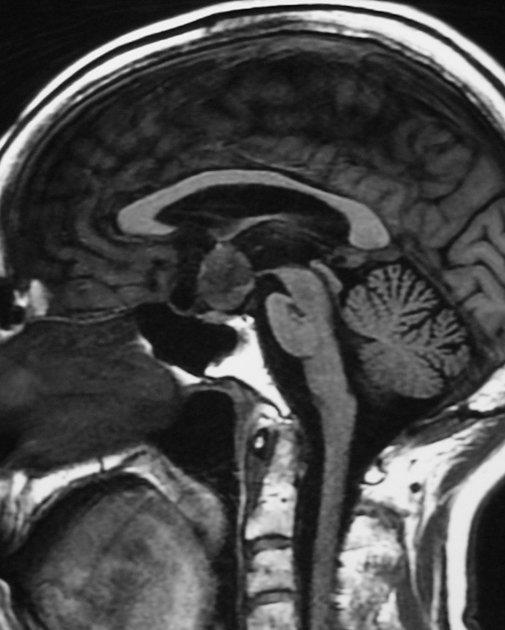
Gangliogliomas are uncommon, usually low-grade, CNS tumors. They are considered long-term epilepsy-associated tumors (LEATs) with medically refractory epilepsy being a common clinical presentation. This tumor has a predilection for the temporal lobes, although they have been described in all parts of the central nervous system.
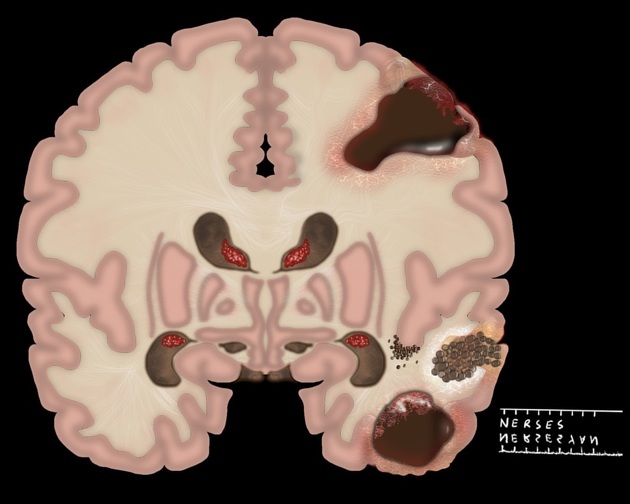
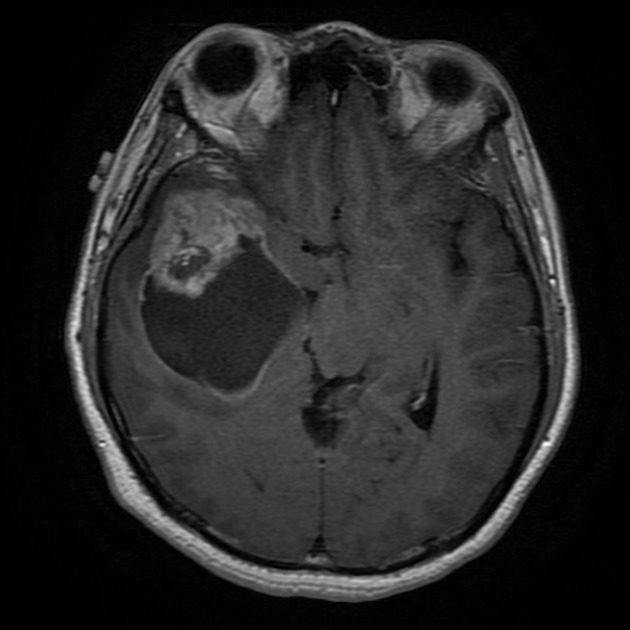
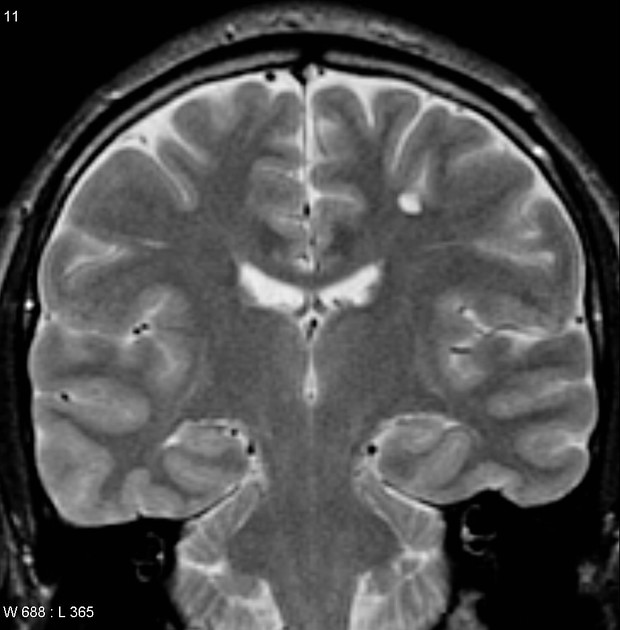
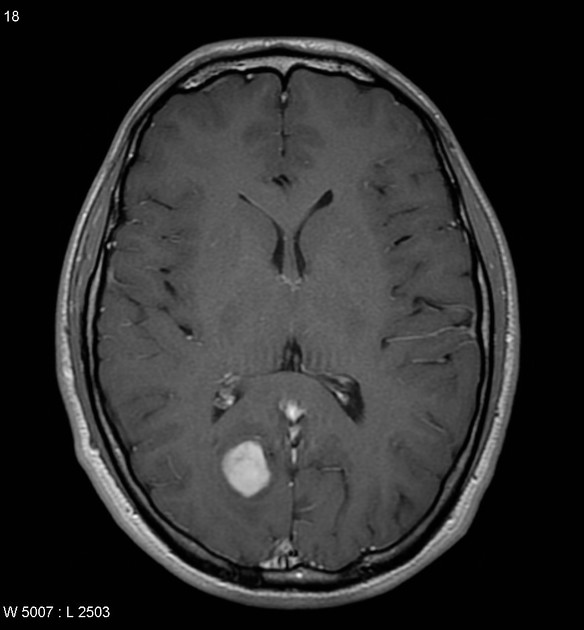
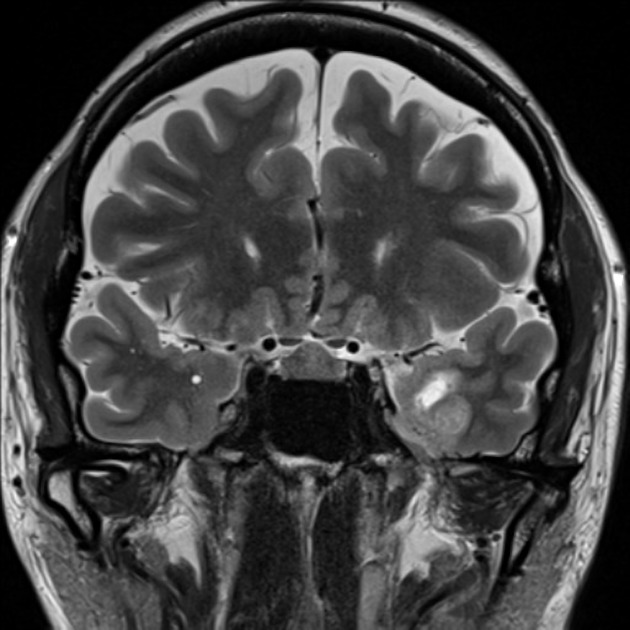
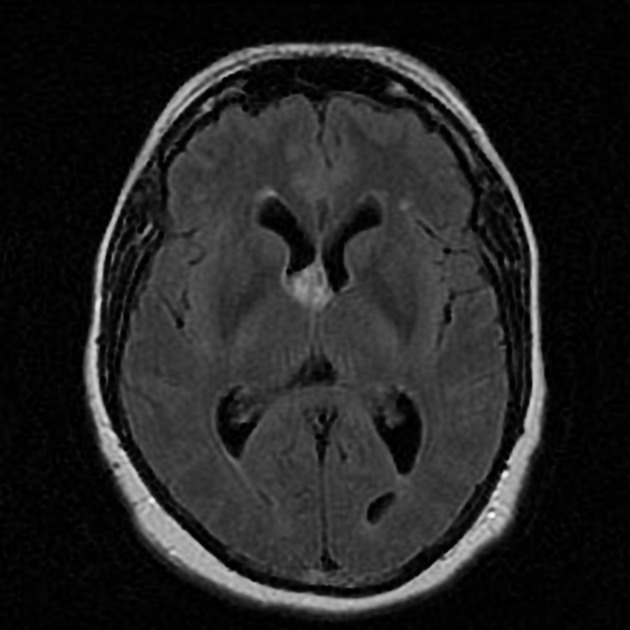
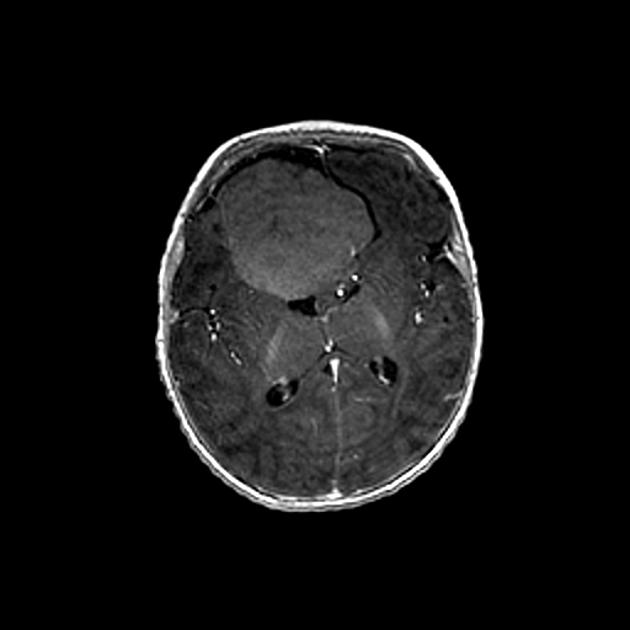
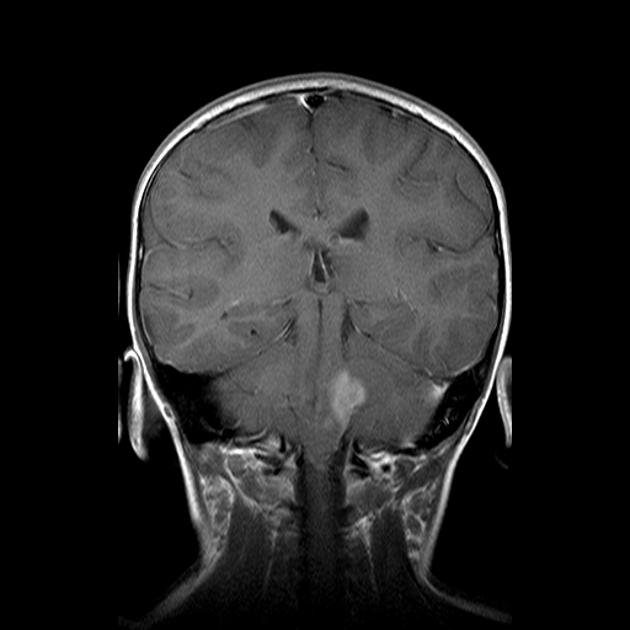
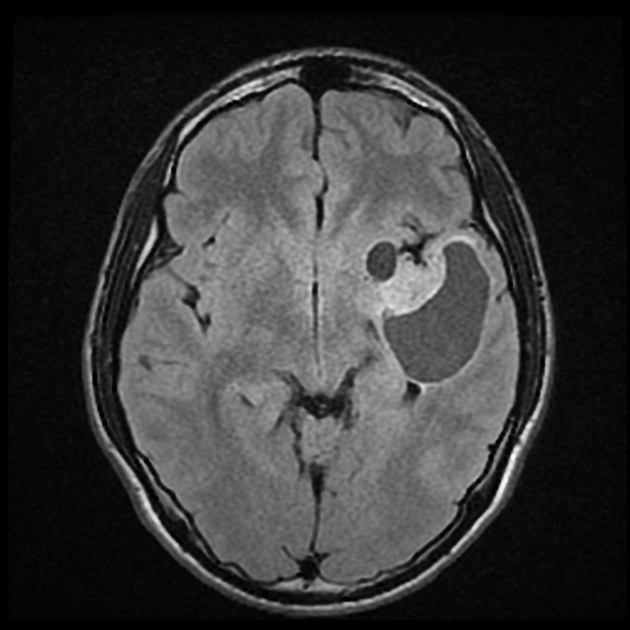
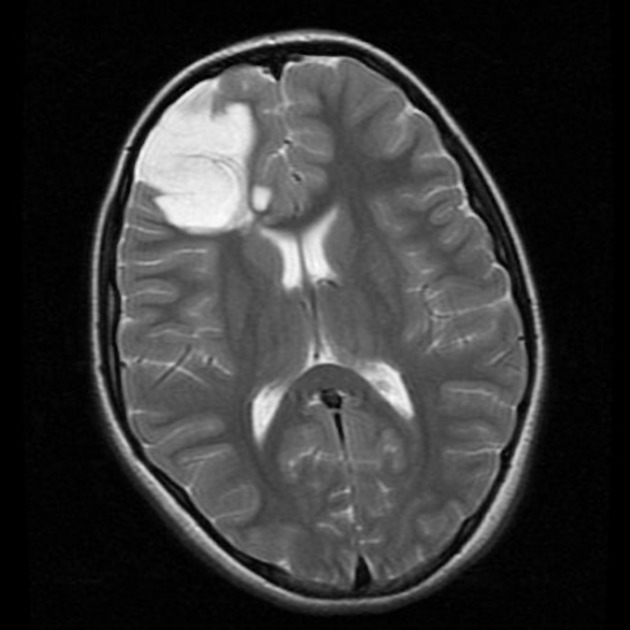
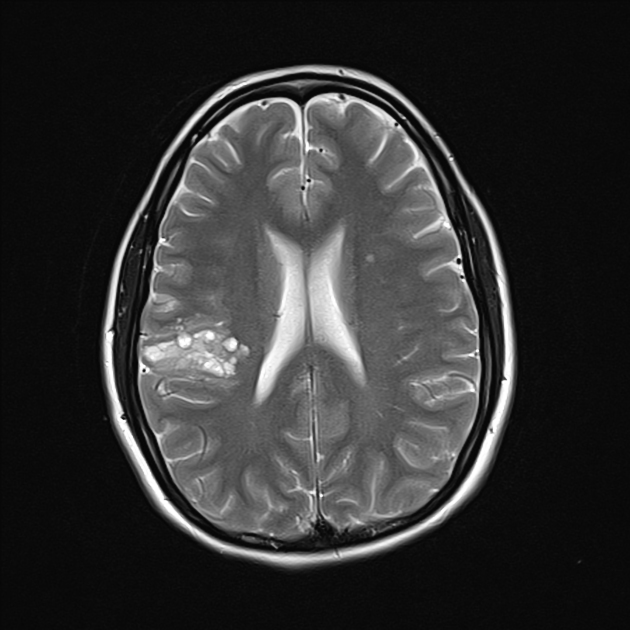
Their appearance on imaging is very variable: from a partially cystic mass with an enhancing mural nodule (~45% of cases) to a solid mass expanding the overlying gyrus. Contrast enhancement is variable.
On this page:
Epidemiology
Children and young adults are usually affected, and no gender predominance is recognized. It accounts for around 2% (from 0.4-3.8%) of all primary intracranial tumors, and up to 10% of primary cerebral tumors in children.
Clinical presentation
The most common presentation is with temporal lobe epilepsy, presumably due to the temporal lobes being a favored location.
Pathology
Gangliogliomas are most frequently found in the temporal lobes (70%) 6,9 but can occur anywhere in the central nervous system.
The majority are indolent and designated as WHO grade 1 tumors in the current (2021) WHO classification of CNS tumors, although in a minority (e.g. 5%) of cases higher grade features are present 10. These have previously been called "anaplastic gangliogliomas" although no clear grading criteria for higher-grade tumors exist at present 10.
Microscopic appearance
Gangliogliomas, as their name suggests, are composed of two cell populations:
ganglion cells (large mature neuronal elements): ganglio-
-
neoplastic glial element: -glioma
primarily astrocytic, although oligodendroglial or pilocytic astrocytoma components are also encountered 9
The proportion of each component varies widely, and it is the grade of the glial component that determines biological behavior.
Dedifferentiation into high-grade tumors does occasionally occur, and it is usually the glial component (into a glioblastoma). Only rarely is it the neuronal component (into neuroblastoma).
They are closely related to both gangliocytomas (which contain only the mature neural ganglion cellular component) and ganglioneurocytoma (which also have small mature neoplastic neurons).
Immunophenotype
Neuronal origin is demonstrated by positivity to neuronal markers 9:
synaptophysin: positive
neurofilament protein: positive
MAP2: positive
chromogranin-A: positive (usually negative in normal neurons) 9
CD34: positive in 70-80%
The glial component may also show cytoplasmic positivity for GFAP.
Genetics
BRAF V600E mutations are encountered in 20-60% of cases 9
IDH: negative (if positive then the tumor is most likely a diffuse glioma) 9
Radiographic features
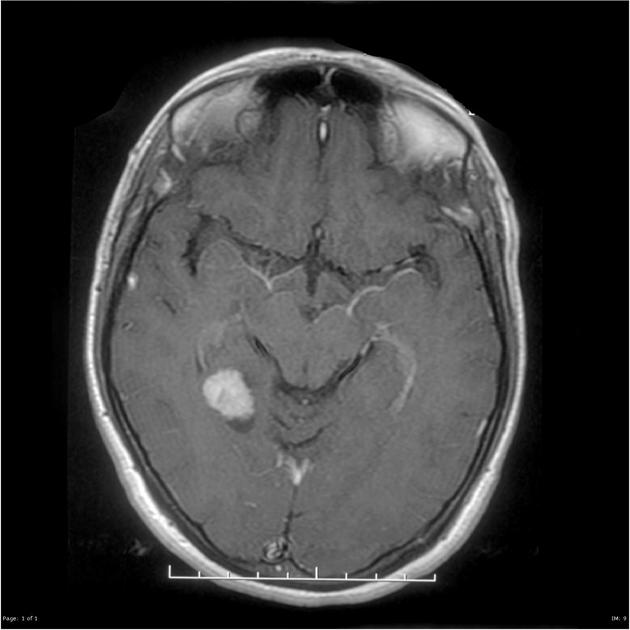
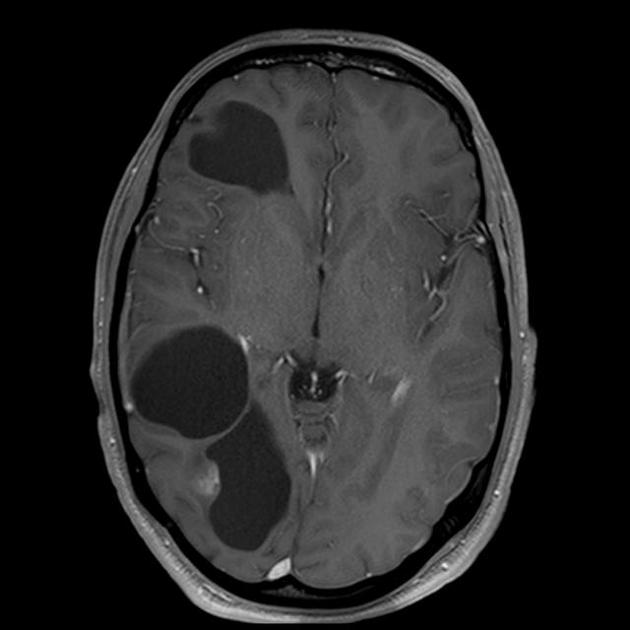
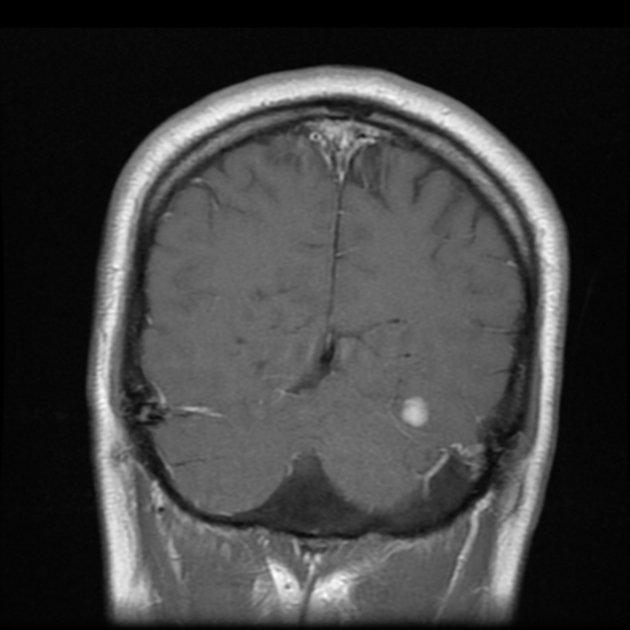
Imaging findings mirror the various patterns of growth which these tumors may demonstrate and thus their appearance is very variable. A partially cystic mass with an enhancing mural nodule is seen in ~45% of cases. They may also simply present as a solid mass expanding the overlying gyrus. An infiltrating mass is uncommon and may reflect a higher grade.
CT
Findings are of a mass that is often non-specific. General features include:
iso- or hypodense
frequently calcified ~35%
bony remodeling or thinning can indicate the slow-growing nature of a tumor
enhancement is seen in approximately 50% of cases (involving the solid non-calcified component)
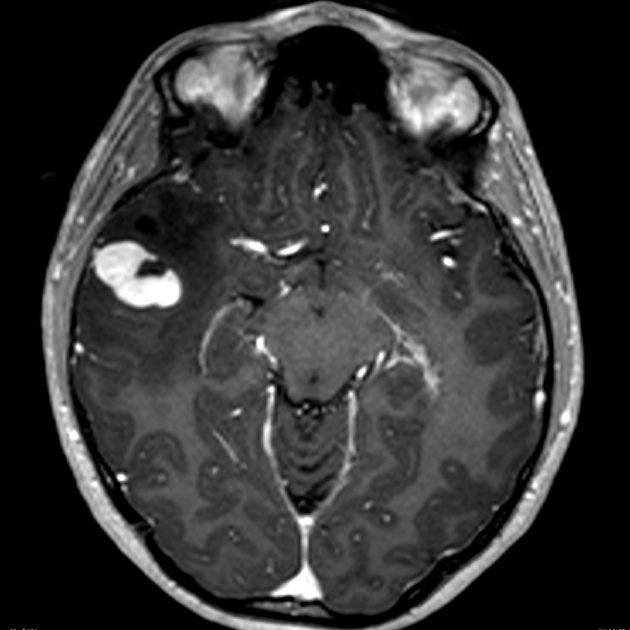
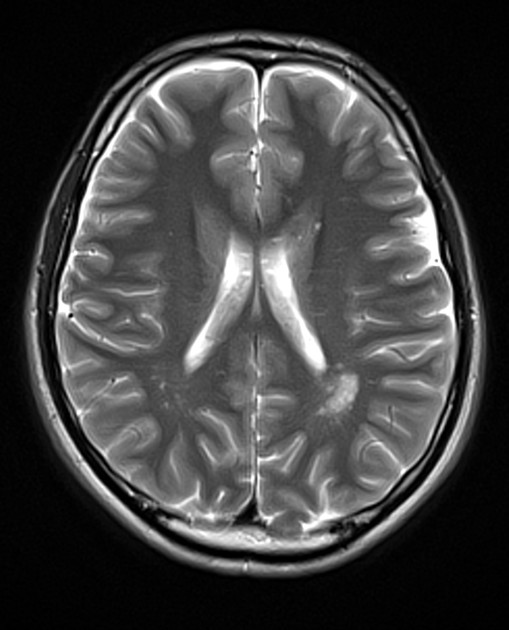
MRI
Reported signal characteristics include:
T1: solid component iso to hypointense
T1 C+ (Gd): solid component variable contrast enhancement
-
T2
hyperintense solid component
variable signal in the cystic component depending on the amount of proteinaceous material or the presence of blood products
peritumoral FLAIR/T2 edema is distinctly uncommon
T2* (GE/SWI): calcified areas (common) will show blooming signal loss
Treatment and prognosis
Local resection is the treatment of choice and determines prognosis. In the brain, when a reasonable resection margin can be achieved, the prognosis is excellent, with recurrence-free survival reported to be up to 97% at 7.5-year follow-up 9.
In contrast, when resection is not possible due to location (e.g. the spinal cord) tumor progression is common 9.
If only incomplete resection is achievable, or tumor recurrence occurs then radiotherapy may be of some benefit.
Differential diagnosis
The main differential diagnosis is that of other cortical tumors including 1-6:
-
can be indistinguishable on imaging
less common
-
polymorphous low grade neuroepithelial tumor of the young (PLNTY)
can be indistinguishable on imaging
less common
-
can be indistinguishable on imaging
rare
-
pleomorphic xanthoastrocytoma (PXA)
contrast enhancement prominent
dural tail sign is sometimes seen
-
dysembryoplastic neuroepithelial tumors (DNET)
contrast enhancement uncommon
-
usually cerebellar or optic pathway (esp in NF1)
when suptratentorial often near the ventricles
-
calcifications common
less commonly in the temporal lobes
If in the spinal cord consider:







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.