles lies at the foramen cecum, a small ostium located at the bottom of a small depression anterior to the crista galli and formed by the closure of the frontal and ethmoid bones.
Basal encephaloceles are internal and are not generally externally visible, although they may manifest as a lump or bump in the oropharynx or nasopharynx.
Small temporal encephaloceles are increasingly recognized as causes of refractory epilepsy in some individuals 10 and are also encountered as asymptomatic sequelae of idiopathic intracranial hypertension.
Importantly, base of skull encephaloceles with CSF leak rarely, if ever, present with signs and symptoms of intracranial hypotension 14,15.
Pathology
Encephaloceles, when congenital (most common) are a form of neural tube defect and occur due to a failure of fusion during embryogenesis of the cartilaginous neurocranium, the membranous neurocranium or viscerocranium 6.
In adults, encephaloceles are mainly due to traumatic or iatrogenic causes but are also increasingly recognized in idiopathic intracranial hypertension.
Classification
Numerous classification systems exist for encephaloceles, many of which are only of subspecialty interest, and most use very similar terminology, sometimes with different meanings 7. As a result reading about this topic can be frustrating. The term nasal encephalocele is, for example, variably used, often to encompass both frontoethmoidal and basal encephaloceles 8.
The most popular classification (c.2023) 13 was published by Suwanwela and Suwanwela in 1972, which divides the encephaloceles according to location 4:
occipital encephalocele: ~75% of cases
-
sincipital
-
nasoethmoidal
nasofrontal
naso-orbital
interfrontal encephalocele
associated with craniofacial clefts
-
-
convexity
-
basal encephalocele: ~10% 9
sphenoidal encephalocele and variants thereof e.g. sphenoethmoidal or frontosphenoidal or spheno-orbital, etc.
Specific types
Genetics
Most cases tend to be sporadic.
Radiographic features
Ultrasound
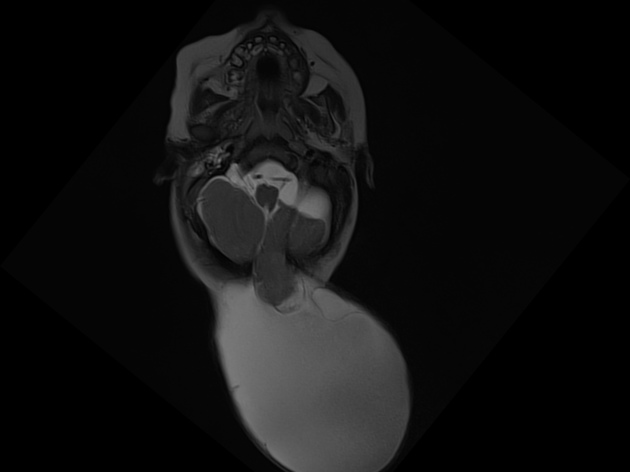
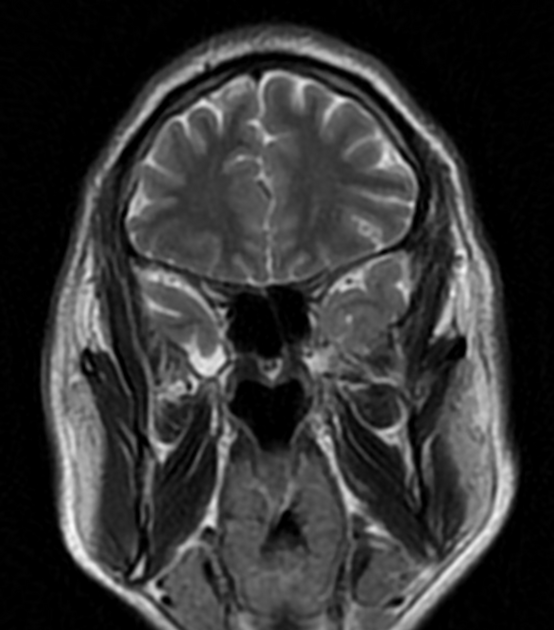
An encephalocele may be seen as a purely cystic mass or may contain echoes from herniated brain tissue. If the mass appears cystic, the meningocele component predominates, while a solid mass indicates predominantly an encephalocele. Larger encephaloceles may show accompanying microcephaly.
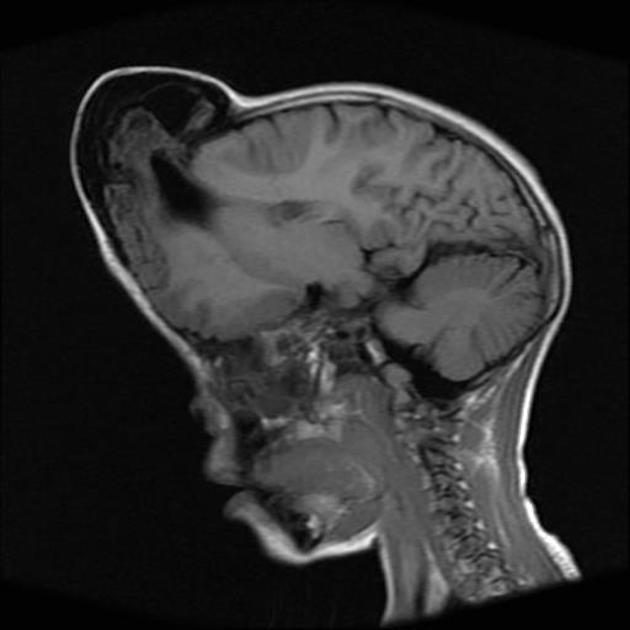
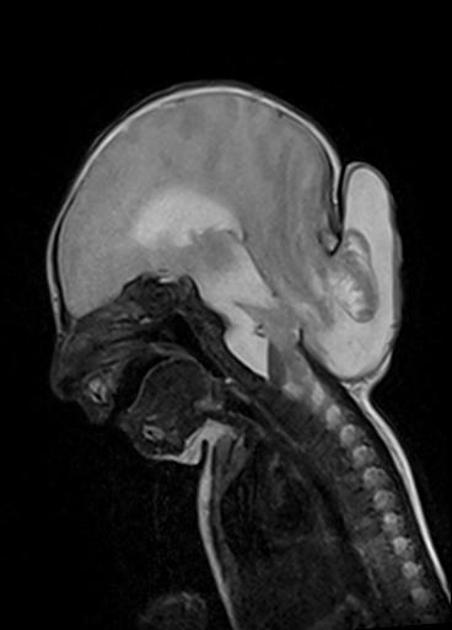
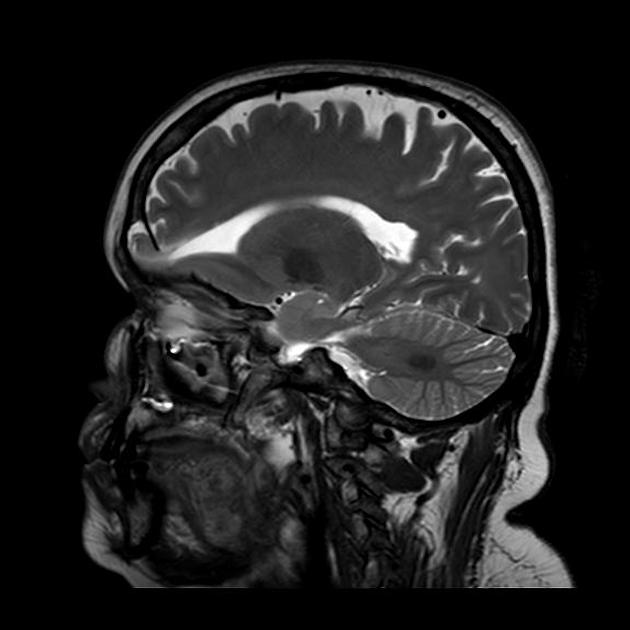
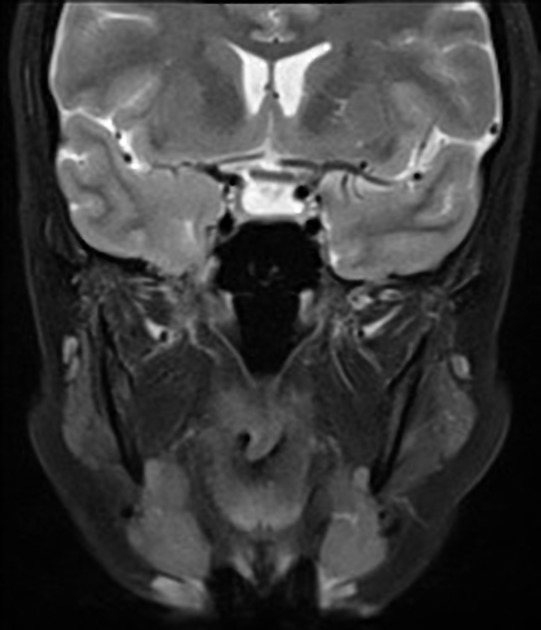
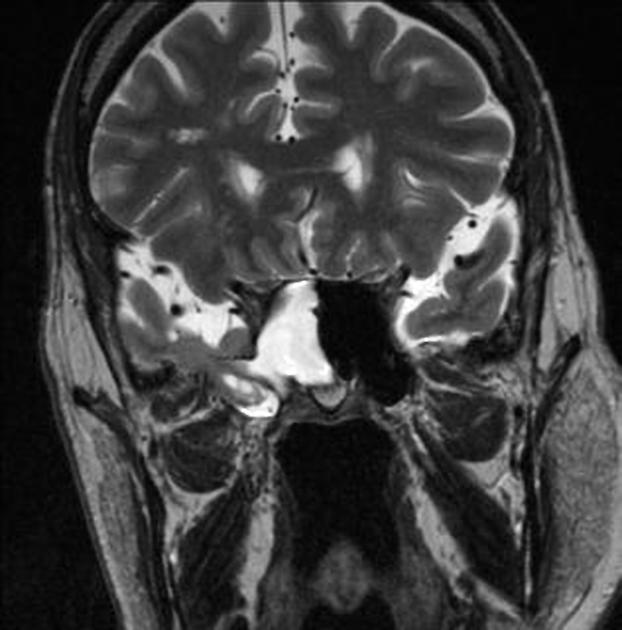
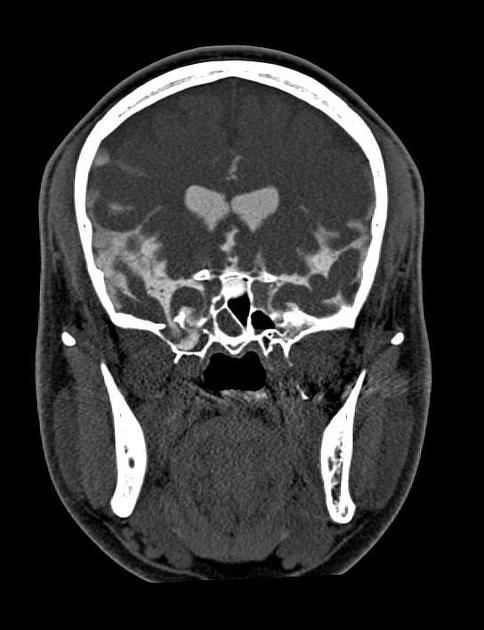
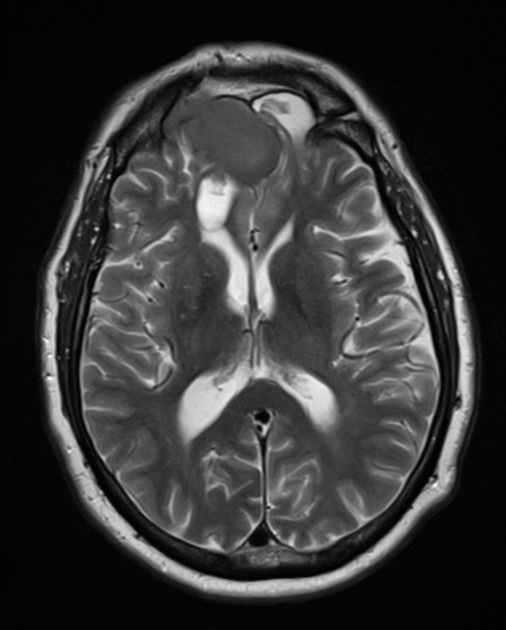
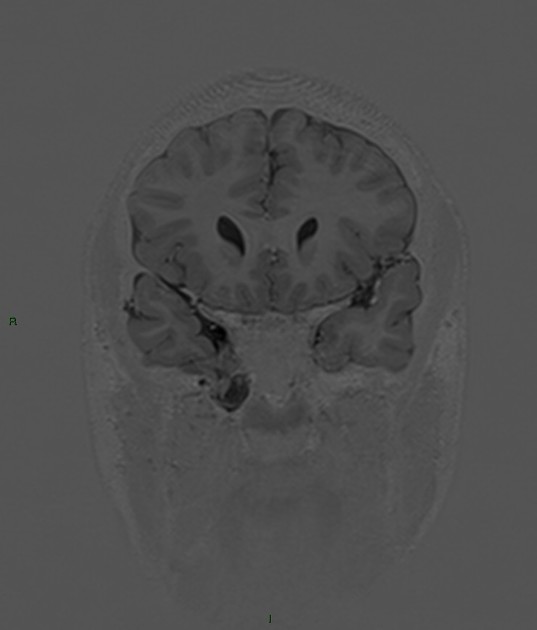
CT/MRI
MR imaging is the best imaging modality for defining the contents of an encephalocele prior to surgery. High-resolution CT may also be used to display the bone anatomy, but the intracranial connection is best defined with MR imaging. The extent of cerebral tissue in an encephalocele is also better defined with MR imaging, which aids in prognosis and surgical planning. In some instances, focal herniation of brain parenchyma occurs into an arachnoid granulation protruding into a dural venous sinus 11,12. The cause and effect, however, is unclear and controversial.
Treatment and prognosis
The prognosis is variable depending on the presence of associated anomalies and the presence of microcephaly (carries a much poorer prognosis). A cesarean delivery may be considered to allow for less traumatic birth for the fetal head.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.