Spinal arachnoid cysts are relatively uncommon and may be either intradural (type III meningeal cyst) or extradural (type IA meningeal cyst).
This article specifically focuses on spinal arachnoid cysts. For a general discussion of arachnoid cysts, refer to the main article: arachnoid cyst.
On this page:
Epidemiology
Spinal arachnoid cysts may present at any age. There is no gender predilection.
Clinical presentation
Most spinal arachnoid cysts are asymptomatic and are discovered incidentally. Clinical symptoms, if present, may include progressive spastic or flaccid paralysis, pain, weakness, numbness, and/or bladder/bowel incontinence. Symptoms may be exacerbated by postural changes and the Valsalva maneuver 13.
Pathology
As with any arachnoid cyst, spinal arachnoid cysts are CSF-filled sacs contained by the arachnoid mater. The degree of communication with the surrounding CSF space is variable with some cysts freely communicating and others not at all 9.
Etiology
They may be congenital or acquired. Secondary arachnoid cysts are usually due to trauma, hemorrhage, inflammation, surgery or iatrogenic injury like lumbar puncture, injection of anesthetic or contrast material within the subarachnoid space 3,4,13.
Location
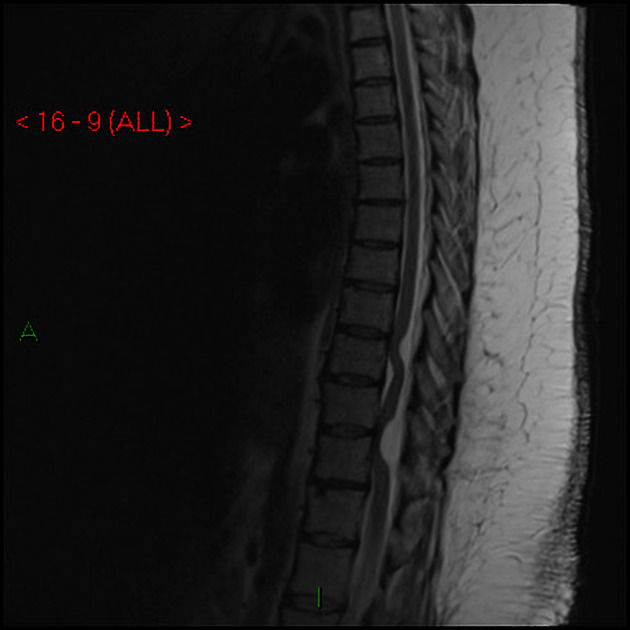
Most primary intradural spinal arachnoid cysts are dorsal to the cord. They occur at the following locations:
thoracic: 80%
cervical: 15%
lumbar: 5%
Secondary spinal arachnoid cysts can be located anywhere, depending on where the insult has occurred (see "Etiology" above).
Associations
spina bifida 10,11
syrinx 13
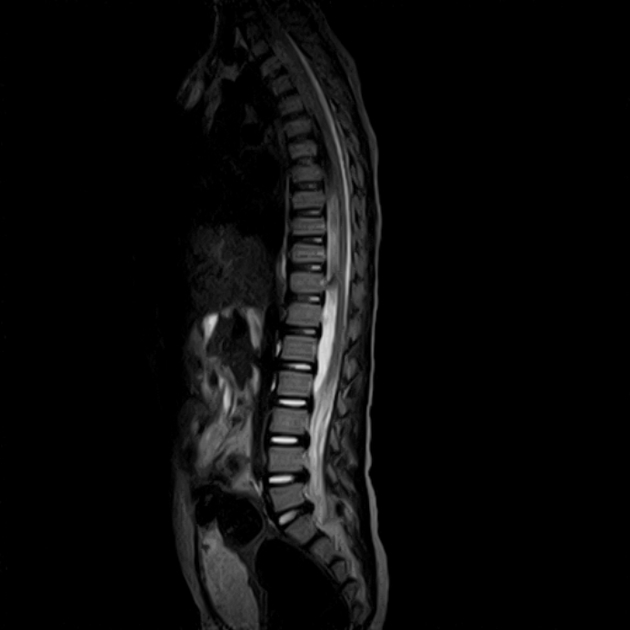
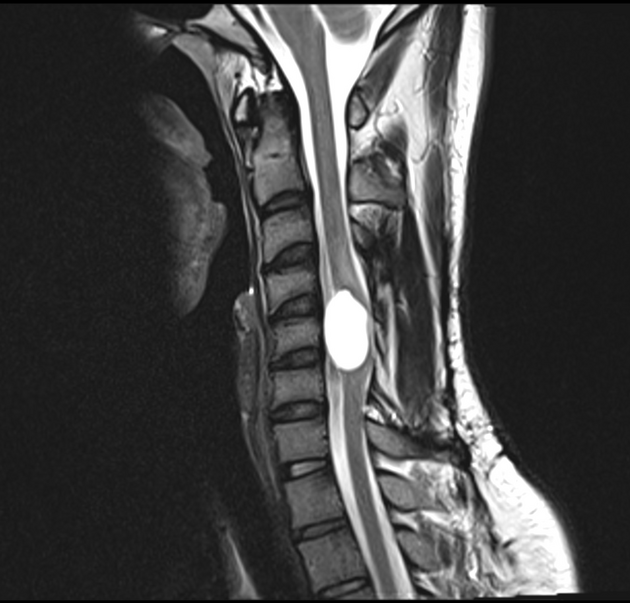
Radiographic features
CT
On CT myelography, the compressed cord is displaced anteriorly 3. Most arachnoid cysts eventually opacify with contrast, although the rate at which they do so is variable 7,9. In many instances, the cyst opacifies readily and as such, it may be challenging to diagnose with certainty. Early scanning is advisable, to 'catch' the cyst before it becomes isodense to CSF while considering the need for more delayed scanning if appropriate CSF mixing is not achieved. This may necessitate the introduction of contrast on the CT table rather than at fluoroscopy.
MRI
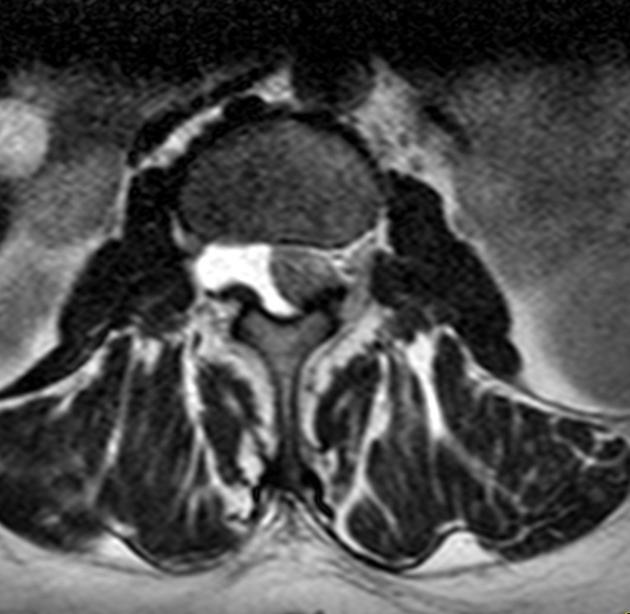
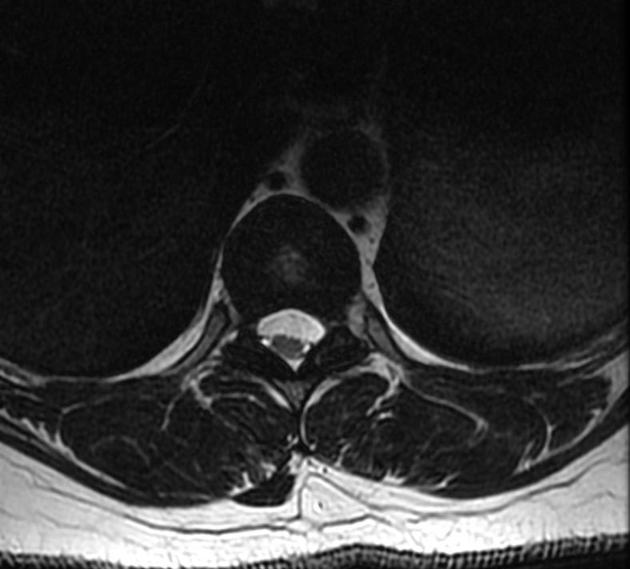
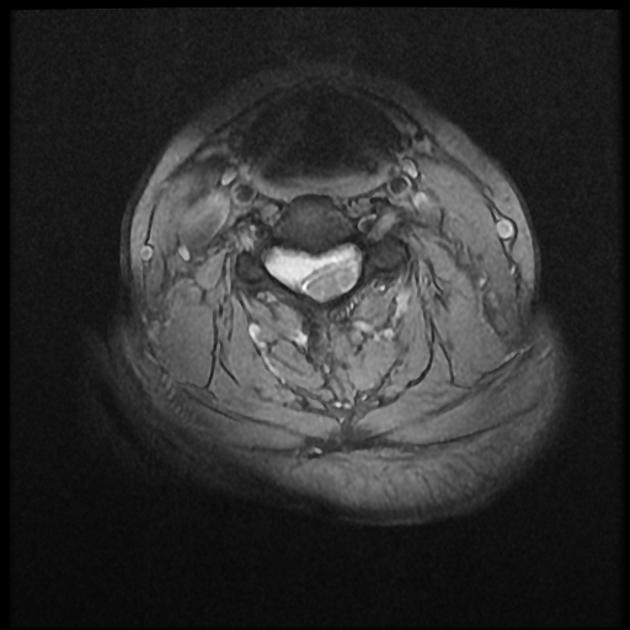
As the cysts follow the intensity of CSF and their walls are generally not visible, they may not be identified unless the cord is displaced.
T1: CSF intensity
T2: CSF intensity, may even be brighter than CSF since there is no signal loss from pulsation/flow 8
T1 C+ (Gd): no contrast enhancement
phase-contrast imaging: decreased CSF flow within the cyst 7
DWI: no evidence of restricted diffusion
Treatment and prognosis
Incidental asymptomatic cysts are managed conservatively. Symptomatic cysts can be treated with surgical excision. An important component of surgical treatment of epidural cysts includes closure of the arachnoid defect, if any, which could become a source of CSF leak.
Differential diagnosis
For intradural arachnoid cysts, several alternative diagnoses should be considered:
-
focal cord deformity
phase-contrast MRI: absence of CSF flow ventral to the herniated cord and a normal CSF flow pattern dorsal to the cord 7
can be challenging to distinguish; myelography may be helpful
-
bright on DWI (as in the brain, spinal epidermoids are differentiated from arachnoid cysts by their brightness on DWI)
-
most common location is the lumbar spine
imaging characteristics are variable but usually resemble fat 3
-
common in the lower cervical and upper thoracic spine ventrally
usually Indistinguishable from an arachnoid cyst on imaging 12
-
most commonly extradural (intradural extramedullary lesions are extremely rare)
usually multiloculated
may show minimal enhancement
-
spinal cysticercosis
peripheral enhancement
usually multiloculated
Rarely, extradural cysts may be considered, although they are generally clearly not within the dura. They include:











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.