Renal infarction results from interruption of the normal blood supply to part of, or to the whole kidney. The main imaging differential diagnosis includes pyelonephritis and renal tumors.
On this page:
Epidemiology
The demographics of affected patients will depend on the underlying cause, although as most cases are the result of atherosclerosis and thromboembolism, most patients are older patients.
Clinical presentation
Small renal infarcts are often asymptomatic, and evidence of their prior occurrence only found on imaging at a later stage. When larger, patients typically present with acute flank pain and may have hematuria and proteinuria 4.
Pathology
Etiology
The causes of renal infarction include 1,2,4:
-
most common
from heart valve, ventricular or atrial thrombus, aorta
-
-
renal artery occlusion is considered a grade V renal injury
iatrogenic (e.g. angiography)
-
rare
seen in infancy secondary to severe dehydration (e.g. gastroenteritis)
in adults, even complete sudden occlusion of the renal vein usually does not result in infarction
torsion of transplant kidney 5
Radiographic features
Although historically plain radiographs intravenous pyelograms (IVP) with tomography were the mainstay of imaging the kidneys, today CT IVP has become the modality of choice and can image nephrolithiasis exquisitely as well as assess the renal vessels and parenchyma.
Ultrasound
Although CT is usually the first investigation of choice, ultrasound may be performed if the clinical presentation is vague.
In such cases, acute infarction will appear as an absence of perfusion on color Doppler examination. There will be a complete absence of perfusion when the entire kidney is affected, or it may be patchy if segmental arteries are involved 6. The absence of flow may also be directly visualized in the renal artery and, in rare cases of venous thrombosis causing infarction, the renal vein 6.
Over time the regions of infarctions shrink, becoming hyperechoic scars 6.
Contrast-enhanced ultrasound may be useful to detect or confirm a diagnosis of renal infarction. Infarcts will appear as wedge-shaped regions of nonperfusion 7.
CT
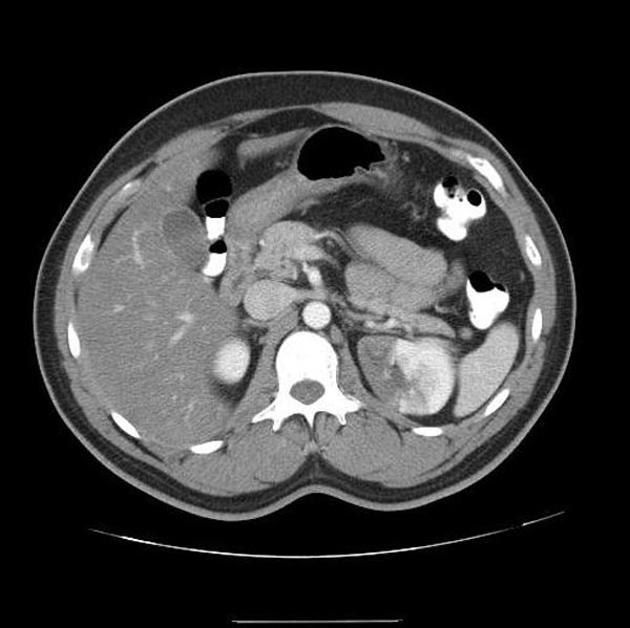
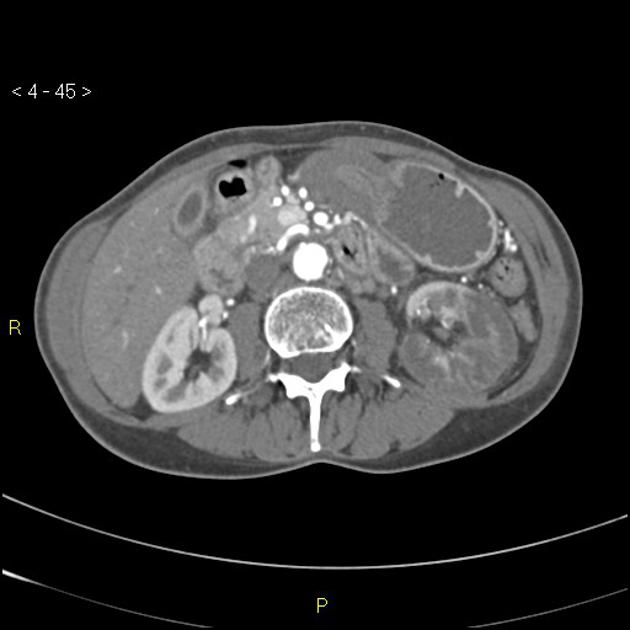
In patients who present with atraumatic flank pain with or without hematuria, a CT KUB is often the first test obtained as the differential is renal colic. Acutely the diagnosis is difficult on non-contrast scans, which may only demonstrate subtle swelling and surrounding stranding 1.
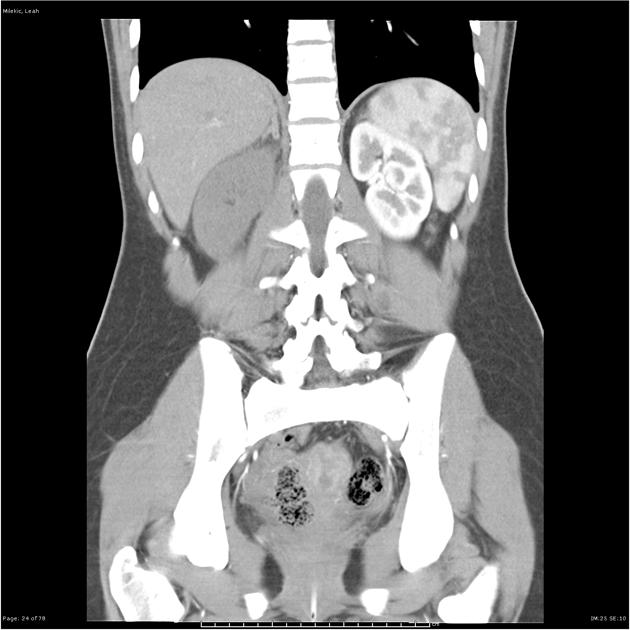
CT angiograms can visualize the occluded vessel. In the setting of trauma, it is important to assess for associated hematoma at the hilum which may indicate transection. Rarely the renal vein may also be occluded 2.
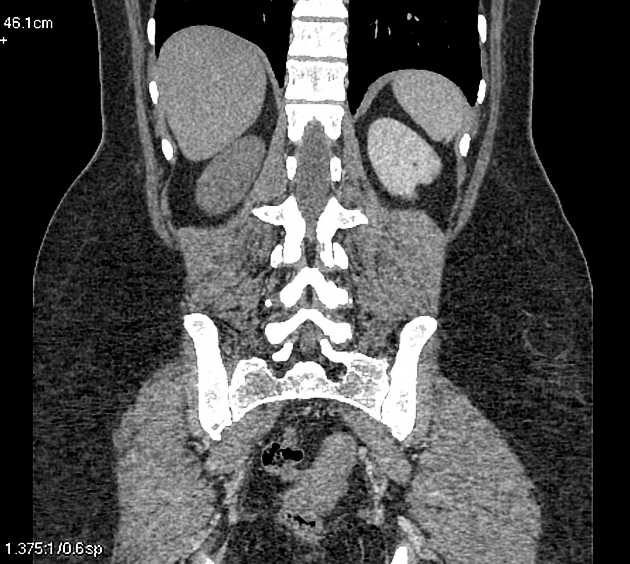
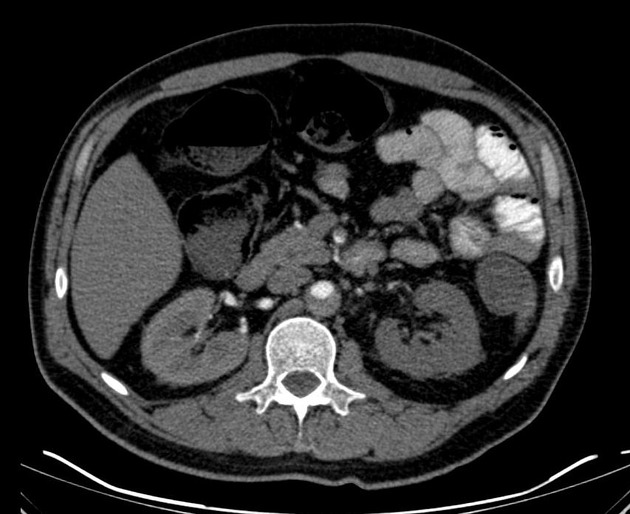
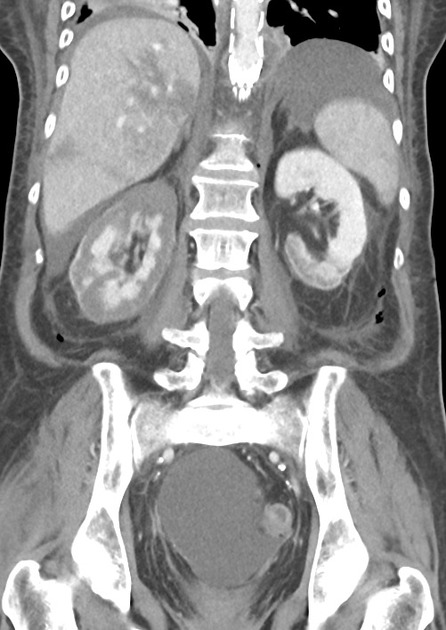
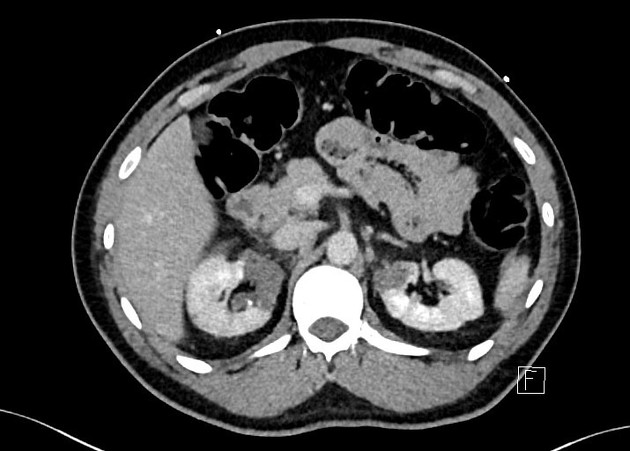
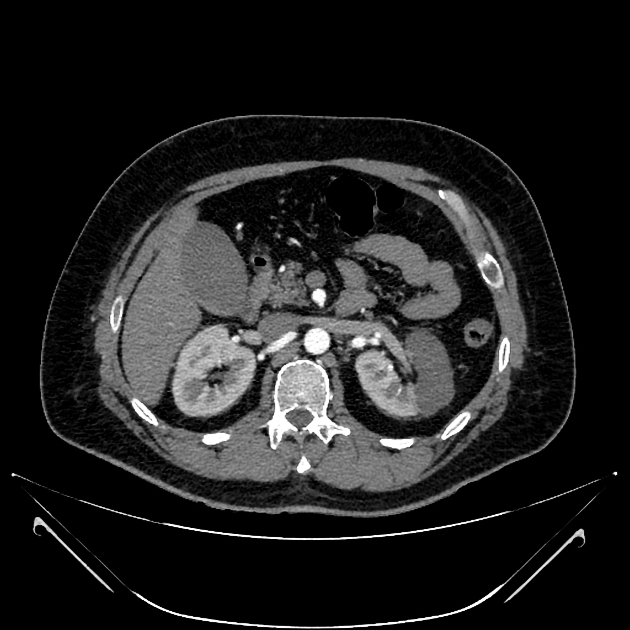
Renal infarcts are most easily identified on post contrast images, preferably in the cortical/arterial phase. One or more focal, wedge-shaped parenchymal defects that involve both the cortex and medulla and extend to the capsular surface are demonstrated 1. In cases where the main renal artery is occluded, then the entire kidney fails to enhance 2.
In ~50% of cases, a thin rim of cortex continues to enhance, due to collateral capsular perfusion 1-3. This is known as the cortical rim sign, and is not usually present immediately after infarction, but can be seen as early as 8 hours after occlusion (typically best seen several days later) 2,3.
Occasionally flip-flop enhancement can be seen, where a region of hypoenhancement on early phases becomes hyperattenuating on delayed imaging 3.
Treatment and prognosis
In cases where infarcts are segmental, only supportive management is required, and the cause of infarction investigated.
When complete occlusion of the renal artery is present, then attempts to revascularize the kidney can be made, although the results are disappointing, even in patients with short ischemic times 2. As such, unless patients have a solitary kidney or are premorbidly on the brink of renal failure, most renal artery occlusions are treated conservatively.
It should be noted that some post renal infarct patients who have remaining viable renal tissue but who develop renal arterial stenosis, may develop secondary renovascular hypertension, and may require endovascular intervention 2.
Differential diagnosis
The main differential is hypoenhancement due to infection (lobar nephronia / pyelonephritis). In these patients the cortical rim sign is absent, and presentation is often different, with inflammatory/infectious symptoms being prominent.











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.