Percutaneous cholecystostomy is the image-guided placement of a drainage catheter into the gallbladder lumen. This minimally invasive procedure can aid in patient stabilization in order to enable a more measured surgical approach with time for therapeutic planning.
A 2018 study demonstrated no difference in mortality between percutaneous cholecystostomy and laparoscopic cholecystectomy in high-risk patients with acute calculous cholecystitis, however, laparoscopic cholecystectomy had a significantly lower complication rate than percutaneous cholecystostomy 11.
On this page:
Indications
poor surgical candidate / high-risk patients with acute calculous or acalculous cholecystitis 3
unexplained sepsis in critically ill patients (diagnostic for cholecystitis as etiology of sepsis if clinical improvement after cholecystostomy)
access to or drainage of the biliary tree following failed ERCP and PTC
Contraindications
Absolute contraindications
usually none
Relative contraindications
bleeding diathesis: all attempts should be made to correct coagulopathy
ascites: thought to increase the risk of failed track maturation but a 2015 study demonstrated this is not increased when compared to patients without ascites 10
gallbladder tumor that might be seeded
gallbladder packed with calculi preventing catheter insertion
Procedure
Preprocedural evaluation
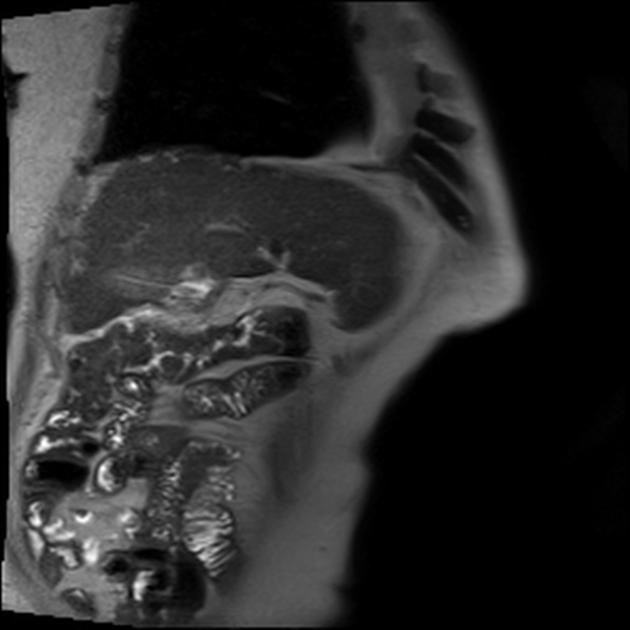
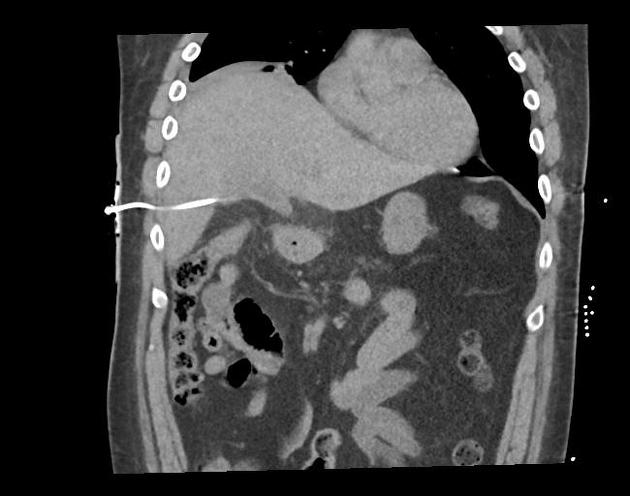
review all available imaging to confirm the indication for the procedure; previous imaging studies help to assess gallbladder anatomy and plan safe access routes to the gallbladder
check full blood count and coagulation profile to assess the risk of hemorrhage
obtain informed consent for the procedure
obtain satisfactory peripheral IV access
administer broad-spectrum IV antibiotics 1-4 hours prior to the procedure; septic patients are often already on parenteral antibiotics
arrange analgesia and sedation arranged according to patient comfort and institutional protocols
Laboratory parameters for a safe procedure
There are widely divergent opinions about the safe values of these indices for percutaneous procedures. The values suggested below were considered based on the literature review, whose references are cited below.
Complete blood count: platelet >50,000/mm3 (Some institutions determine other values between 50,000-100,000/mm3) 6,8.
Coagulation profile: some studies showed that having a normal INR or prothrombin time is no reassurance that the patient will not bleed after the procedure 7.
international normalized ratio (INR) ≤1.5 8
normal prothrombin time (PT), partial thromboplastin time (PTT)
Positioning and room set-up
the procedure is performed with the patient in a supine position
regular monitoring of the vital signs by a suitably trained staff member is recommended during the procedure
clean skin with an antiseptic solution and drape to maintain sterility for the procedure
Equipment list
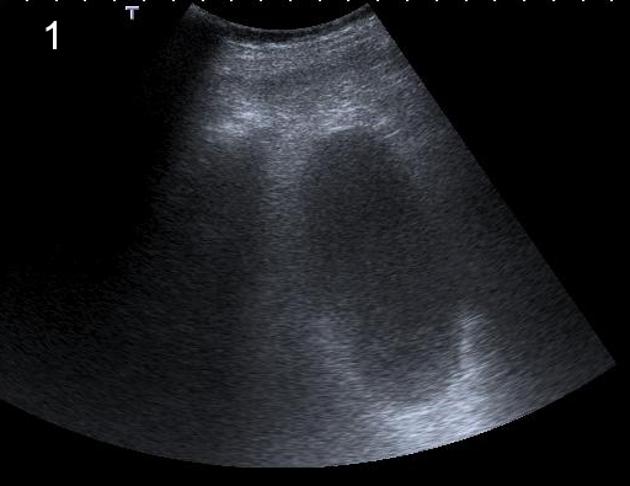
This procedure is often performed using ultrasound guidance, which was chosen to describe the procedure in this article. Alternatively, modalities such as fluoroscopy or CT can also be used depending on the clinical situation, availability and local expertise:
ultrasound machine
sterile ultrasound probe cover and sterile ultrasound gel
local anesthesia typically with 1% lidocaine
-
trocar technique:
8-10 French locking pigtail catheter with trocar (thick or purulent bile may require catheter >8 Fr)
-
18-gauge needle
0.035" guidewire with 3 mm J-tip
7-9 French dilator
8-10 French locking pigtail catheter
Technique
clean skin with a preparatory solution
place a sterile drape to isolate the sterile field
apply 1% lidocaine local anesthetic; anesthetize the liver capsule when using a transhepatic route
make skin "nick" with #11 blade
insert catheter using trocar or Seldinger technique
secure catheter to the skin (commercial fixation system could be used)
attach the gravity drainage bag to the catheter
send bile for Gram stain, culture and/or cell count
Seldinger technique
The gallbladder is punctured with an 18 or 19 G needle under ultrasound guidance. Bile can then be aspirated for microbiological studies. A 0.035 guidewire is used to exchange the needle for a dilator and an 8 French or larger pigtail drain is placed within the gallbladder. The drain can often be visualized under ultrasound. Aspiration of bile/pus from the drain confirms satisfactory position.
Also see main article: Seldinger technique.
Trocar technique
Load a 8 Fr locking pigtail catheter over a trocar. Advance the catheter assembly into the gallbladder lumen under ultrasound guidance; it is usually possible to visualize tip in the gallbladder lumen. Aspiration of bile/pus from the drain confirms a satisfactory position. Unscrew trocar from catheter; advance catheter over trocar into gallbladder, then remove trocar and lock pigtail.
Seldinger vs Trocar technique
In general, due to the small diameter of the needle that is used for the initial puncture when undertaking percutaneous cholecystostomy with the Seldinger technique, for many years it has been considered a safer option when compared to the larger diameter of the pigtail catheter that is inserted at once with the trocar technique 12. However, prospective trials (c. 2023) 13,14 comparing the trocar technique and the Seldinger technique for percutaneous cholecystostostomy have shown that the trocar technique is just as effective and at least as safe as the Seldinger technique. The trocar technique is also easier to use, places the catheter faster, and causes less pain for the patient 13,14.
Postprocedural care
Bed rest (typically 2-4 hours) with regular monitoring of vital signs and provision of adequate analgesia are routinely indicated in the first few hours following the procedure. Catheter is flushed and aspirated regularly with saline (6 to 8 hourly). A cholecystogram (injection of contrast into the indwelling catheter under fluoroscopy), performed when the patient is stable, helps establish satisfactory catheter position and the state of the gallbladder. It also allows for assessment of any residual calculi in the biliary tree.
The catheter can be removed once the tract is mature. When PC placement is done via the transhepatic route, most patients typically need two weeks for tract maturation, and when it is done via the transperitoneal route, it usually takes at least three weeks 15. A trial of clamping the catheter for 24 hours is usually done prior to removing the catheter.
Taking into account age and comorbidities, cholecystectomy after the resolution of cholecystitis is normally performed in order to prevent recurrent cholecystitis. 9
If percutaneous cholecystostomy is being used as the definitive therapy, to ensure optimal treatment, it is recommended to do a tube exchange with a concomitant fistulography every three months 16.
Complications
The occurrence of death directly caused by the procedure is exceedingly uncommon and is primarily linked to the presence of other comorbidities that are characteristic of these vulnerable patients. Complications include 5, 12, 16:
catheter displacement/migration (most common)
bile leakage and biliary peritonitis (see: biloma)
bowel injury (transperitoneal puncture)
pleural space injury (leading to pneumothorax or pleuro-biliary fistula)
bradycardia and hypotension from gallbladder manipulation
bleeding (both major and minor)
hemobilia
cholangitis
sepsis
formation of abscesses







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.