Paraovarian cysts are remnants of the Wolffian duct in the mesosalpinx that do not arise from the ovary. They account for ~15% (range 10-20%) of adnexal masses 3,4.
On this page:
Terminology
Paraovarian cysts are sometimes called paratubal cysts or hydatid cysts of Morgagni 14.
Epidemiology
They typically occur in women aged 20-40 years ref.
Clinical presentation
Most are asymptomatic, although patients with large lesions can present with pelvic pain ref.
Pathology
They usually occur around the broad ligament and arise from paramesonephric, mesothelial, or mesonephric remnants. They are usually simple cysts (although some authors include paraovarian cystadenomas under the umbrella of paraovarian cysts) ref.
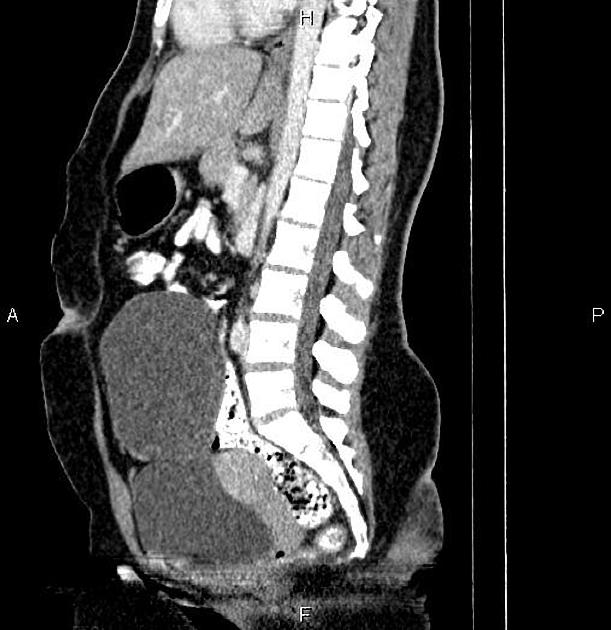
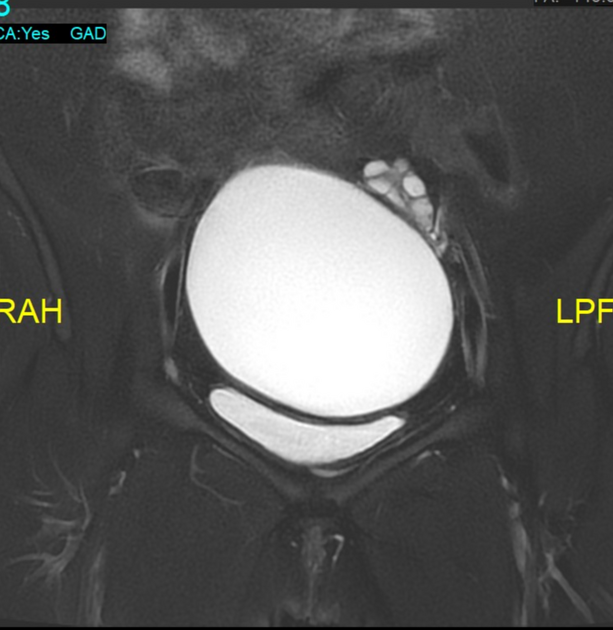
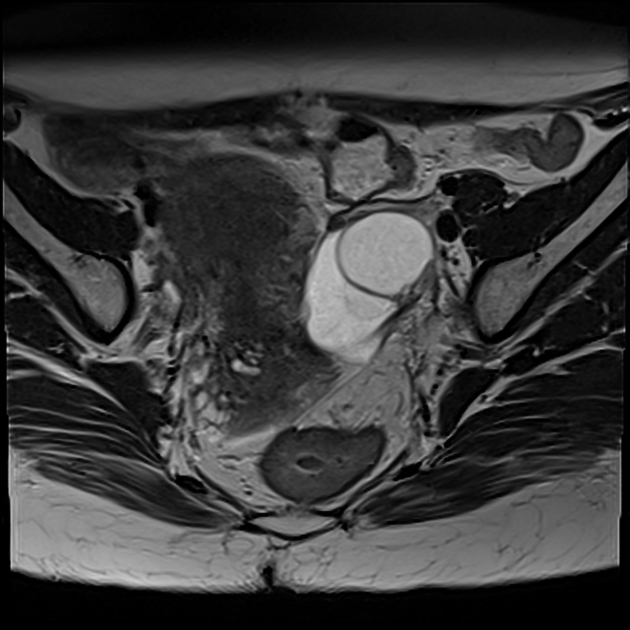
Radiographic features
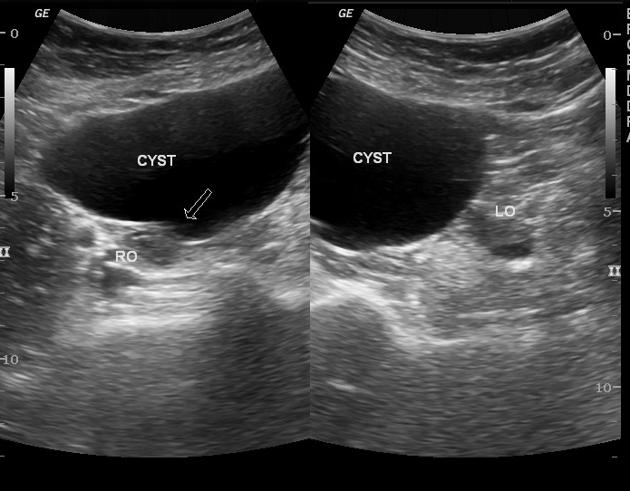
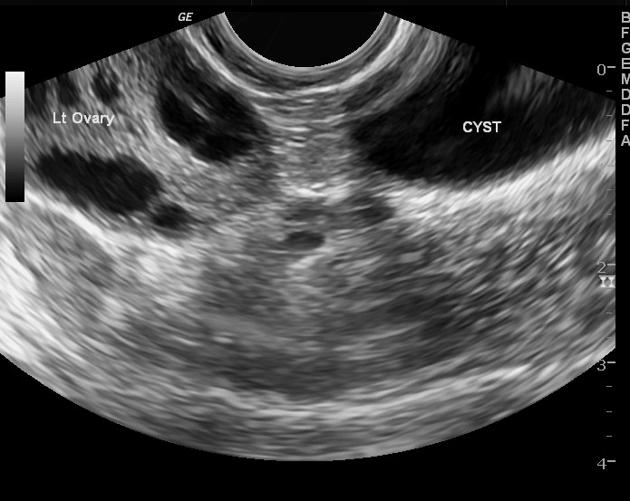
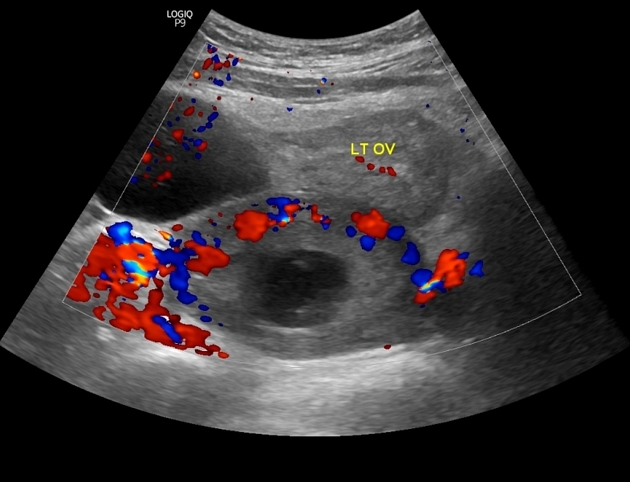
A paraovarian cyst is easier to recognize if the ipsilateral ovary is demonstrated to be separate from it ref.
Ultrasound
typically thin-walled and smoothly marginated ref
typically unilocular simple cyst (in ~66%); rarely multilocular (~4%) ref
cyst moves independently of ovary when transducer pressure is applied ref
rarely, a soft tissue nodule in the cyst may indicate the development of a neoplasm 9
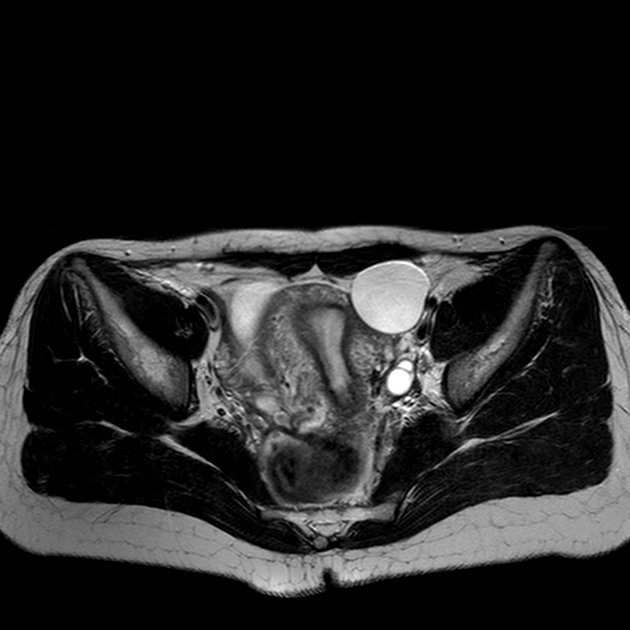
MRI
Often seen located close to the ipsilateral round ligament and when uncomplicated are of homogeneous fluid signal intensity 12. A beak sign may be present 11.
Signal characteristics
-
T1
hypointense
can be hyperintense if complicated by hemorrhage
T2: hyperintense
Treatment and prognosis
Paraovarian cysts occasionally can be complicated by rupture, torsion, or hemorrhage. Large or symptomatic cysts often undergo surgical resection. Smaller asymptomatic ones are treated conservatively ref.
Given a small chance of representing neoplasm, paraovarian cystic lesions may be recommended for follow-up imaging. Societal guidelines differ in this regard.
The 2010 Society of Radiologists in Ultrasound consensus statement recommends follow-up of simple paraovarian cysts in situations similar to that of simple ovarian cysts 13:
5-7 cm simple cyst in premenopausal women: yearly ultrasound
1-7 cm simple cyst in postmenopausal women: yearly ultrasound
>7 cm simple cyst in any age: further imaging (e.g. MRI) or surgical evaluation
In contrast, the American College of Radiology Ovarian-Adnexal Reporting and Data System (O-RADS) for ultrasound, published in 2019, recommends the following 15:
any size simple paraovarian cyst in premenopausal women: no follow-up
any size simple paraovarian cyst in postmenopausal women: optional single follow-up study in 1 year
nonsimple paraovarian cysts: management dependent on risk stratification as per ovarian criteria
Finally, the American College of Radiology Incidental Findings Committee on adnexal findings on CT or MRI recommends that for paraovarian cysts with characteristic features, further imaging is usually unnecessary 16.
Differential diagnosis
For an adnexal cystic lesion consider ref:
true ovarian cyst
ovarian cystic neoplasm: typically has a solid component
paraovarian cystadenoma: typically has a small solid nodule or septum
pelvic peritoneal inclusion cyst







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.