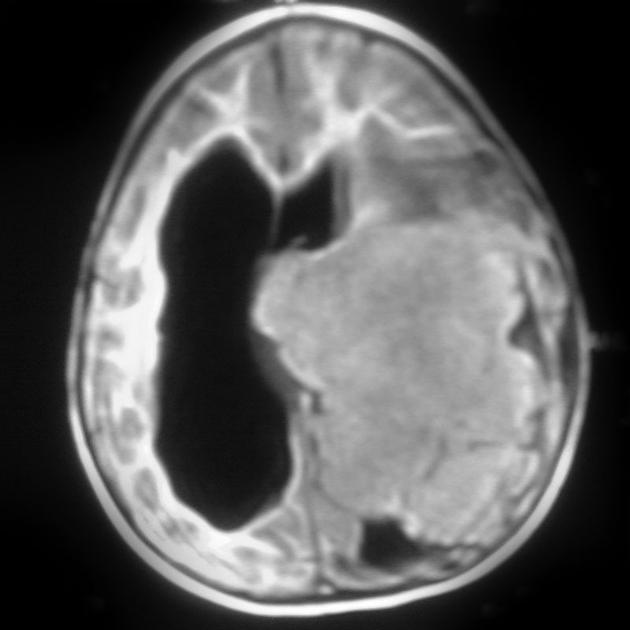
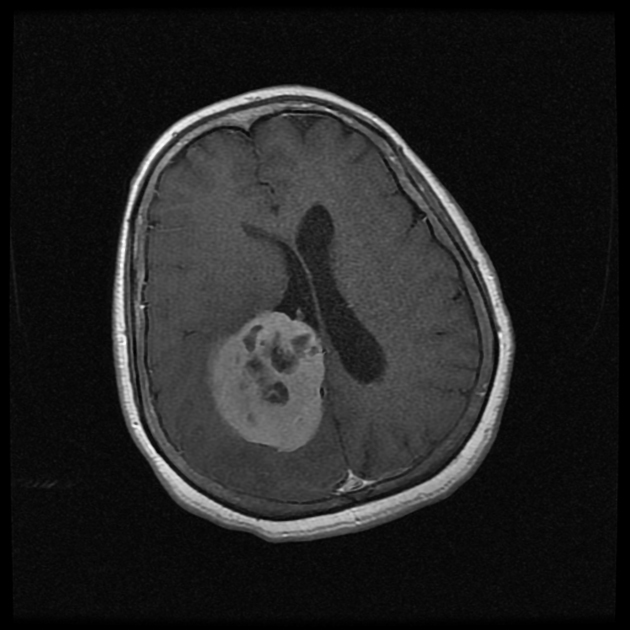
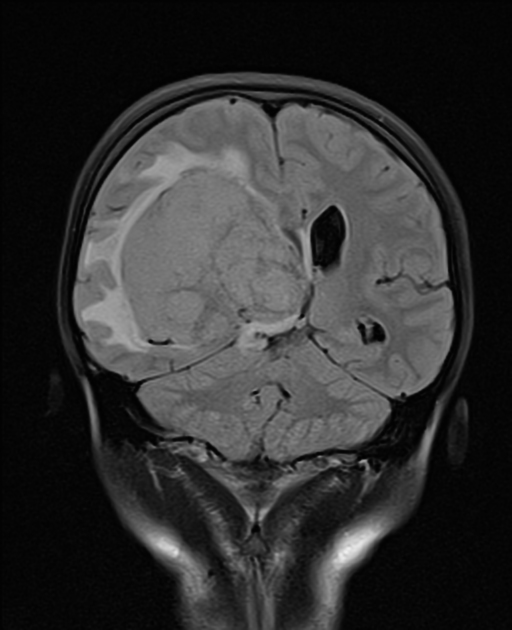
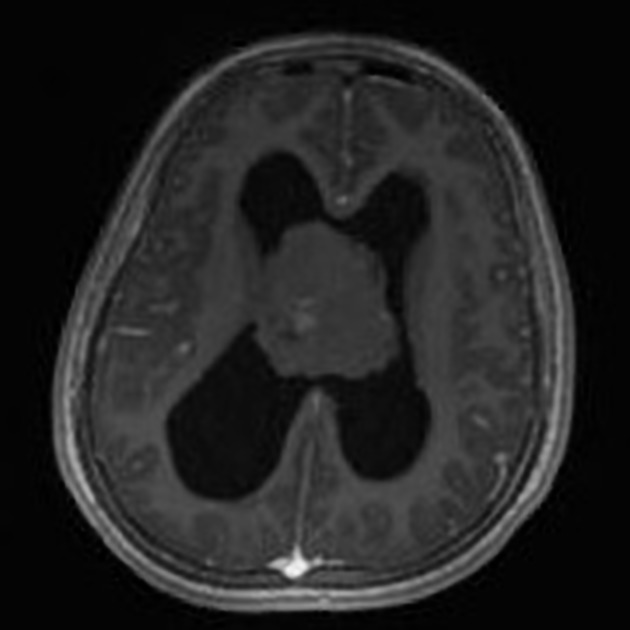
Intraventricular meningiomas are rare tumors usually encountered in adults and are somewhat distinct from the far more common extra-ventricular meningioma.
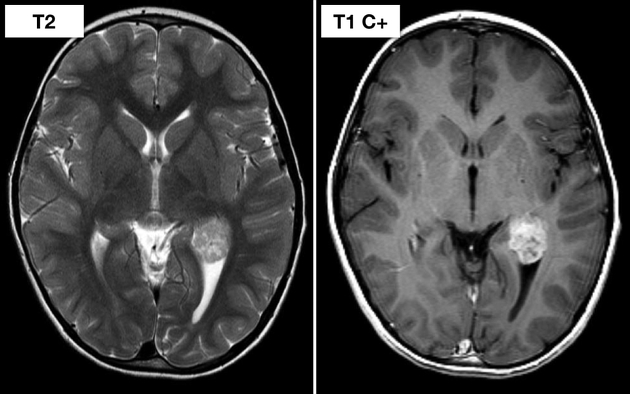
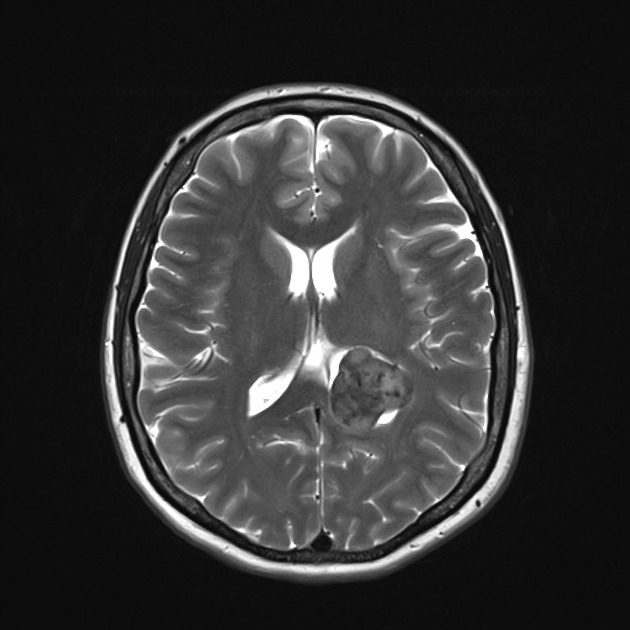
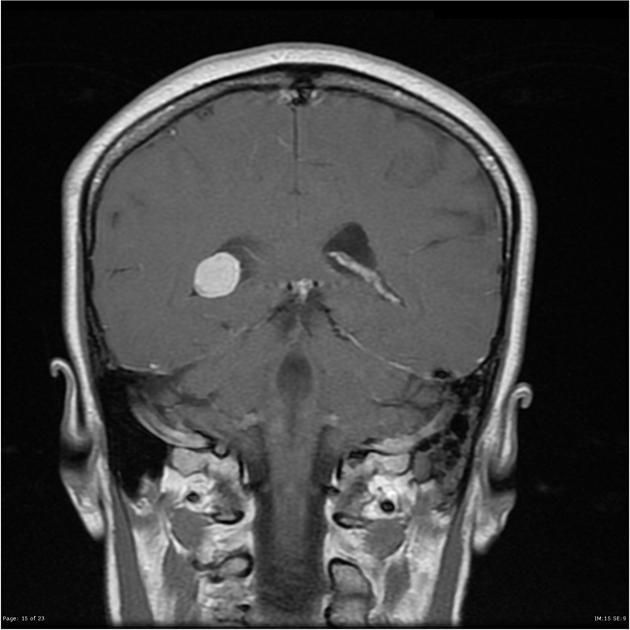
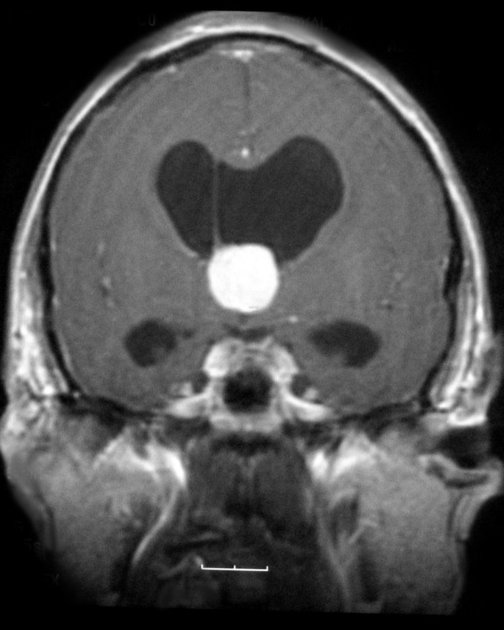
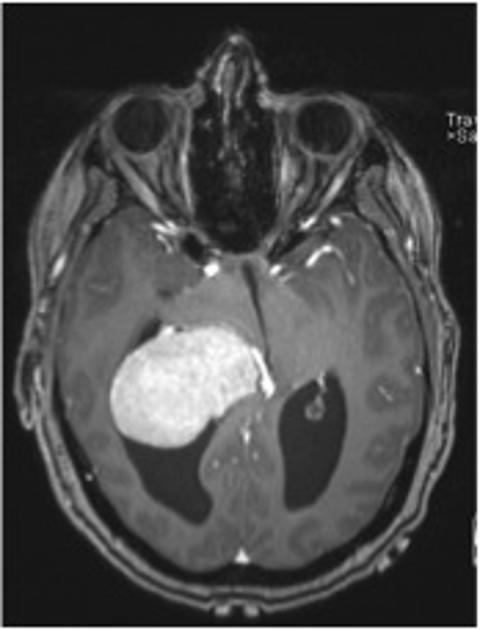
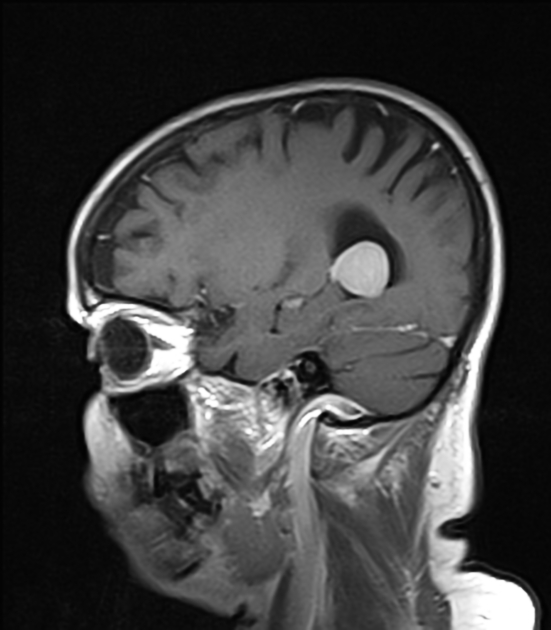
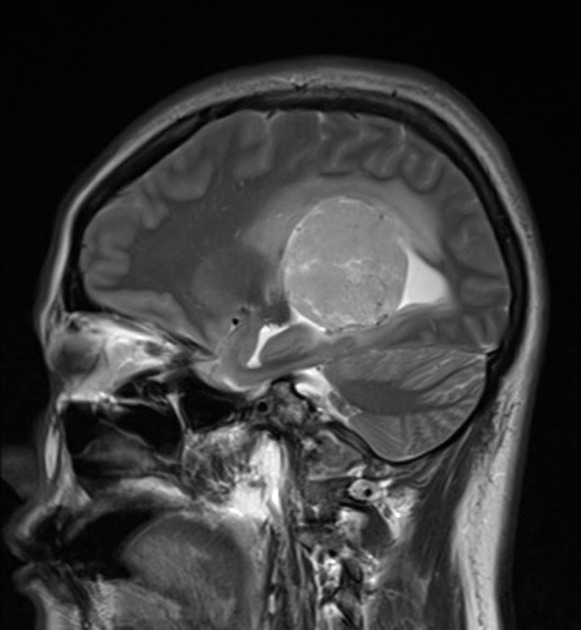
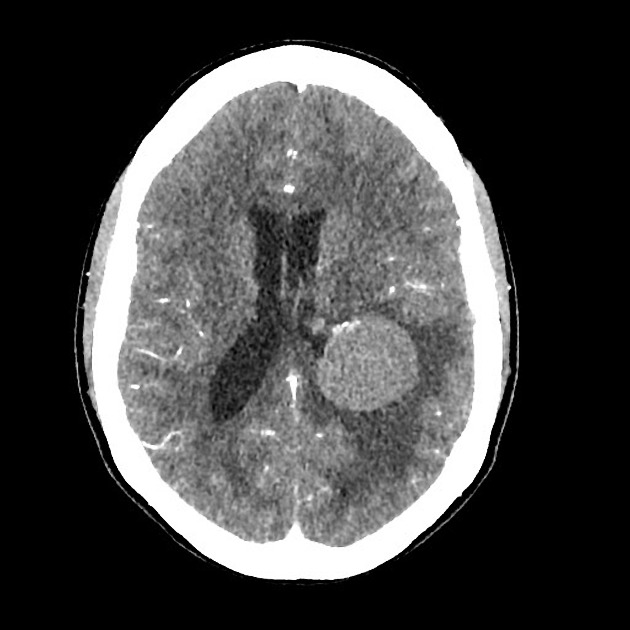
On imaging, they classically present as vividly enhancing solid mass at the trigone of the lateral ventricles.
On this page:
Epidemiology
Intraventricular meningiomas are rare, accounting for only 0.5-3% of all meningiomas 7. Nonetheless, because of the overall rarity of intraventricular tumors after childhood, they account for 10-15% of all intraventricular neoplasm in adults 7.
Most intraventricular meningiomas present between the 3rd and 6th decades 3,6 with a recognized female predilection (M:F ratio of 1:2) 4,6,7. They are rare in childhood 7.
Clinical presentation
Intraventricular meningiomas present usually due to mass effect, either by direct compression of the adjacent brain or from obstruction to normal CSF drainage with resultant hydrocephalus.
Pathology
Intraventricular meningiomas are thought to arise from mengingothelial inclusion bodies located in the tela choroidea and/or mesenchymal stroma of the choroid plexus 5,6,7. In general, these meningiomas are most commonly of the fibrous meningiomas 5.
Location
- 80% trigone of the lateral ventricle
- 15% third ventricle
- 5% fourth ventricle
Radiographic features
Their signal and attenuation characteristics are the same as other meningiomas, demonstrating essentially isodensity and intensity to grey matter precontrast and vivid, usually homogeneous enhancement following administration of contrast. Compared to extra-axial meningiomas, a greater proportion is calcified (50% compared to 20% for standard meningioma).
The vascular supply depends on the location but generally is from the arterial supply of the adjacent choroid plexus 7.
For further discussion of the radiographic appearances of these tumors, refer to the general article: meningioma.
Treatment and prognosis
As is the case with other meningiomas, provided complete excision is possible, surgical excision is curative and therefore the treatment of choice. Recurrence rate following resection is fairly low, ~5% 7.
Differential diagnosis
The differential somewhat depends on the location of the tumor and age of the patient, however, in general considerations should include:
- glial tumor
- choroid plexus metastases
- choroid plexus papilloma (particularly in children)
- CNS lymphoma
- central neurocytoma








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.