TIPS evaluation is useful to ensure that a transjugular intrahepatic portosystemic shunt (TIPS) is working properly and that no stenosis has occurred within the stent. Ultrasound is often used as a first-line modality.
Radiographic features
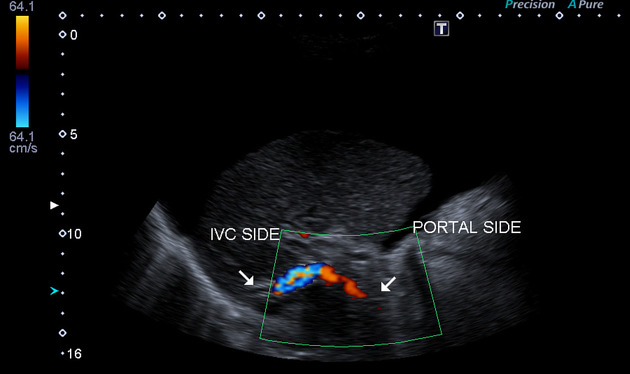
Ultrasound
The normal TIPS should show color Doppler flow throughout its length. The in-stent velocities are typically higher than in a native portal vein 1.
Trending stent velocities over multiple exams adds specificity to a single evaluation. If there is a concern for a stenosis based on a combination of abnormal findings, venography can be pursued.
Normal
normal TIPS velocity: 90-190 cm/s
normal portal vein velocity before entering the TIPS: ~30 cm/s
phasic waveform
the portal vein branches normally reverse their flow into the shunt
Stenosis
color Doppler aliasing at the site of the stenosis
velocity of >190 cm/s at a stenotic segment
velocity of <90 cm/s in non-stenotic segments
velocity <30 cm/s in the pre-stent portal vein (accessory sign)
complete occlusion: lack of color Doppler flow
return of antegrade portal branch flow previously retrograde towards TIPS.
Always be sure to thoroughly evaluate the hepatic vein distal to the stent as well.
3D and 4D ultrasound techniques to evaluate TIPS flow volumes are being developed as a possible improvement over using velocities 3.
Contrast-enhanced ultrasound (CEUS) is also being evaluated as a tool to improve non-invasive assessment of TIPS 8.
Venography
Non-invasive investigations are usually effective at assessing the patency and flow of the TIPS shunt 5. In case of inconclusive results after US or cross-sectional imaging and in the appropriate clinical settings (e.g. suspicion of thrombosis or significant in-stent stenosis in patient with recurrent bleeding after TIPS) an invasive interrogation of the tract might be necessary.
The shunt is cannulated using usually a right internal jugular vein access. A non-selective angiographic catheter (e.g. 5 Fr pigtail) should be advanced in the portal vein, in order to confirm antegrade flow through the stent via the hepatic vein into the right atrium: this allows to evaluate for shunt thrombosis or stenosis 6.
Portal venography also characterizes the dynamic flow distribution between the splenoportal axis, and portosystemic or portoazygos shunts. After a successful TIPS, there should not be preferential filling of such shunts feeding gastric varices.
CT
Studies have investigated whether CT can be used to assess TIPS patency and stenosis 7. However, most centers continue to rely on ultrasound +/- venography as the mainstay 8.
Practical points
when using color Doppler ultrasound for evaluation, remember to take angle correction into account to avoid false positives; if there is an area of the TIPS without color flow, make sure the TIPS is not approaching 90° relative to the transducer
patency of covered TIPS stents is better than bare metal stents and many centers do not evaluate them on a regular schedule, only when there is a suspicion for stent failure
recently placed TIPS stents often contain a small amount of gas in the wall of the stent, so if a baseline ultrasound exam is desired, consider waiting a week for the gas to resorb before imaging




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.