Ganglion cysts are non-malignant cystic masses that occur in association with musculoskeletal structures. They are the most common soft tissue mass in the hand and wrist.
On this page:
Terminology
Ganglion cysts are sometimes also simply referred to as ganglia or a ganglion, but should not be confused with the anatomical term ganglion.
Epidemiology
They occur more commonly in young women, especially in the hand or wrist 7.
Clinical presentation
They can cause a myriad of symptoms depending on location due to mass effect on adjacent structures, and these are best discussed under location-specific subsites. A proportion of patients have a history of trauma.
Pathology
The etiology of ganglion cysts is unclear and is generally thought to result from myxoid degeneration of the connective tissue associated with joint capsules and tendon sheaths 10. They may represent sequelae of synovial herniations or coalescence of small degenerative cysts arising from the tendon sheath, joint capsule or bursae. Typically, they are attached to the underlying joint capsule or tendon sheath 8.
Some ganglion cysts can occur in post-traumatic and post-surgical situations 12.
Location
They can occur within:
muscles: intramuscular ganglion cyst
menisci: intrameniscal ganglion cyst
tendons: intratendinous ganglion cyst 6
bones: intraosseous ganglion cyst
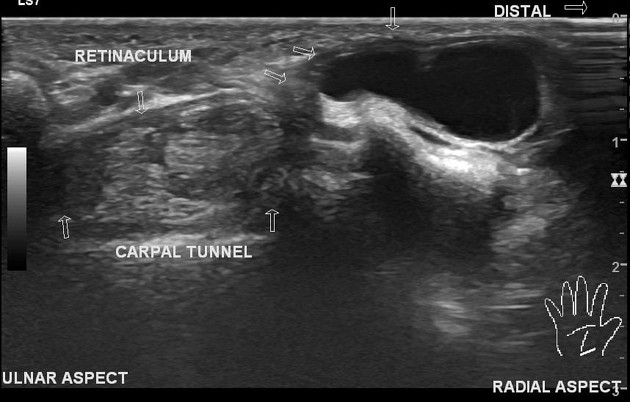
They most commonly (70-80% of cases) occur in relation to the hand or wrist (see ganglion cysts of the hand and wrist). In this location, notable specific subsites include 1:
dorsum of the wrist: ~60% of all hand ganglion cysts
volar aspect of the wrist: ~20%
flexor tendon sheath: ~10%
distal interphalangeal joint: ~10%
Other notable locations include:
spinoglenoid notch: spinoglenoid notch ganglion cyst
knee: e.g. ACL ganglion cyst
ankle/foot
Classification
There are many ways of classifying ganglion cysts.
-
in relation to bone:
within bone: intraosseous ganglion cyst
adjacent to bone: periosteal ganglion cyst - rare and may occur more frequently in males 4
away from bone: soft tissue ganglion cyst
-
in relation to a joint:
within a joint: intra-articular ganglion cyst
adjacent to a joint: juxta-articular ganglion cyst
within a peripheral nerve: intraneural ganglion cyst
Microscopic appearance
Histologically, ganglia have a thin connective tissue capsule, but no true synovial lining, and contain mucinous material filled with gelatinous fluid rich in hyaluronic acid and other mucopolysaccharides 4.
Radiographic features
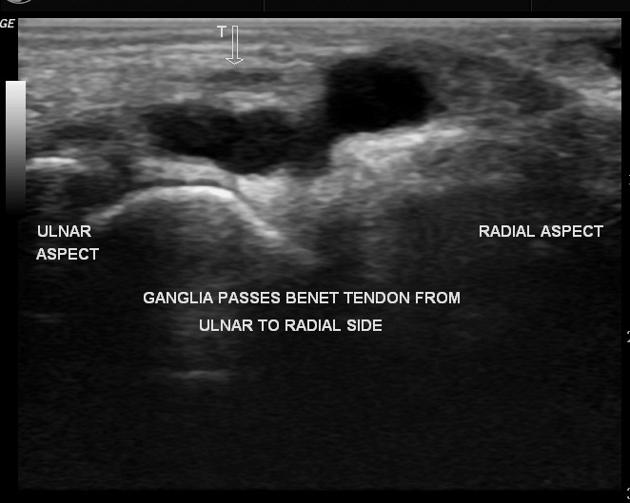
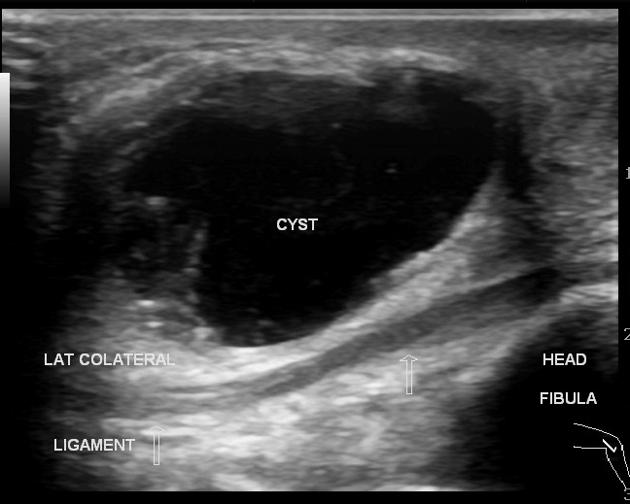
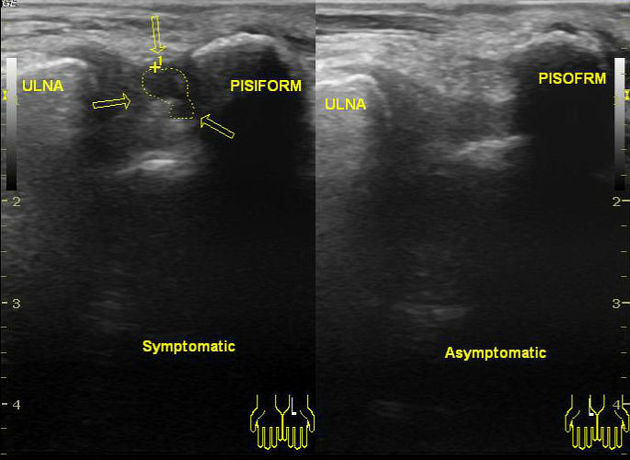
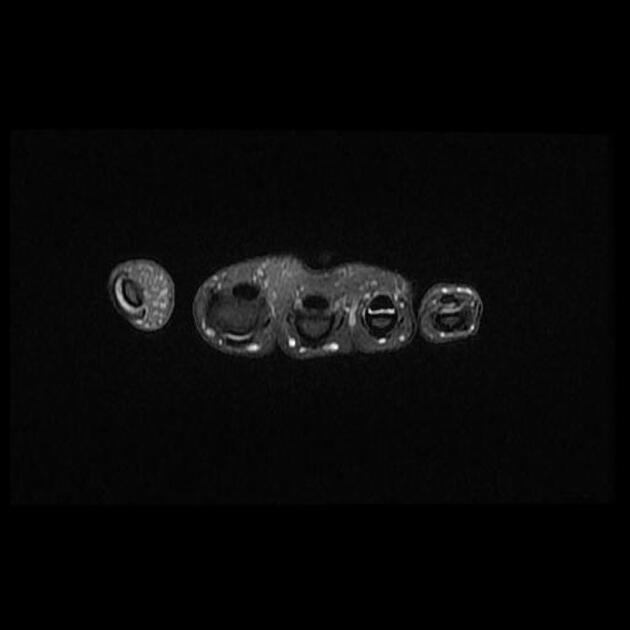
Ultrasound
The vast majority are anechoic to hypoechoic on ultrasound and have well-defined margins 3,5. Many demonstrate internal septations as well as acoustic enhancement 5.
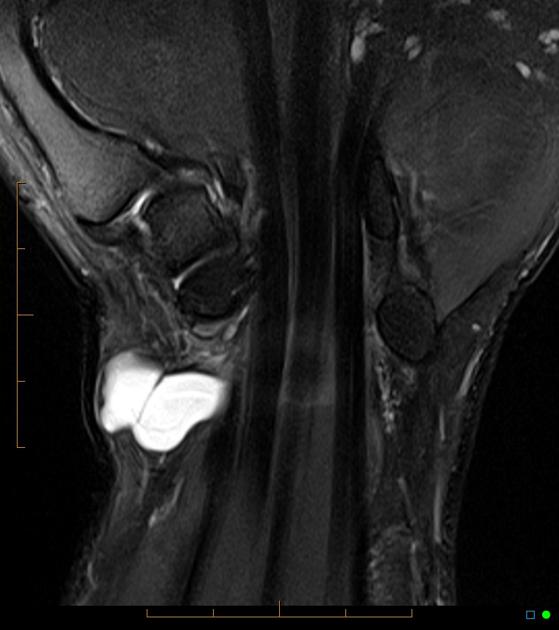
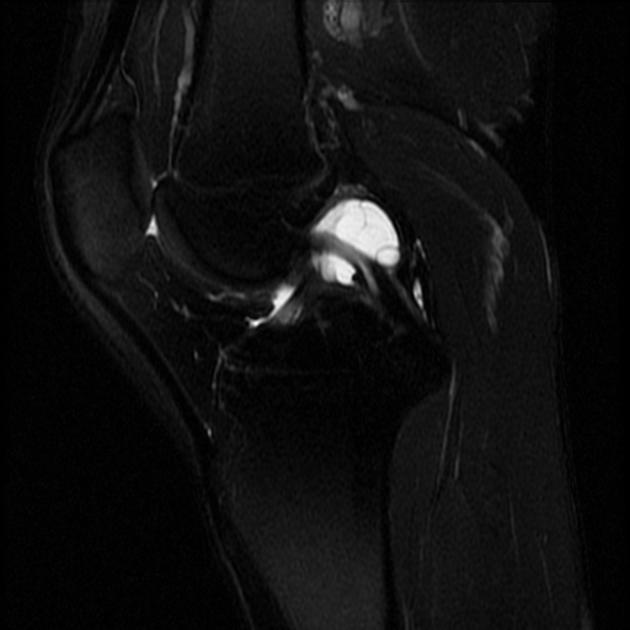
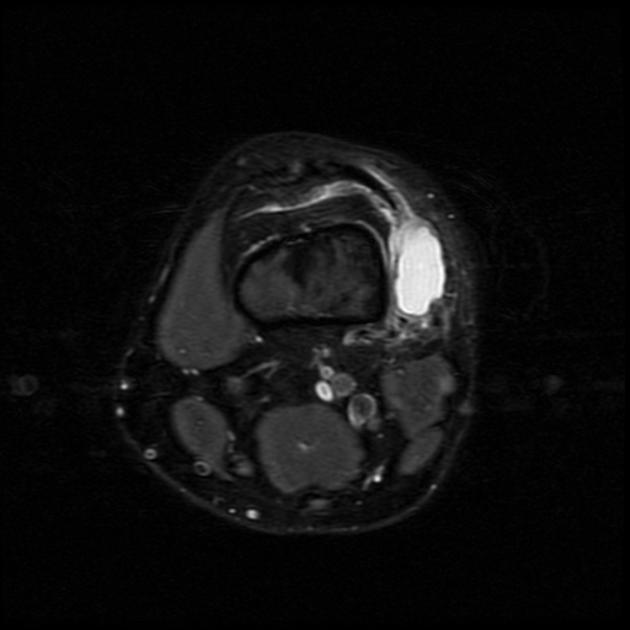
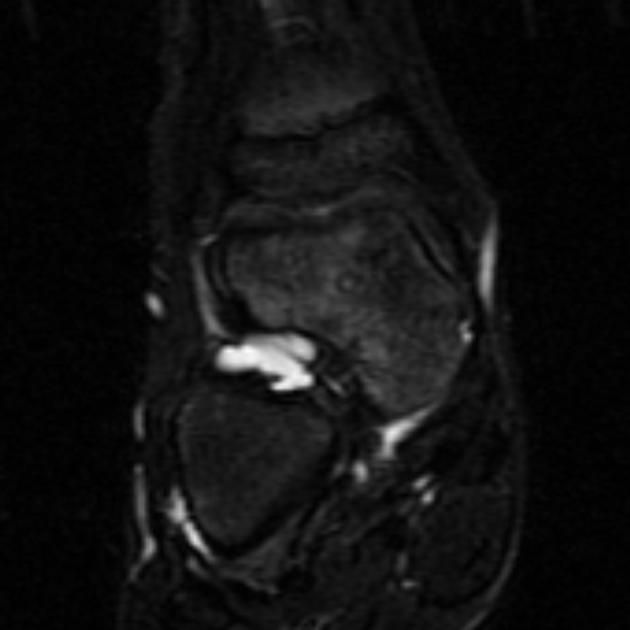
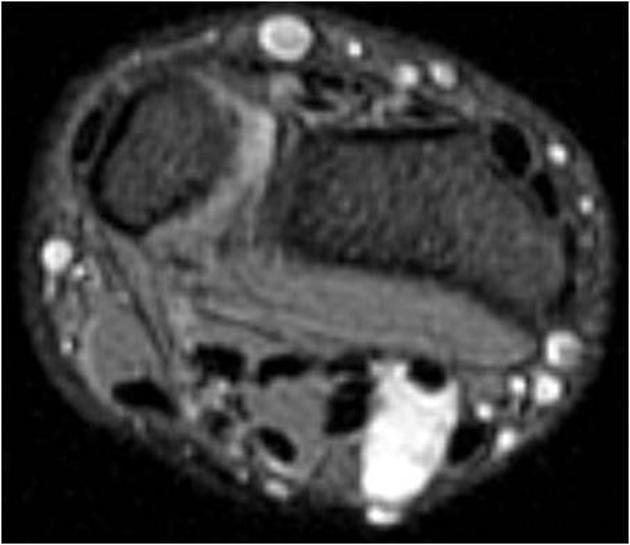
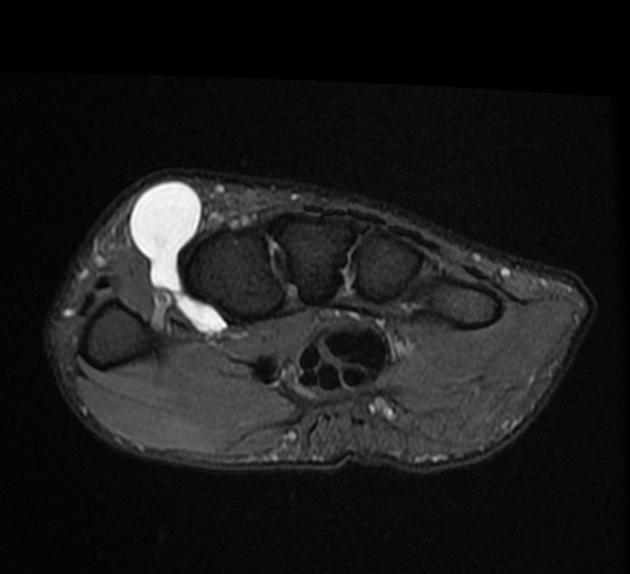
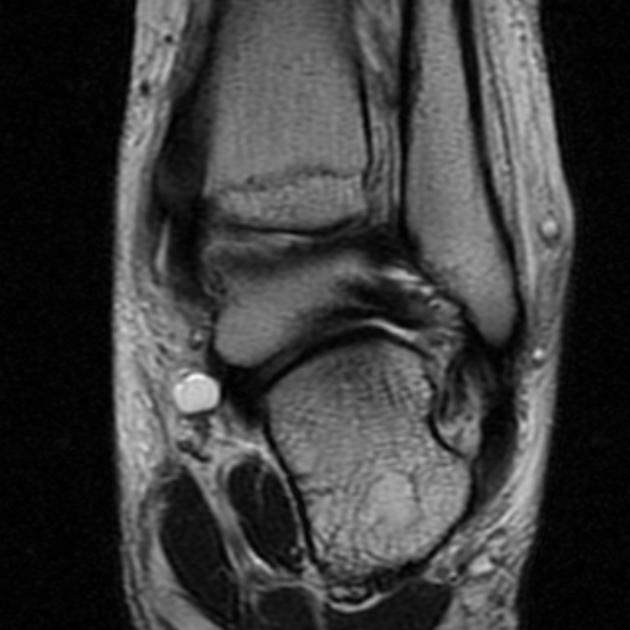
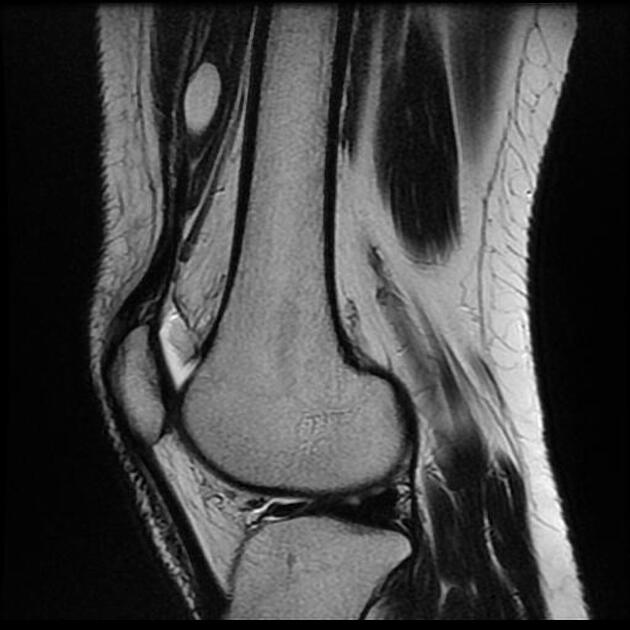
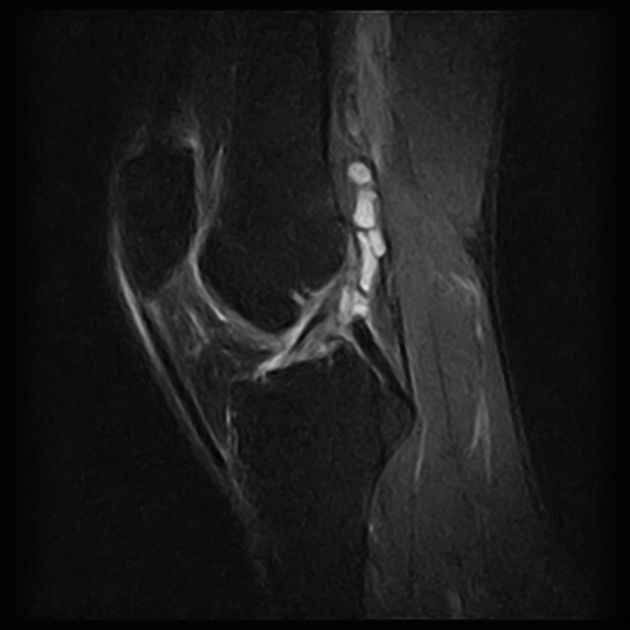
MRI
Usually seen as a unilocular or multilocular rounded or lobular fluid signal mass, adjacent to a joint or tendon sheath. Very small cysts may simulate a small effusion, but a clue to the diagnosis is the paucity of fluid in the remainder of the joint and the focal nature of the fluid. A periosteal bone formation may be visible.
T1: typically ganglia are low signal although high proteinaceous content or hemorrhage may result in lesions appearing isointense or hyperintense on T1 weighted images
T2/STIR: typically high signal
T1 C+ (Gd): thin rim or septal enhancement 13
Ruptured cysts are often irregularly delineated and show pericapsular edema on T2 weighted sequences 9. The cyst itself may show diffuse enhancement after intravenous administration of gadolinium contrast, but there is often an absence of enhancement of the pericapsular soft tissue edema.
Treatment and prognosis
Treatment is based on the severity of symptoms. Most cysts can be managed non-operatively with observation or aspiration, or be resected surgically. The rates of recurrence are lower with surgical resection (15%) compared to aspiration (50%).
History and etymology
Ganglion cysts are thought to be first described by Hippocrates as ‘‘knots of tissue containing mucoid flesh’’.
Differential diagnosis
General imaging differential considerations include:
synovial cyst: these have a synovial lining, and although they are histologically distinct from ganglia, they are indistinguishable on imaging 1












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.