Spinal astrocytomas are the second most common spinal cord tumor, representing 40% of intramedullary tumors 3. They account for 60% of pediatric intramedullary tumors, making them the most common spinal cord tumor in children 6.
This article specifically relates to spinal astrocytomas. For a discussion on intracranial astrocytomas and for a general discussion of the pathology refer to the main article: astrocytoma. Pilocytic astrocytomas and pleomorphic xanthoastrocytomas are also discussed separately.
On this page:
Epidemiology
The peak incidence of spinal astrocytomas occurs in the third decade, with the mean age at presentation being ~30 years. Males are affected somewhat more commonly than females (M: F = 3:2) 5.
Astrocytoma accounts for one-third of all spinal cord glioma tumors. It is also the most common intramedullary tumors in children 5.
Associations
There is an increased incidence in neurofibromatosis type 1 including high-grade astrocytoma with piloid features.
Clinical presentation
Clinical presentation is similar to that of other intramedullary spinal tumors, commonly consisting of pain, and sensory changes (53.6% of cases). Muscle weaknesses are seen in 41.4% of cases. Bowel and bladder dysfunction are uncommon 5.
Pathology
Astrocytomas (both intracranial and spinal) arise from astrocytic glial cells. Spinal cord astrocytomas generally have a lower histologic grade than astrocytomas in the brain (see grading of astrocytomas):
-
adults
low-grade: 75%
anaplastic astrocytoma: 25%
glioblastoma: ~1%
-
pediatric
in children <3 years, 80% are grade I or II 5
All astrocytomas are characterized by hypercellularity and the absence of a surrounding capsule. In contrast to cord ependymomas, a cleavage plane is not present in most intramedullary spinal astrocytomas.
High-grade tumors are more commonly associated with leptomeningeal spread, overall seen in up to 60% of spinal cord glioblastomas 5.
Location
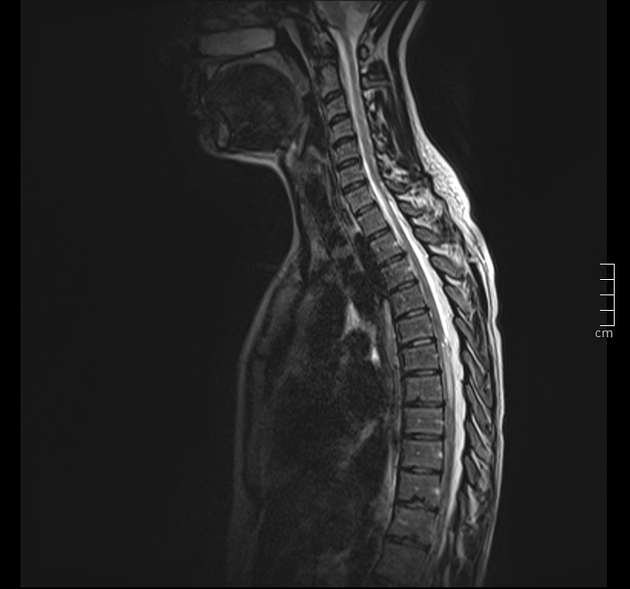
Spinal astrocytomas usually span multiple segments in craniocaudal extent, with an average length of involvement of 4-7 vertebral body segments 5,7.
Regarding their specific spinal location:
involvement of thoracic cord (67%), followed by cervical cord (49%), are most common. Tumor may, of course, involve both regions 5
involvement of entire spinal cord (holocord presentation) - more common in children than in adults
-
rare:
isolated conus medullaris involvement (3%)
isolated filum terminale 5 (more typical of myxopapillary ependymomas)
Radiographic features
Astrocytomas are typically intramedullary masses that diffusely expand the spinal cord. They usually span spinal multiple segments, as discussed above. Their slow outward growth tends to cause osseous remodeling of the spinal canal, which may be the only clue to their presence on x-ray or CT.
Plain radiograph/CT
The radiographic appearance of the spine can be normal; however, osseous remodeling at the level of the tumor may be seen as posterior vertebral body scalloping or thinning of the pedicle or laminae. Patients may present with scoliosis, especially in children presenting with holocord involvement 5. However, these features are less common compared to spinal ependymomas.
Expansion of the spinal cord is frequently visible on CT but can be subtle due to limited soft-tissue contrast resolution. Lesion conspicuity may be better on a contrast-enhanced study.
Myelography
Myelography may show non-specific multisegmental cord enlargement and may result in a block to normal flow of contrast past the lesion, although this is more common with ependymoma.
MRI
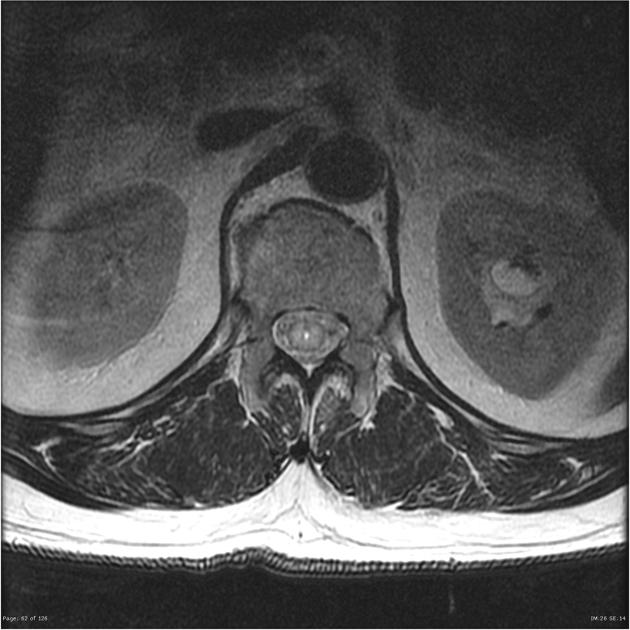
As astrocytomas arise from cord parenchyma (cf. ependymomas that arise in the central canal), they typically have an eccentric location within the spinal cord.
They may be exophytic and even appear largely extramedullary. They usually have poorly defined margins. Peritumoral edema is present in ~40%. Intratumoral cysts are present in ~20% and peritumoral cysts are present in ~15% 8. Unlike ependymomas, hemorrhage is uncommon.
Reported signal characteristics include
T1: isointense to hypointense
T2: hyperintense
-
T1 C+ (Gd)
vast majority enhance (previously thought to be universally enhancing 8)
usually patchy enhancement pattern
Treatment and prognosis
Astrocytomas are generally faster growing than ependymomas and have a worse prognosis.
Surgical excision is usually the treatment of choice; however, due to the infiltrative nature of astrocytomas, resection is almost always histologically incomplete.
Cord astrocytomas in children tend to be associated with a good prognosis, as they behave much like grade I cerebellar pilocytic astrocytomas and displace neural tissue rather than infiltrate it.
Differential diagnosis
The main differential diagnosis is a spinal ependymoma. Certain imaging features may help to differentiate between the two, which are covered in this article:
-
more common in adults
scoliosis and bony remodeling more common
central location in spinal canal
well-circumscribed
-
hemorrhage is common
may rarely present as a subarachnoid hemorrhage
hemosiderin staining, especially at the superior and inferior margins (so-called hemosiderin capping), is common
focal, intense homogeneous contrast enhancement
more frequent and more prominent cysts (intratumoral and polar)










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.