Non-compaction of the left ventricle, also known as spongiform cardiomyopathy or left ventricular non-compaction (LVNC) is a phenotype of hypertrophic ventricular trabeculations and deep interventricular recesses. It has been hypothesized to result from the arrest of normal myocardial compaction during embryogenesis, although acquired cases have also been reported.
Non-compaction of the right ventricle has been described but is rare 3.
On this page:
Terminology
There is controversy as to whether non-compaction of the left ventricle represents a distinct disease versus a phenotypic manifestation of various cardiomyopathies 9. For example, although left ventricular non-compaction is classified as primary genetic cardiomyopathy by the American Heart Association, it remains unclassified by both the World Health Organization and the European Society of Cardiology 9.
At least some of the inconsistency is due to the fact that non-compaction of the left ventricle is mostly diagnosed by morphological criteria on non-invasive imaging (e.g. echocardiography and cardiac MRI), and no universally accepted criteria exist.
Additionally, findings of non-compaction of the left ventricle may be seen in a spectrum of clinical presentations. It may be seen as a component of cardiomyopathy, such as in Barth syndrome, or in concert with other myocardial structural/functional abnormalities (e.g. dilated, restrictive, arrhythmogenic right ventricular cardiomyopathies); however, it may be acquired/reversible and/or observed in subjects with normal left ventricular function and size.
Thus, findings of left ventricular non-compaction should not be equated with cardiomyopathy or aberrant left ventricular function, as the findings should be integrated into a holistic evaluation of cardiac function in deciding a final diagnosis 6.
Clinical presentation
While non-compaction of the left ventricle may be an isolated morphological variant, discovered in patients with otherwise structurally and functionally normal hearts, it may also present as a component of congenital heart disease or true cardiomyopathy; in this latter instance, it may present as congestive heart failure. Other presenting features may include 8:
-
exertional syncope
-
might be associated with a long QT interval
may predispose to a subtype of polymorphic ventricular tachycardia, torsades de pointes
-
-
systemic thromboembolic events
may lead to transient ischemic attacks or stroke
Pathology
Associations
In most patients with non-compaction of the left ventricle, there are no other cardiac malformations. Both familial and sporadic forms have been described 1. However, in at least one study, approximately 12% of patients had associated cardiac malformations 1:
ventricular outflow tract / left ventricular outflow tract abnormalities (46%, mainly bicuspid aortic valve)
Ebstein anomaly (25%)
more rarely: tetralogy of Fallot or coarctation of the aorta
Radiographic features
Plain radiograph
Chest radiographs are not useful in the diagnosis of non-compaction of the left ventricle. They are more useful in identifying complications of cardiomyopathy, such as pulmonary edema and cardiomegaly.
Ultrasound
Echocardiography
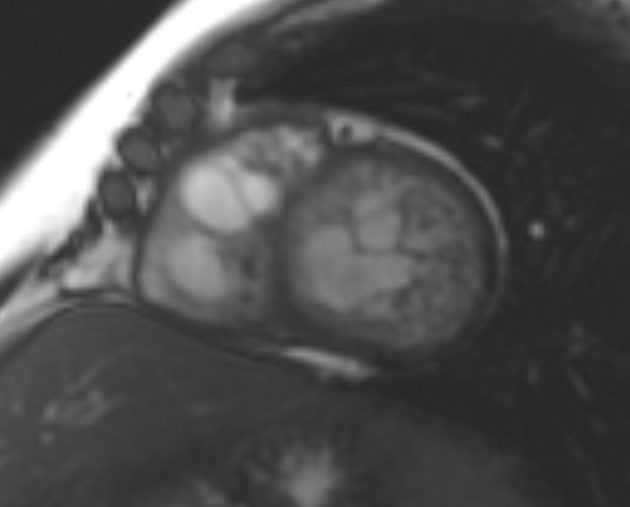
Echocardiography was traditionally used in the diagnosis of left ventricular non-compaction, with the addition of contrast greatly increasing the sensitivity of this examination. However, cardiac MRI is now considered the modality of choice to make this diagnosis. There are no universally accepted echocardiographic criteria for left ventricular non-compaction. Most common echocardiographic features include 7:
-
a bilayered mural appearance of the left ventricle
-
the relatively hypoechoic inner layer of the left ventricular wall representing the endocardium/myocardium is hypertrabeculated
referred to as the non-compacted or "NC" layer
the non-compacted layer is surrounded by the outer "compacted" layer, representing the epicardium
-
classical definition based on the ratio between non-compacted vs compacted myocardium
increased thickness of the non-compacted layer with a non-compacted/compacted ratio >2.3 consistent with the diagnosis
-
-
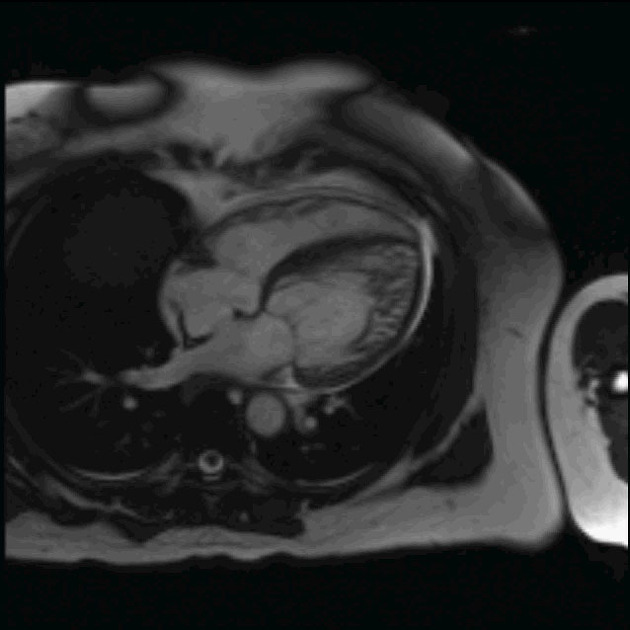
regional increase in left ventricular trabeculation
predominantly affects the inferolateral walls and the apex
parasternal short axis (or apical four/two/long-axis view) should reveal at least four trabeculations
-
pronounced intertrabecular "crypts" or recesses
continuity with the left ventricular cavity may be demonstrated by color flow Doppler
Other commonly associated features include:
-
left ventricular dysfunction
intraventricular thrombus
-
associated with atrial fibrillation
MRI
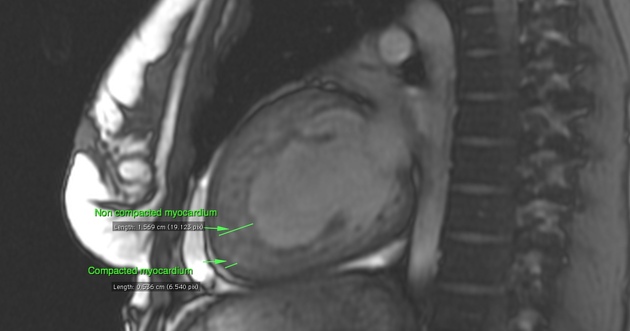
Cardiac MRI (CMR) has a better contrast resolution than echocardiography and it is the modality of choice for the diagnosis of spongiform cardiomyopathy.
A good diagnostic clue is a ratio of non-compacted telediastolic myocardium to compacted telediastolic myocardium of more than 2.3:1 (sensitivity: 86%, specificity: 99%) 10,11.
For improved discrimination of left ventricular non-compaction versus other cardiomyopathies with hypertrabeculated myocardium the following MRI criteria were proposed 11,12:
percentage left ventricular myocardial mass (non-compacted) >25 %
total left ventricular myocardial mass index (non-compacted) >15 g/m2
non-compacted/compacted myocardium ratio of ≥3:1 in at least one of the following segments (1–3, 7–16) – the apical segment 17 is excluded
trabeculation (non-compacted/compacted) in segments 4–6 of ≥2:1
Radiology report
The radiology report should include a description of the following:
ratio non-compacted to compacted enddiastolic myocardium
affected left ventricular segments
left ventricular myocardial mass (compacted and non-compacted myocardium)
Treatment and prognosis
The only definitive treatment of left ventricular non-compaction is heart transplantation. Otherwise, prevention of both heart failure and thromboembolic events are the main target of treatments.
Differential diagnosis
Possible differential considerations in certain situations include:






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.