Sturge-Weber syndrome, also known as encephalotrigeminal angiomatosis or encephalofacial angiomatosis, is a phakomatosis characterised by facial port-wine naevus (capillary malformation) and pial angiomas. It is part of a wide spectrum of possible cerebrofacial arteriovenous metameric syndrome (CAMS) phenotypes.
On this page:
Epidemiology
Sturge-Weber syndrome is rare, with an incidence estimated at 1 in 20,000-50,000 11.
Associations
Clinical presentation
The diagnosis is usually evident due to a congenital facial cutaneous capillary malformation, also known as port-wine naevus (previously port-wine stain) or facial naevus flammeus. This feature is almost always present and usually involves the ophthalmic division (V1) of the trigeminal nerve 3; if this territory is not involved, Sturge-Weber syndrome is unlikely 10. In ~5%, intracranial involvement is present without associated cutaneous naevus 1,2. In most cases (~70%), the naevus is unilateral and ipsilateral to the intracranial abnormality.
The most common clinical manifestation is with childhood seizures, present in ~80% (range 71-89%) of cases 2, which is often refractory to medical therapy 1. These usually begin in the first few years of life and are often associated with developmental delay and hemispheric symptoms including hemiplegia/hemiparesis and hemianopsia.
Approximately a third of patients have choroidal or scleral angiomatous involvement, which may be complicated by retinal detachment, buphthalmos or glaucoma 1.
Pathology
The leptomeningeal angiomatosis results in a vascular steal affecting the subjacent cortex and white matter producing localised ischaemia. In about 80% of the cases, there is unihemispheric involvement.
Classification
According to Roach et al. 23, Sturge-Weber syndrome can be classified according to the presence/absence of facial and leptomeningeal angiomas:
type I: represents the classic syndrome, with both facial and leptomeningeal angiomas; may have glaucoma
type II: facial angioma without evidence of intracranial disease; may have glaucoma
type III: isolated leptomeningeal angioma; usually no glaucoma
However, this classification system has been criticised as it suggests that all patients with facial capillary malformations have Sturge-Weber syndrome, even in the absence of brain or eye involvement (type II), which does not appear to be the case 24.
Genetics
Unlike most phakomatoses, Sturge-Weber syndrome is sporadic with no definite identifiable hereditary component 4,10. An associated gene mutation has been identified with a nucleotide transition in GNAQ on chromosome 9q21 12.
Radiographic features
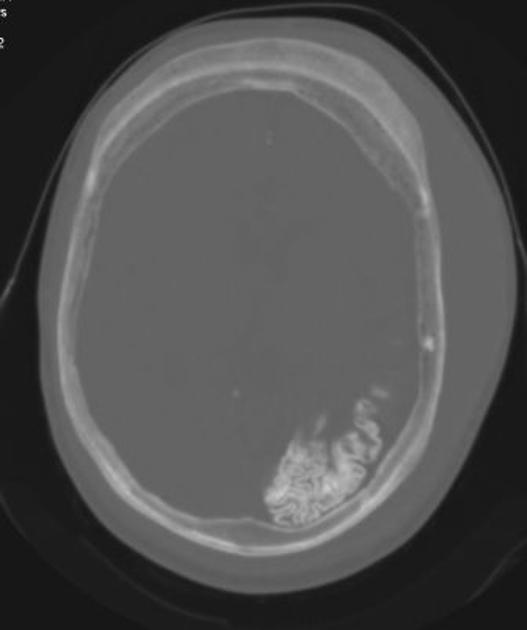
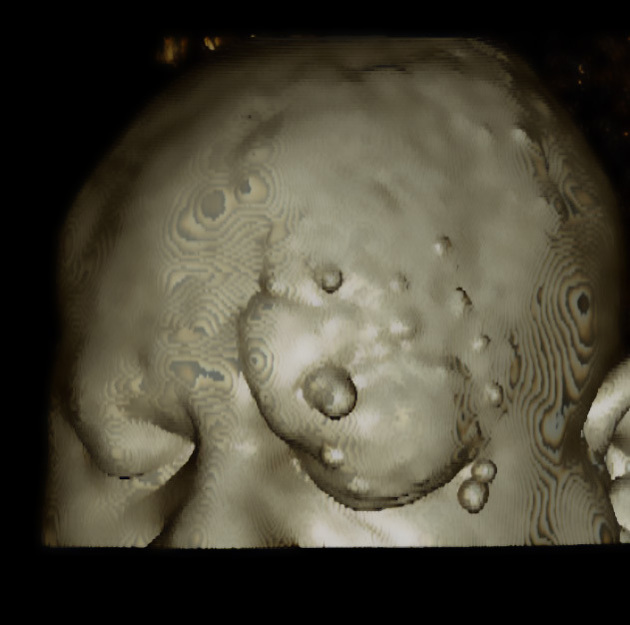
Plain radiograph
Skull radiographs were historically useful and capable of identifying the gyriform calcification of the subcortical white matter although they no longer play a significant role in the diagnosis or management of this condition. The finding usually becomes evident between 2-7 years of age 2.
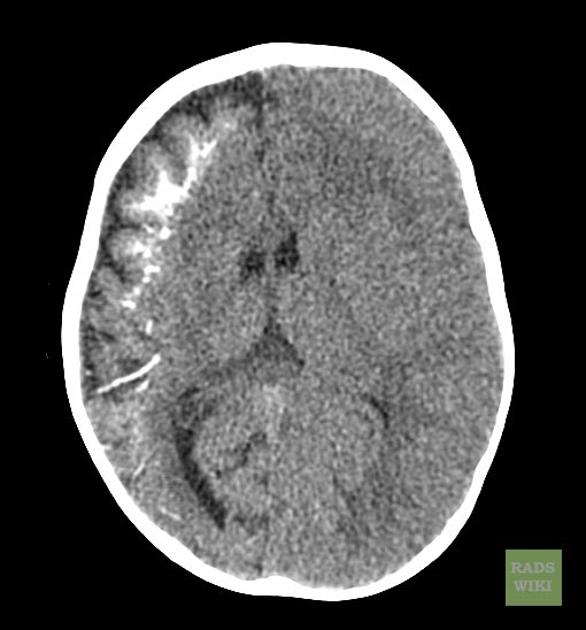
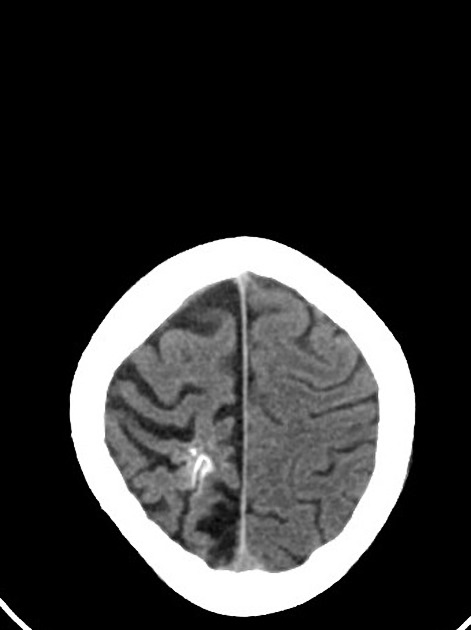
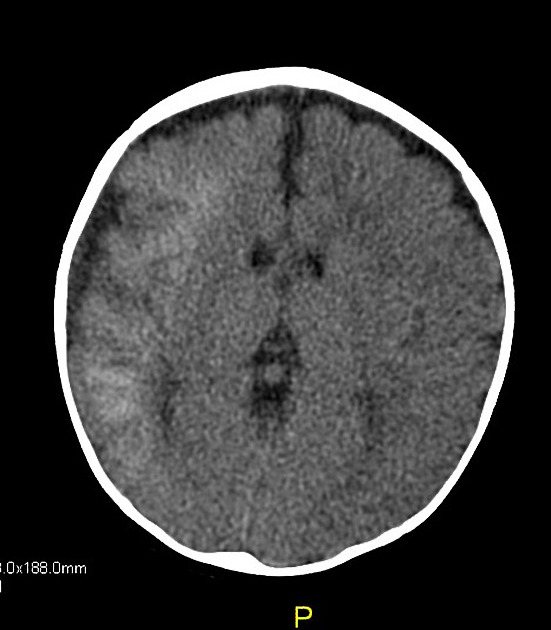
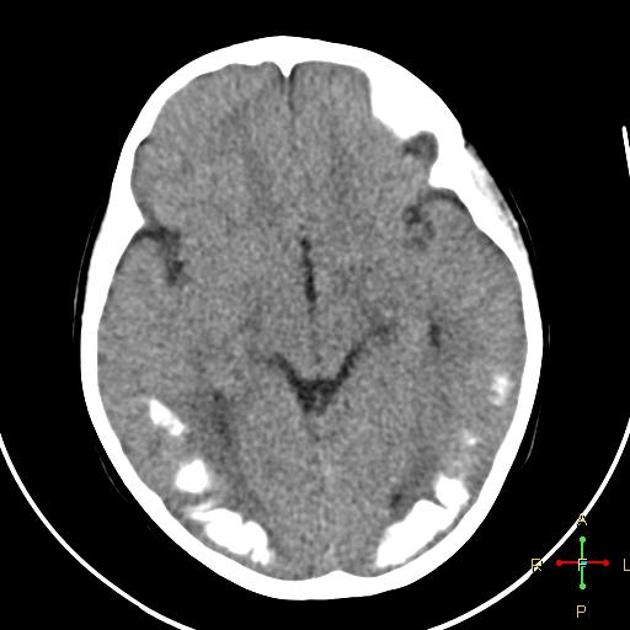
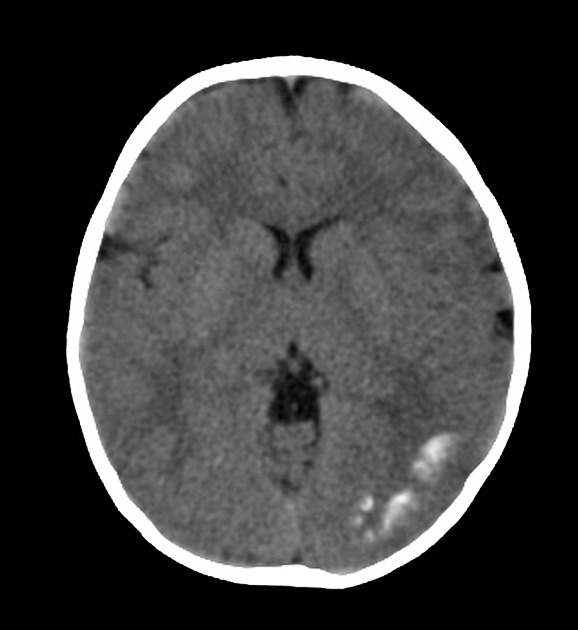
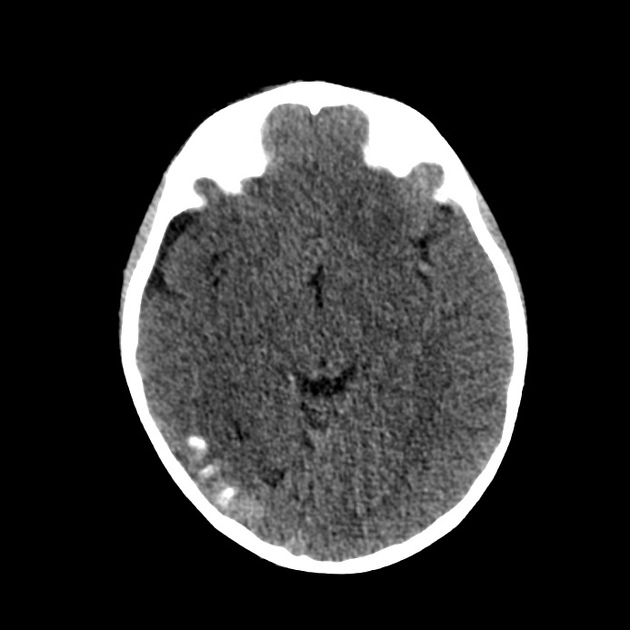
CT
subcortical calcification (seen at an earlier age than plain film) and associated parenchymal volume loss
tram-track sign of cortical and subcortical calcification 13,14
calvarial and regional sinus enlargement may be evident
ipsilateral choroid plexus may be enlarged
in severe cases, a Dyke-Davidoff-Masson appearance may be seen
orbital choroidal haemangiomas may be present
asymmetric cavernous sinus enlargement 22
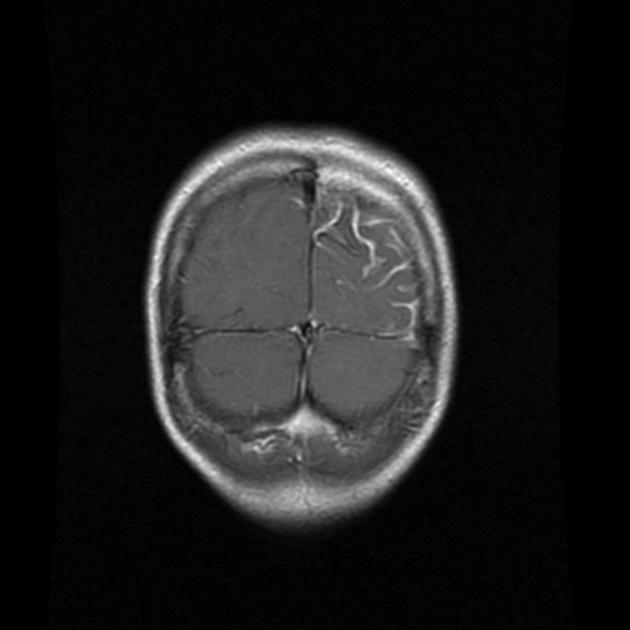
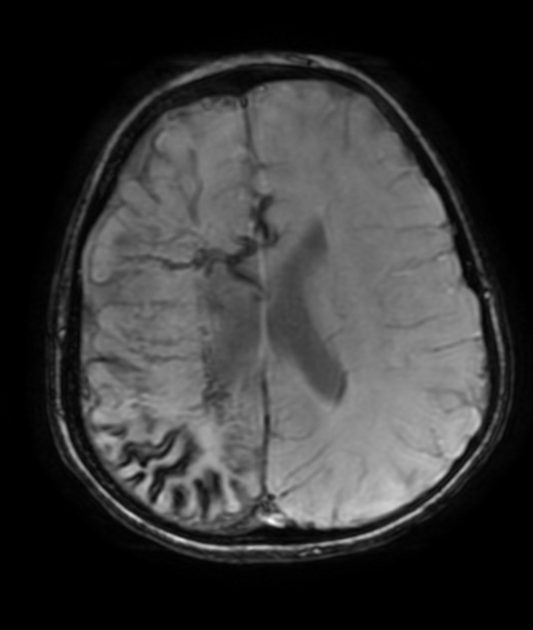
MRI
T1: signal of the affected region is largely normal, with anatomic volume loss evident at an older age
-
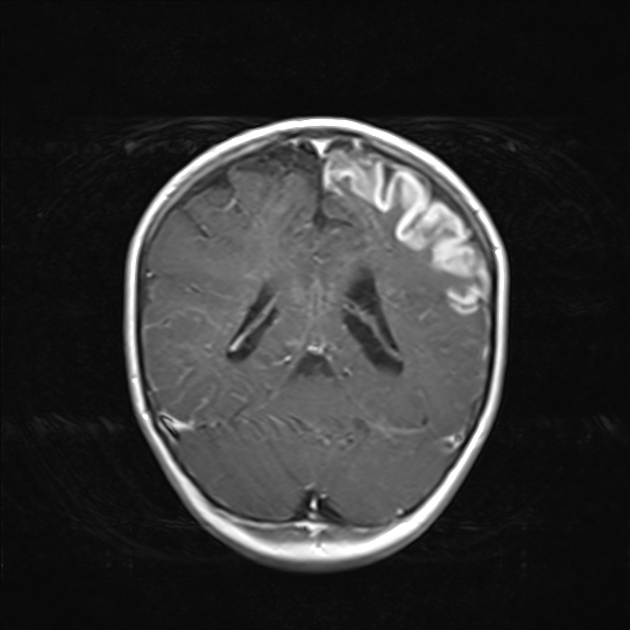
T1 C+ (Gd)
prominent leptomeningeal enhancement in the affected area (due to congested internal cerebral veins, a manifestation of the so-called "pial angiomatosis", resulting in venous congestive ischaemia with infarction and obliteration of cerebral parenchyma)
much later in life, the angioma may "burn out", losing enhancement 1
enlarged ipsilateral choroid plexus
dilatation of transparenchymal veins that communicates between the superficial and deep venous systems
-
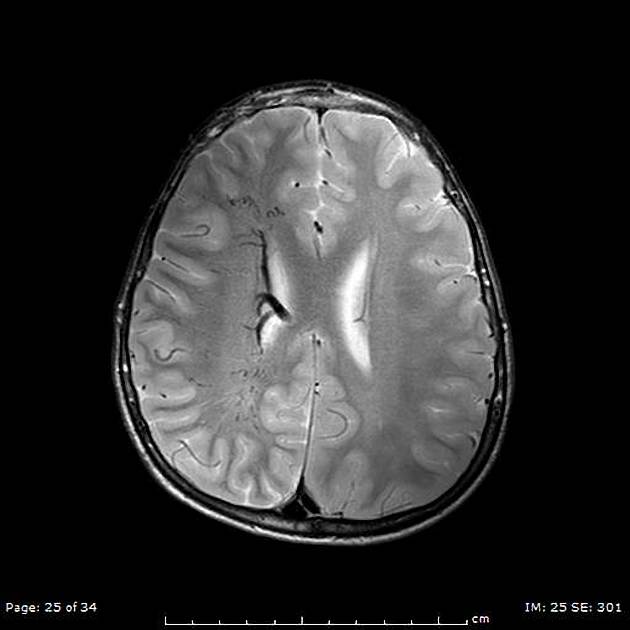
T2
-
low signal in white matter subjacent to angioma representing
postulated accelerated myelination in neonate 1
calcification later in life
abnormal deep venous drainage seen as flow voids
-
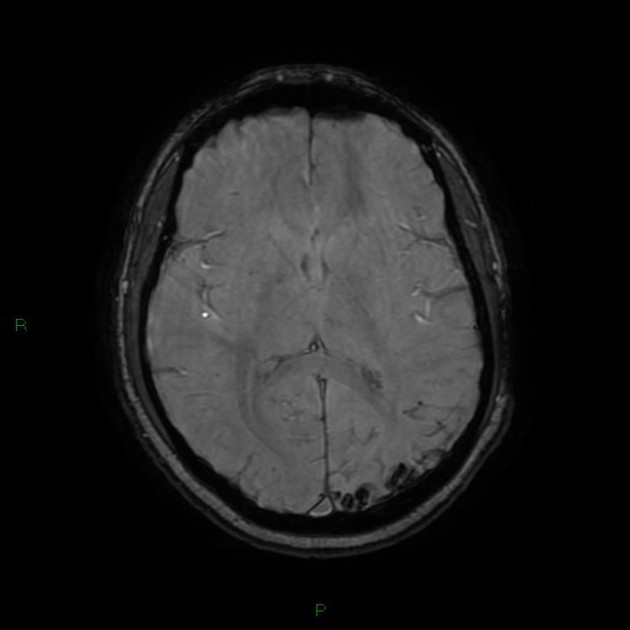
GE/SWI/EPI: sensitive to calcification, seen as regions of signal dropout
MR spectroscopy: decreased NAA 6
Angiography (DSA)
In most cases (82%), angiography is abnormal and demonstrates absent superficial cortical veins with abnormal and enlarged deep venous drainage 2.
Treatment and prognosis
Treatment revolves primarily around seizure control, with surgical resection only indicated rarely in refractory cases. An ophthalmological examination is also essential to identify and treat ocular involvement 3.
History and etymology
Sturge-Weber syndrome was first described by Sturge in 1879 who argued that there was a direct link between the intracranial haemangioma and the clinical presentation, although this was not accepted by his medical peers. It took until 1901 for Kalischer to provide the pathological confirmation that the pial angioma caused the neurological sequelae 20.
In 1912 Weber and Volland described the intracranial calcification. Radiographic identification of cerebral calcification was first described by Dimitri in 1922 2,18,20. In fact, Schirmer described a male patient with a facial naevus and buphthalmos in 1860, however, he did not recognise that it was a neurological condition 20.
William Allen Sturge: English physician (1850-1919) 16,18,20
-
Frederick Parkes Weber: English dermatologist (1863-1962) 17,19
five different diseases are named after Dr Weber! 19
Vincente Dimitri: Austrian dermatologist (1885-1955) 18
Rudolf Schirmer: German ophthalmologist (1831-1896) 20
Siegfried Kalischer: German neuropathologist (1862-1954) 20,21
Differential diagnosis
The differential is a combination of that for multiple intracranial calcifications, cerebral hemiatrophy and leptomeningeal enhancement, and therefore includes:










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.