Rectal cancer, although sharing many of the features of generic colorectal carcinoma (CRC), has different preoperative imaging assessment, with MRI rectum as the mainstay for local staging and distinct surgical techniques (i.e. total mesorectal excision).
On this page:
Epidemiology
Rectal cancer is generally considered a disease of the elderly, but the incidence of cases in patients under the age of 50 has been increasing. There is a slight male predilection, not seen in cancers of the rest of the large bowel.
Clinical presentation
Patients often present with altered bowel habit or rectal bleeding 3.
Pathology
Similarly to the rest of the colon, the vast majority of rectal tumors are adenocarcinomas (98%), with neuroendocrine tumors, lymphoma, GIST, and squamous cell carcinomas making up most of the remainder 2.
In addition to conventional adenocarcinomas, there are two important subtypes that produce and contain mucin. Mucinous adenocarcinoma is characterized by abundant production of extracellular mucin, accounts for up to 10% of rectal adenocarcinomas and is associated with a higher T category at diagnosis, greater risk of metachronous metastases and poorer overall survival 13.
Signet ring cell is the second mucin producing subtype of adenocarcinoma, with variable reported incidence in different populations, up to 2.4% in the West and up to 25% in South East Asia and the Middle East, although many studies describing this subtype are single-center studies. It affects a younger group of patients than other types of adenocarcinoma. The histopathology features are similar to linitis plastica of the stomach, with abundant intracytoplasmic mucin that displaces the nucleus to the periphery, producing the appearance of a signet ring. It has a poorer prognosis with a greater propensity for lymphatic, vascular and perineural invasion. It grows submucosally which may lead to later presentation due to a delay in symptoms caused by no mucosal abnormalities 12.
It should be noted that the third setting in which rectal cancers may contain mucin is as a post-treatment response to a tumor which was a conventional adenocarcinoma at baseline.
Radiographic features
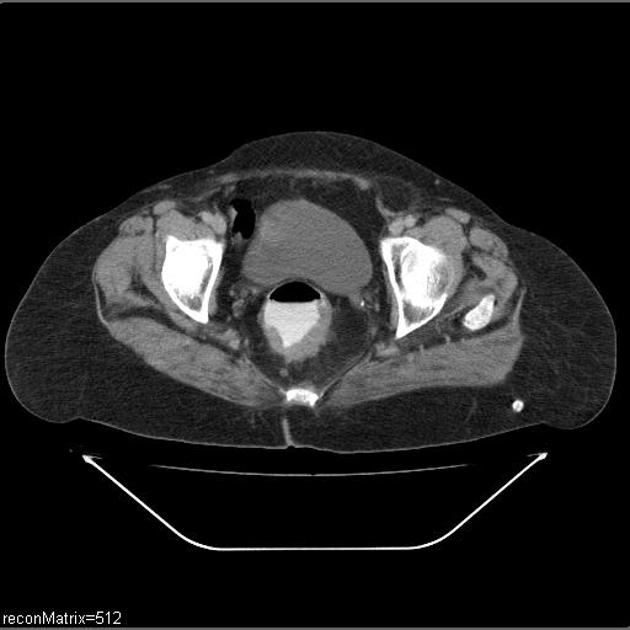
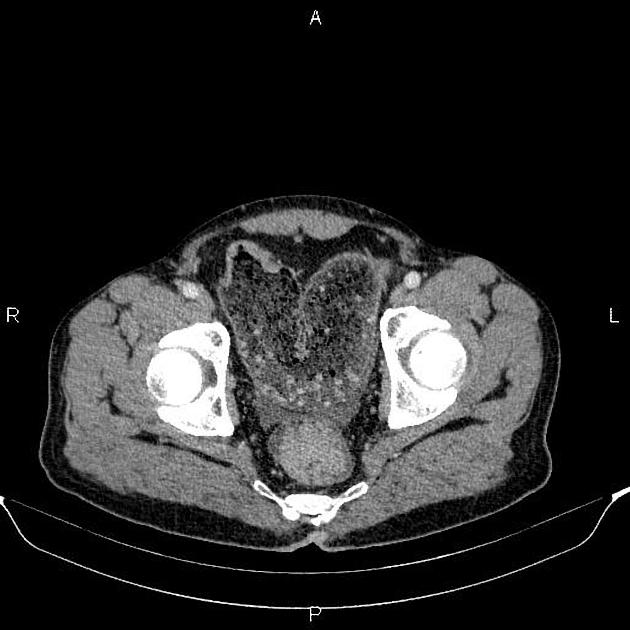
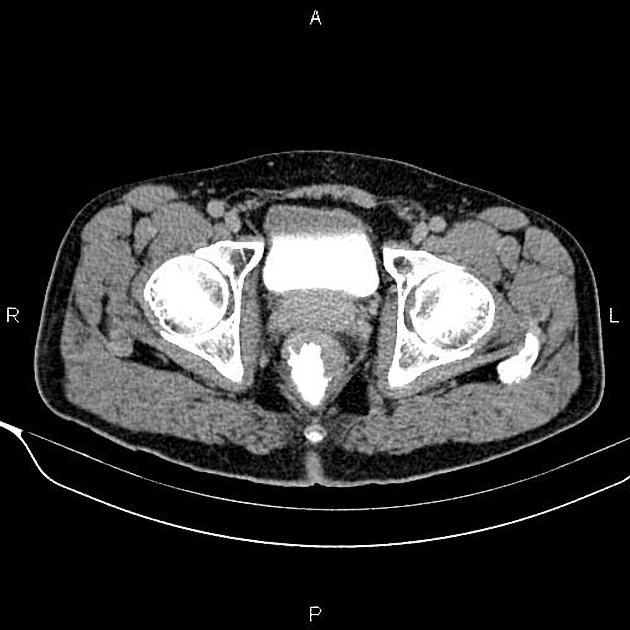
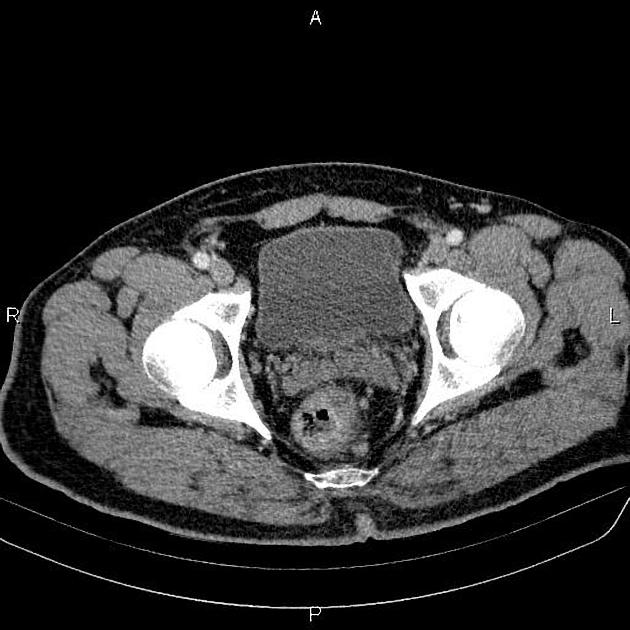
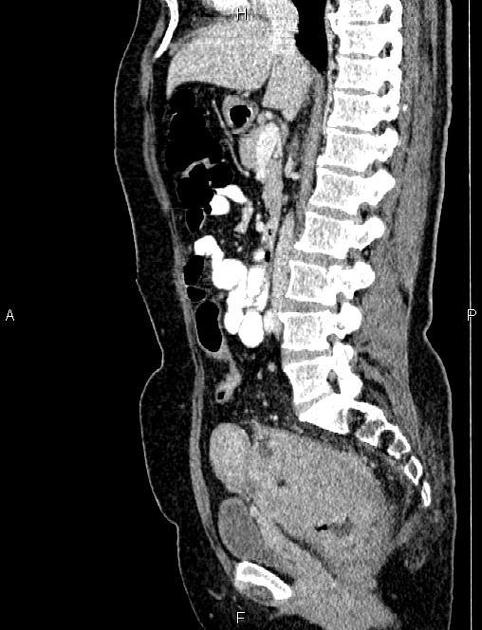
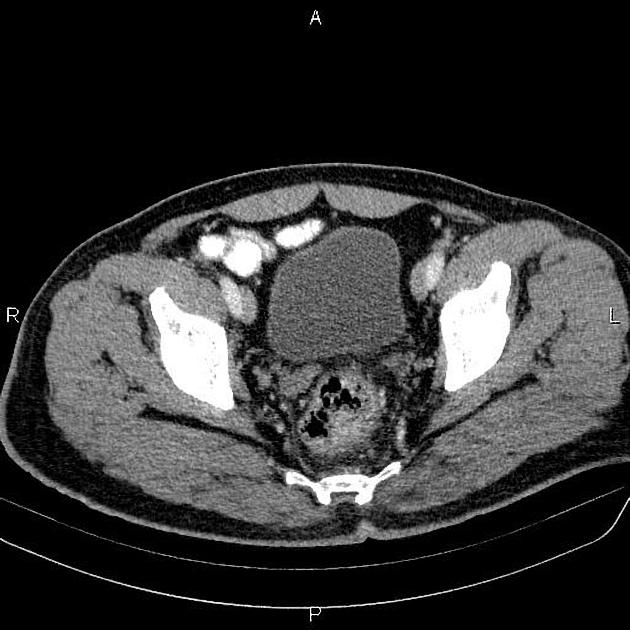
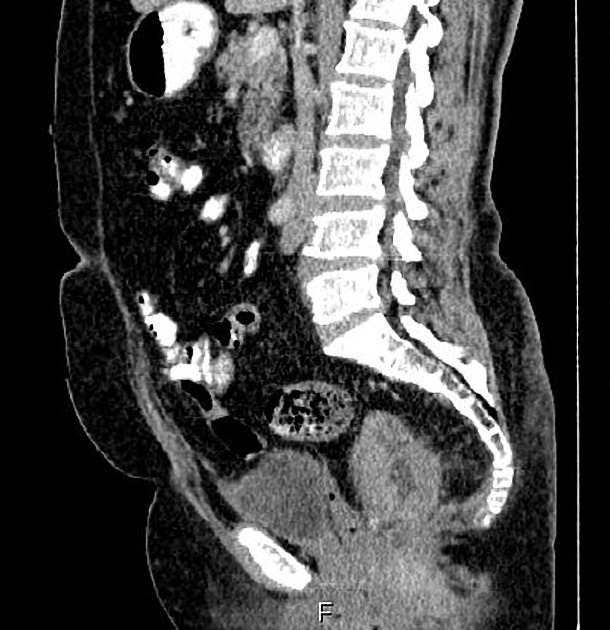
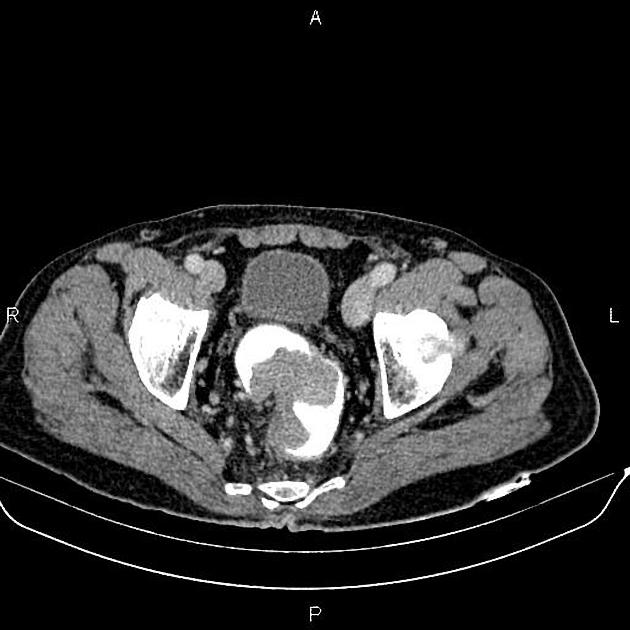
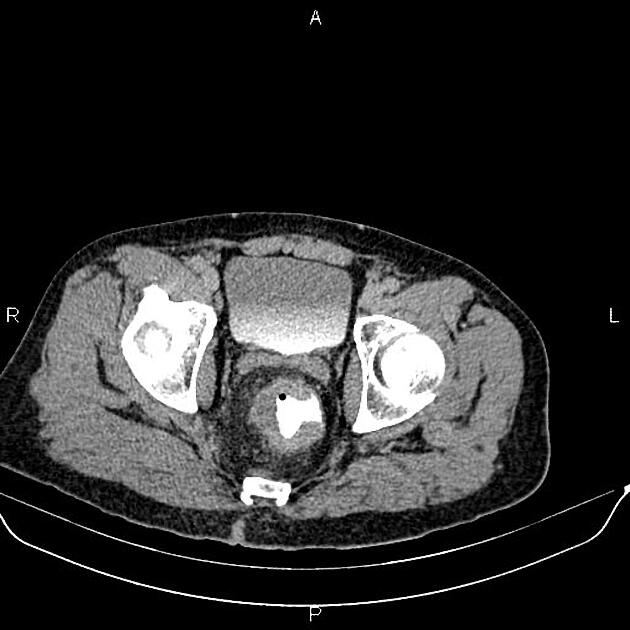
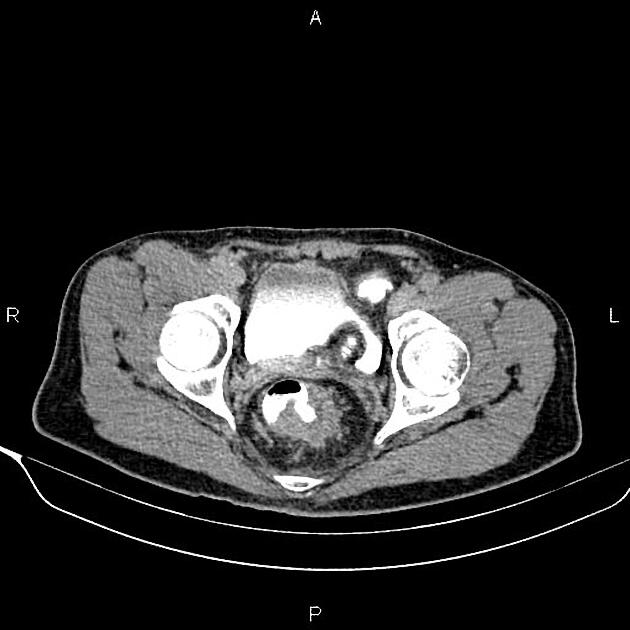
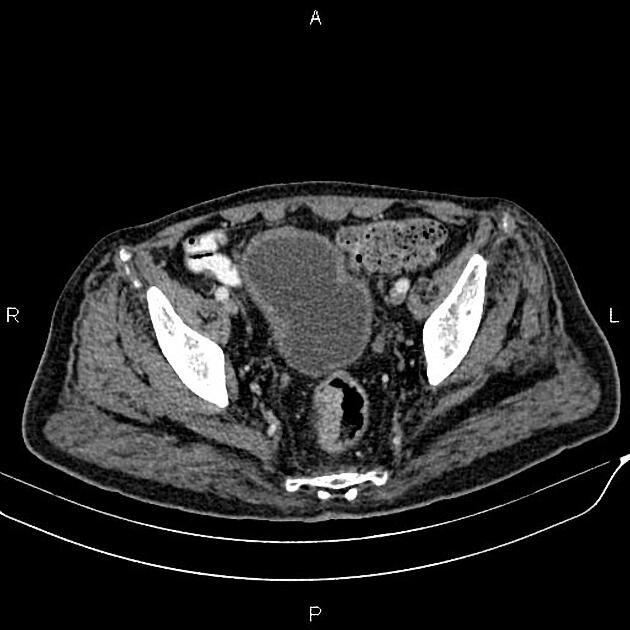
Although CT can diagnose in more advanced cases, MRI has become the fundamental imaging modality for evaluation and staging due to better soft-tissue contrast. Endorectal ultrasound also has a role in the staging, particularly for assessment and differentiation between T1 and T2 disease, but is not commonly performed by a radiologist.
MRI may be performed for:
-
diagnosis and/or locoregional staging
helps evaluate which patients may benefit from neoadjuvant therapy (usually stage II and III) and for evaluating poor prognostic factors
helps surgical planning
assessment of the effectiveness/response of neoadjuvant therapy
monitoring for recurrence post-therapy
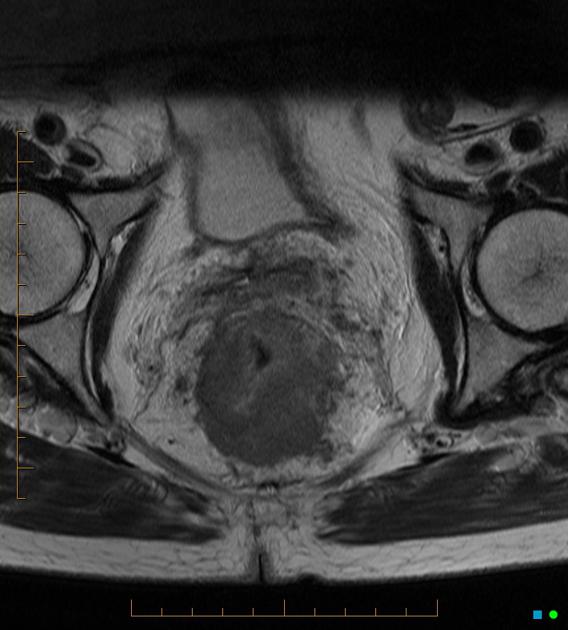
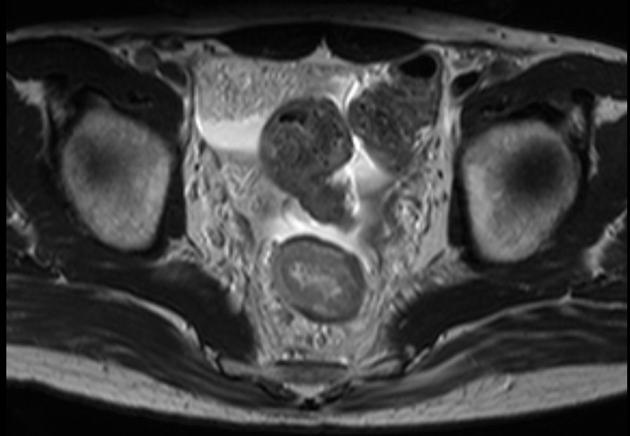
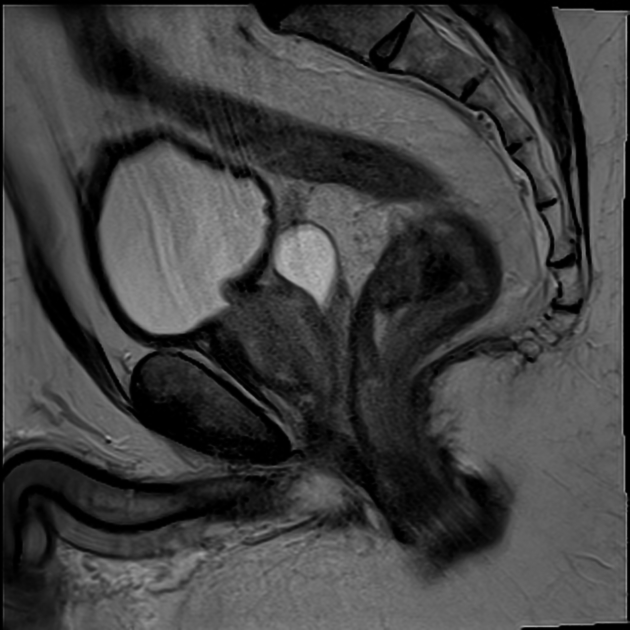
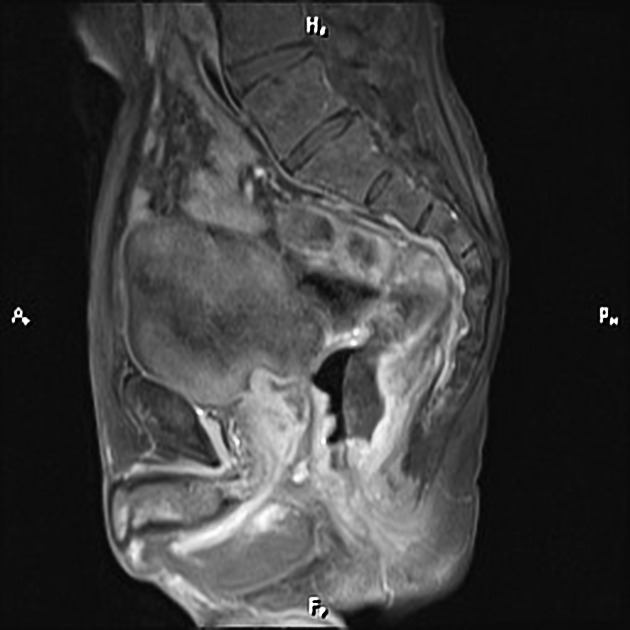
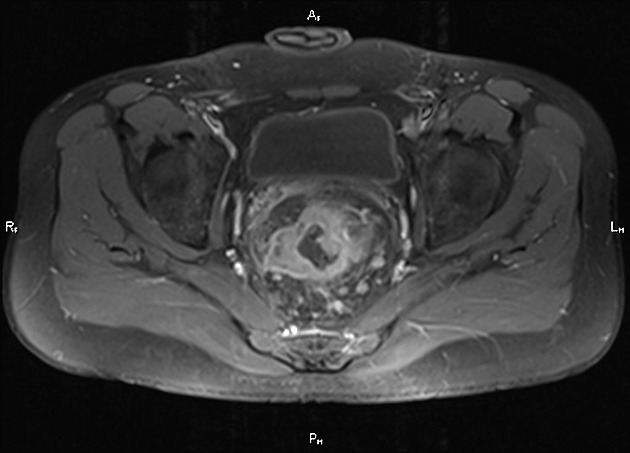
MRI
MRI is able not only to assess tumor stage but other important prognostic features such as extramural venous invasion (EMVI), tumor deposits and lymph node metastases. The key sequences are T2-weighted images parallel and perpendicular to the axis of the segment of the rectum containing the tumor. For more information, see MRI protocol for assessment of rectal cancer.
Factors to be assessed and described on MRI report:
morphology of primary tumor: semi-annular/circumferential/ulcerating/polypoidal/villous/eroding/mucinous/signet/cannot be assessed
invading edge of tumor (e.g. x o'clock to y o'clock)
distance of distal edge from the anal verge
distance of distal edge from puborectalis sling
longitudinal extent
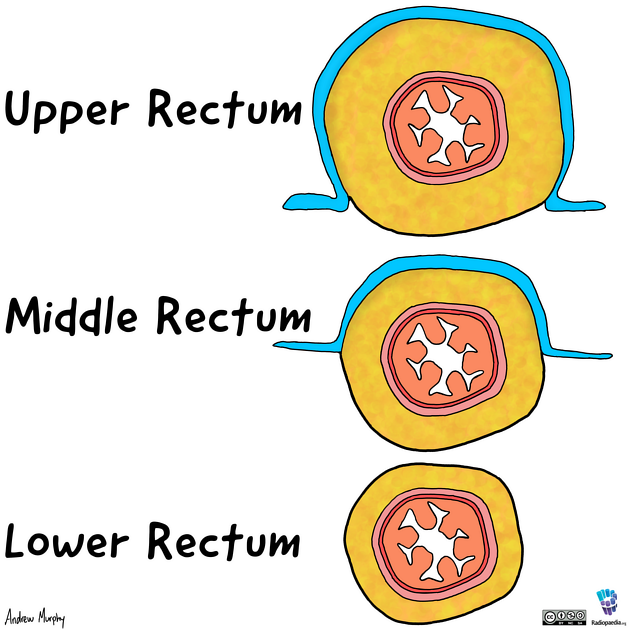
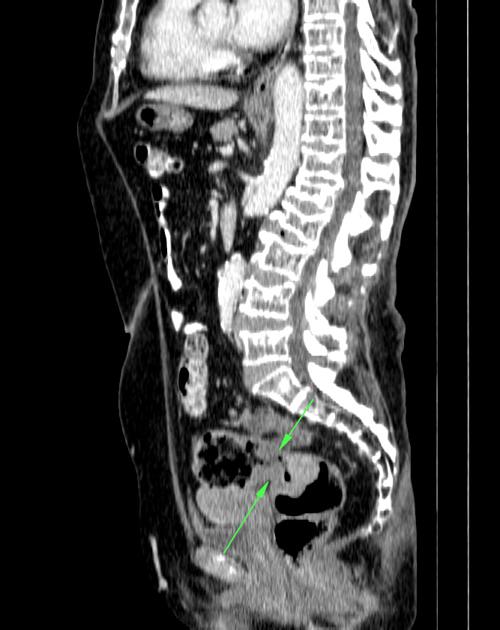
confirmation that the tumor is distal to the sigmoid take-off; this is the definition of the rectosigmoid junction and is identified by the point at which the bowel assumes a horizontal path on the sagittal images, moving away from the sacrum 14
whether it lies above or below the peritoneal reflection with approximate measurement, or whether it straddles and invades the peritoneal reflection
-
T stage
whether it is confined to or extends through the muscularis propria
extent of extramural spread (T3 disease) and whether peritoneum (T4a) or other organs (T4b) are invaded
distance from the mesorectal fascia
presence of tumor deposits
-
N (locoregional) stage
combination of size (short axis diameter) and morphologic criteria used for regional nodes 17
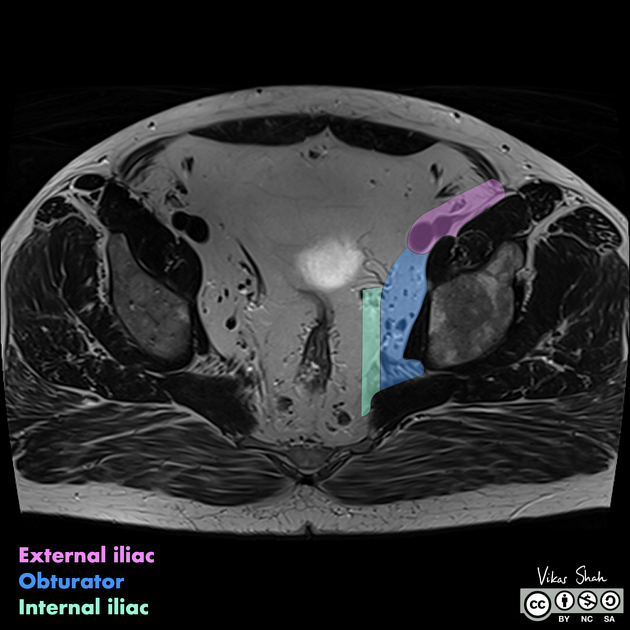
for tumors above dentate line, mesorectal, superior rectal, inferior mesenteric, internal iliac and obturator nodes are regional, with the latter two areas known as 'lateral' or pelvic sidewall 18
see staging article for more details
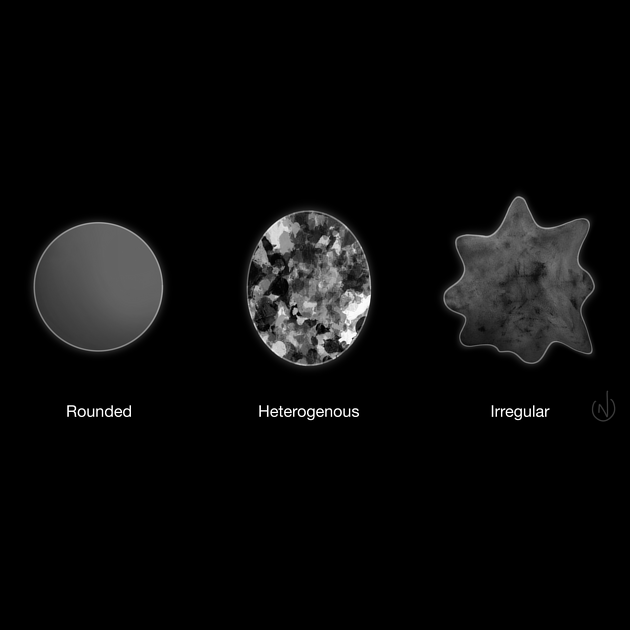
irregular or spiculated margin, heterogeneous signal intensity and round shape are suspicious characteristics
number of nodes
closest node to the mesorectal fascia
lateral/pelvic sidewall nodes: assess size, see staging article for more details
evidence of peritoneal nodal involvement
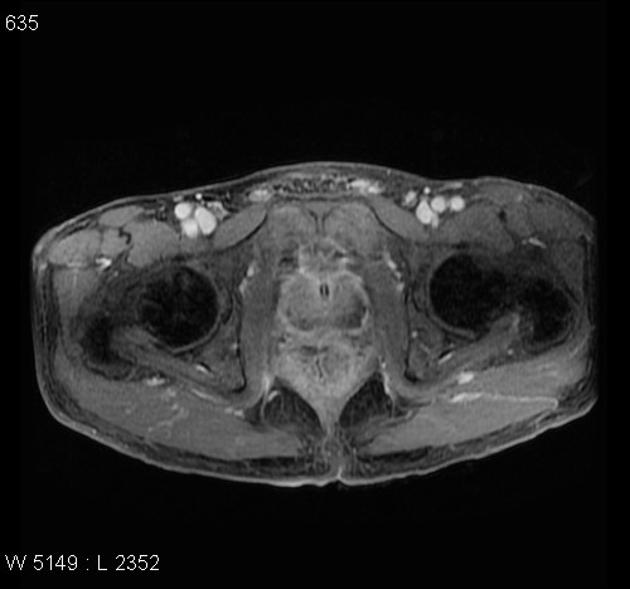
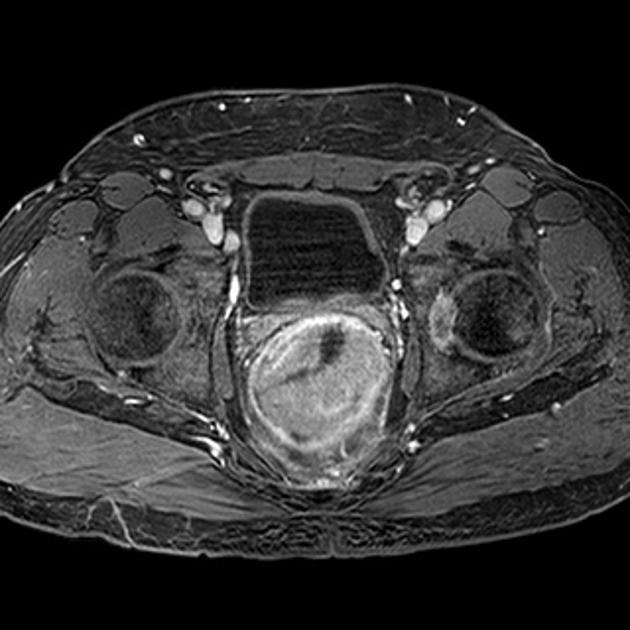
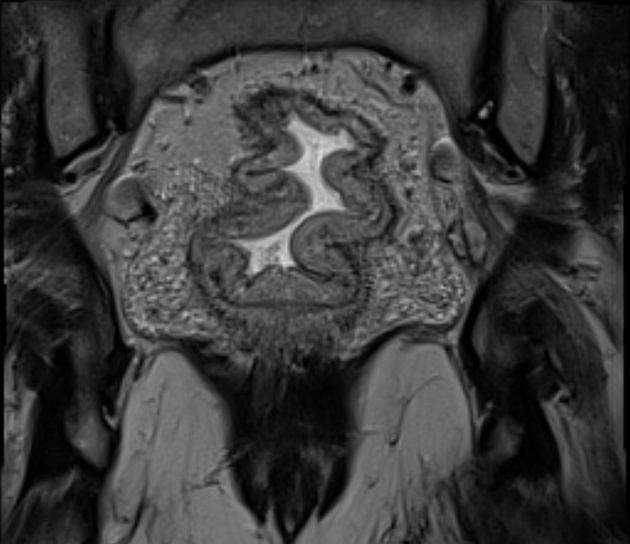
Signet ring cell cancer has a specific pattern of findings on MRI. Because of the submucosal growth and abundant intracytoplasmic mucin, these tumors tend to be long with preservation of the mucosa, and with a high signal on T2 weighted imaging 12. Low signal fibrotic change adjacent to the muscularis propria is due to local desmoplastic reaction. The findings referred to as rectal linitis plastic 16. Involved nodes, tumor deposits, and EMVI may have a similar high signal to the primary tumor.
Please refer to the article on rectal cancer staging for further details on how to apply and report the TNM staging on imaging.
Treatment and prognosis
The mainstay of treatment is surgical excision, however preoperative down-staging with either radiotherapy alone (more common in Europe) or combined chemo-radiotherapy (more common in the US) is employed in T3 and/or N1 disease (see rectal cancer staging) 1.
Depending on the stage at the time of resection local recurrence rates vary from 3-32% 1 with overall good 5-year survival in T1 and T2 tumors (85-100% and 70% respectively) 1,2,5. Some focal T1 lesions are candidates for transanal endoscopic microsurgery.
The majority of local recurrences occur within 20-36 months 2,5, have positive resection margins, and have a major impact on prognosis, with 80-90% of these patients succumbing to the disease within 5 years 4.
Some authors suggest that a circumferential resection margin (CRM) of less than 1 or 2 mm (the exact cut-off is debated) confers a poorer prognosis and patients should be considered for neoadjuvant treatment 6.



















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.