Uterine leiomyomas, also known as uterine fibroids, are benign tumours of myometrial origin and are the most common solid benign uterine neoplasms. They are a common incidental finding on imaging and rarely cause diagnostic dilemma.
On this page:
Epidemiology
They are clinically apparent in ~25% of women of reproductive age and over 70% of women by menopause 21. Fibroids are responsive to hormones (e.g. stimulated by oestrogens). Being rare in prepubertal females, they commonly accelerate in growth during pregnancy and involute with menopause 1.
Risk factors
2-3x increased incidence in Black women than in White women 20,21
increasing incidence with age: 10x more common between 41-60 years of age compared to 21-30 years of age, reaching a peak at 50-60 years 20,21
3x increased incidence with a family history of uterine fibroids 21
Clinical presentation
They are often asymptomatic and discovered incidentally. Signs and symptoms associated with fibroids include:
abnormal vaginal bleeding
pain
palpable masses
Pathology
Leiomyomas are benign monoclonal tumours 16 predominantly composed of smooth muscle cells with variable amounts of fibrous connective tissue. They are commonly multiple (~85% 8), and range significantly in size.
Any fibroid may undergo atrophy, internal haemorrhage, fibrosis, and calcification. They can also undergo several types of degeneration:
hyaline degeneration: focal or generalised hyalinisation: this is the most common type of degeneration (can occur in ~60% of cases) 6
cystic degeneration: ~5%
myxoid degeneration: generally considered uncommon although reported as high as 50% by some authors 14
red (carneous) degeneration: due to haemorrhagic infarction, which can occur particularly during pregnancy, and may present with acute abdominal pain
Location
Fibroids may have a number of locations within or external to the uterus:
-
intrauterine
intramural leiomyoma: most common, centred within the myometrium
subserosal leiomyoma: projecting outwards from the uterus; may be pedunculated and predominantly extrauterine, simulating an adnexal mass
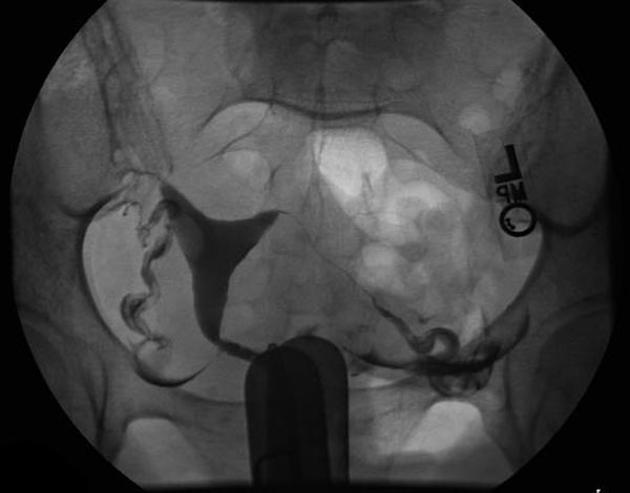
submucosal leiomyoma: least common (10-15%), projecting into the uterine cavity
-
extrauterine
Subtypes
Histological subtypes include:
Classification
Radiographic features
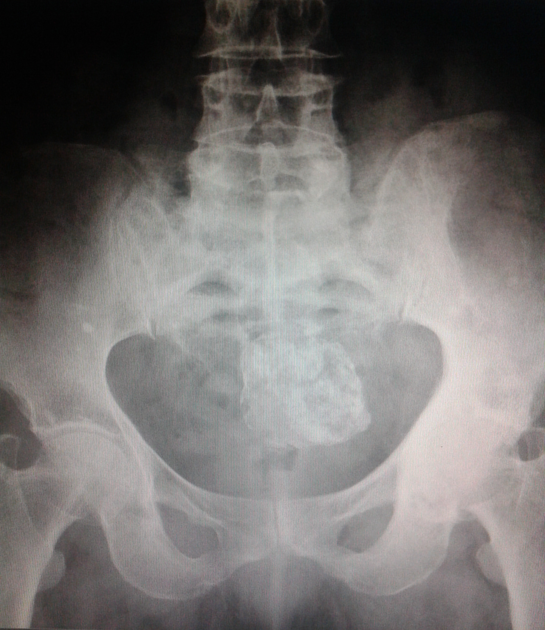
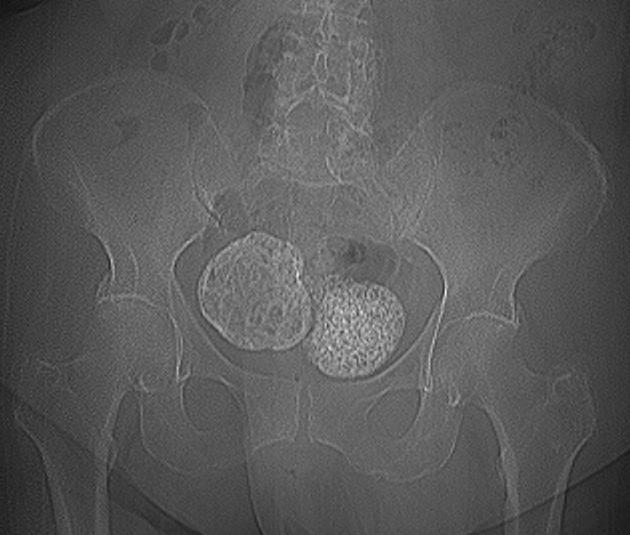
Plain radiograph
Popcorn calcification within the pelvis may suggest the diagnosis.
Ultrasound
Ultrasound is used to diagnose the presence and monitor the growth of fibroids:
uncomplicated leiomyomas are usually hypoechoic, but can be isoechoic, or even hyperechoic compared to normal myometrium
calcification is seen as echogenic foci with shadowing
cystic areas of necrosis or degeneration may be seen
Venetian blind artifact may be seen but edge shadowing +/- dense posterior shadowing from calcification is also typically seen 17
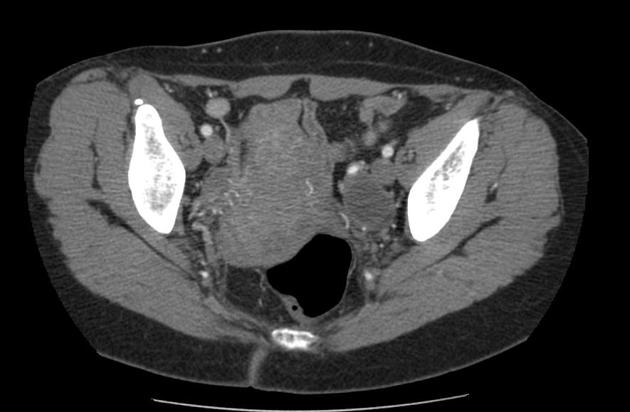
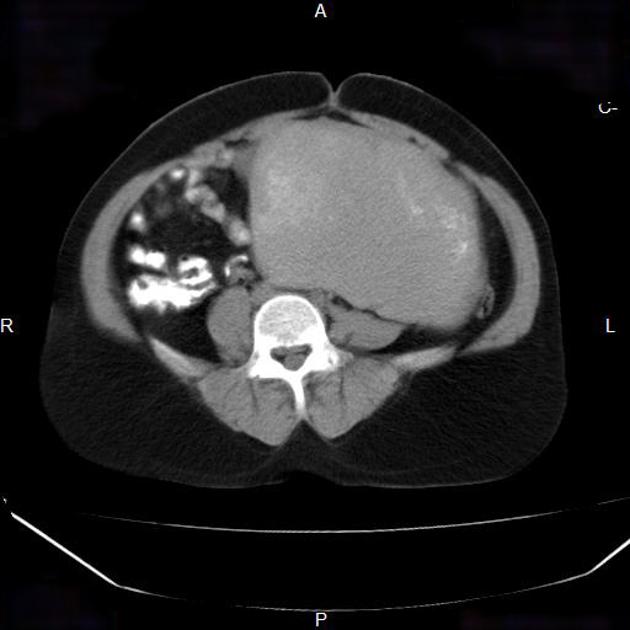
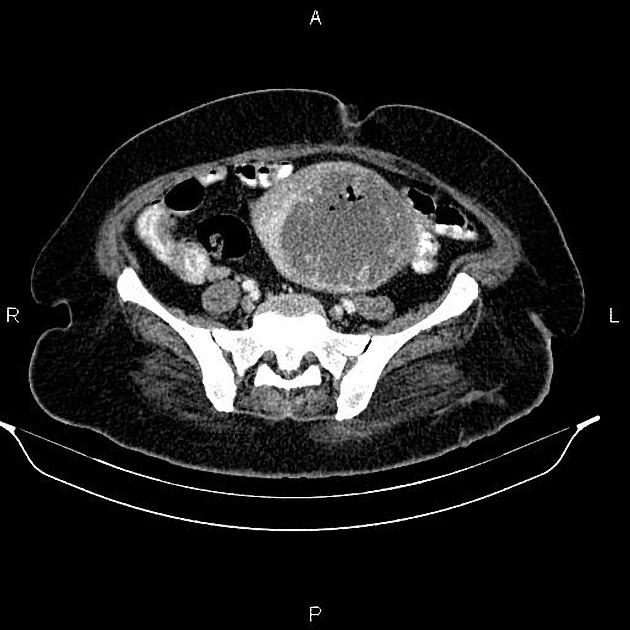
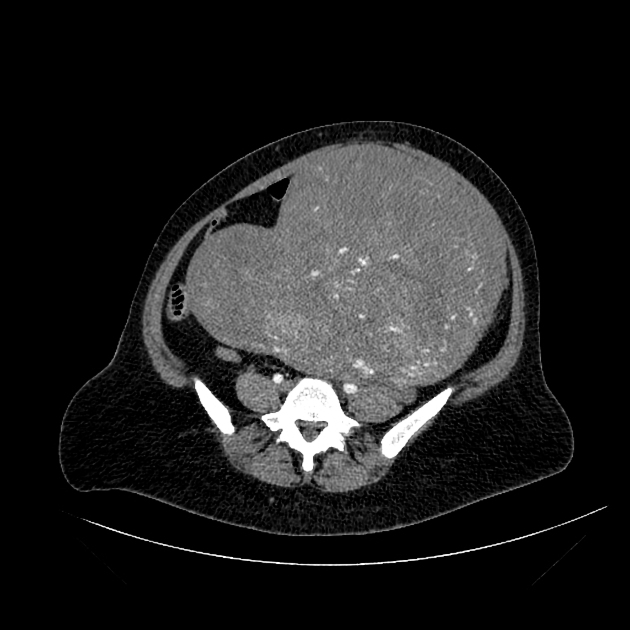
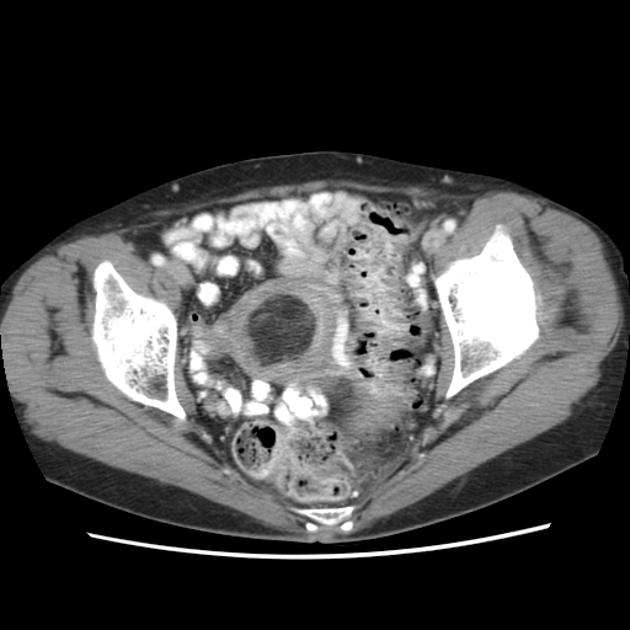
CT
fibroids are usually seen as soft tissue density lesions and may exhibit coarse peripheral or central calcification
they may distort the usually smooth uterine contour
enhancement pattern is variable
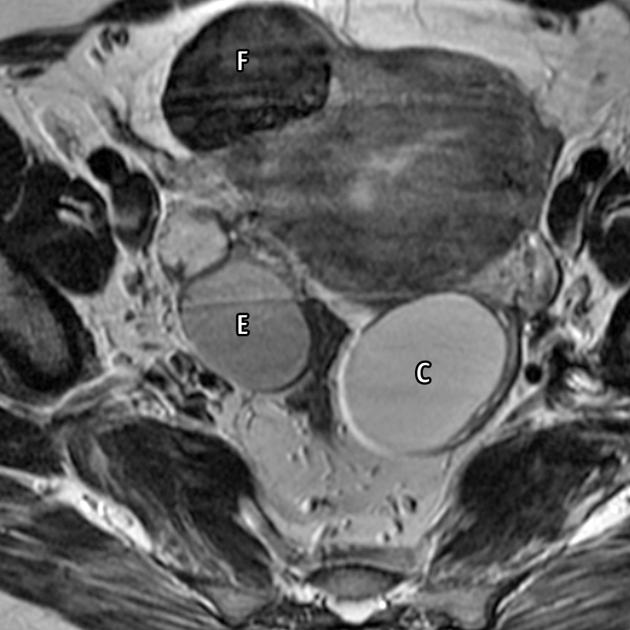
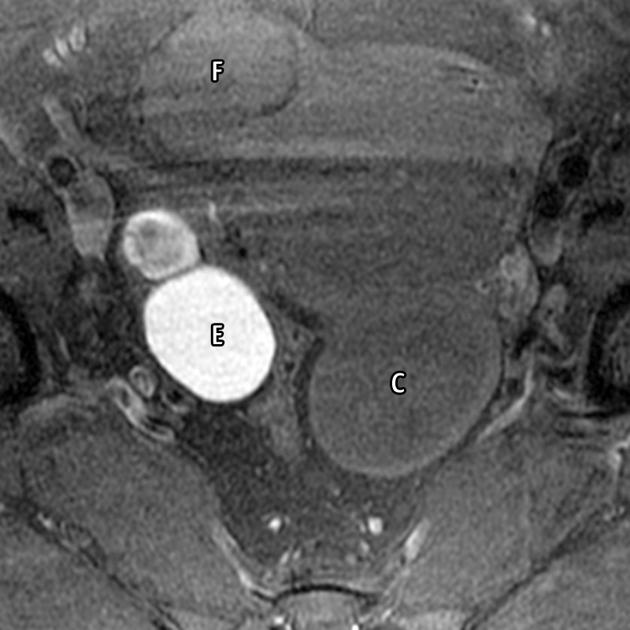
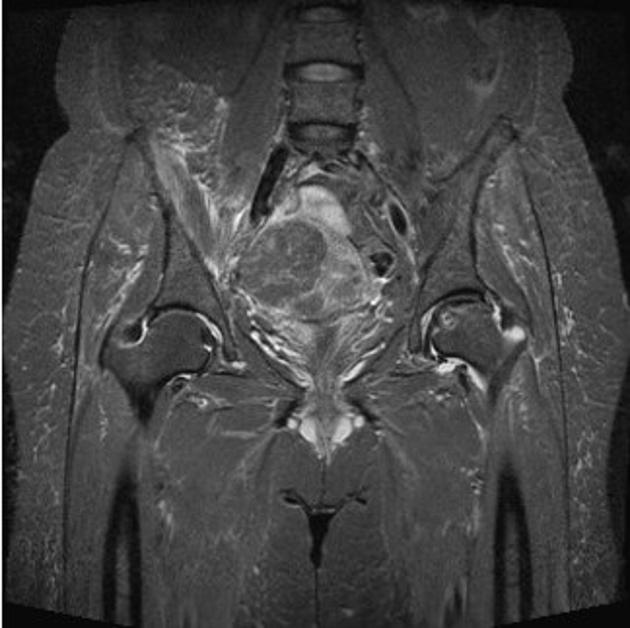
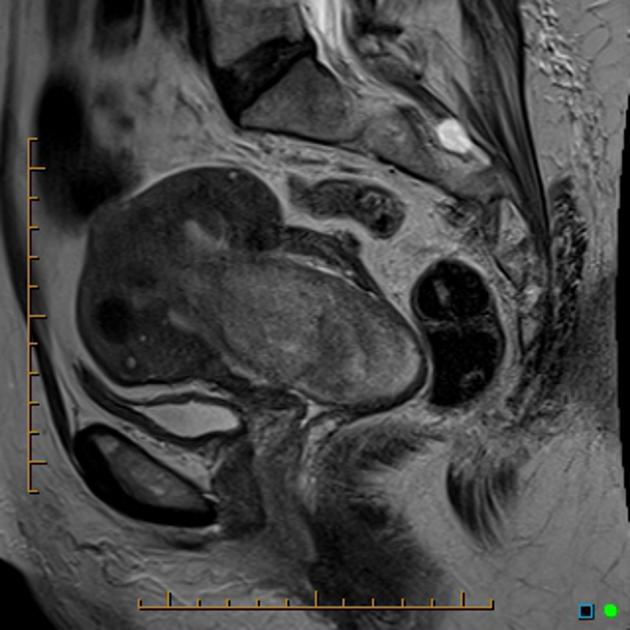
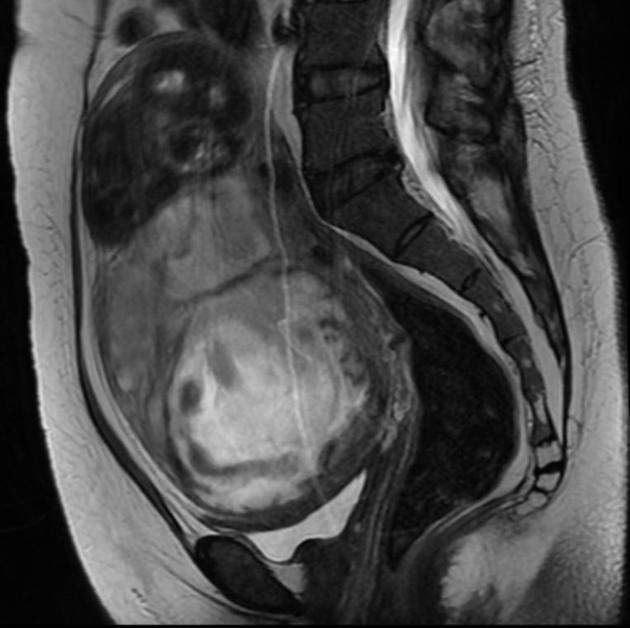
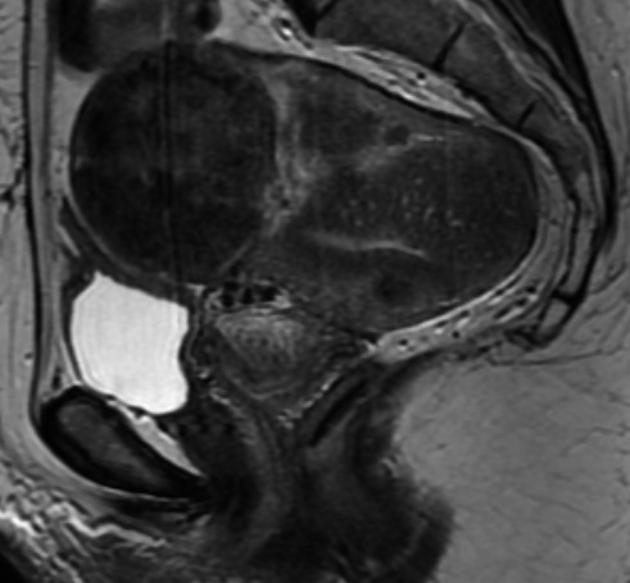
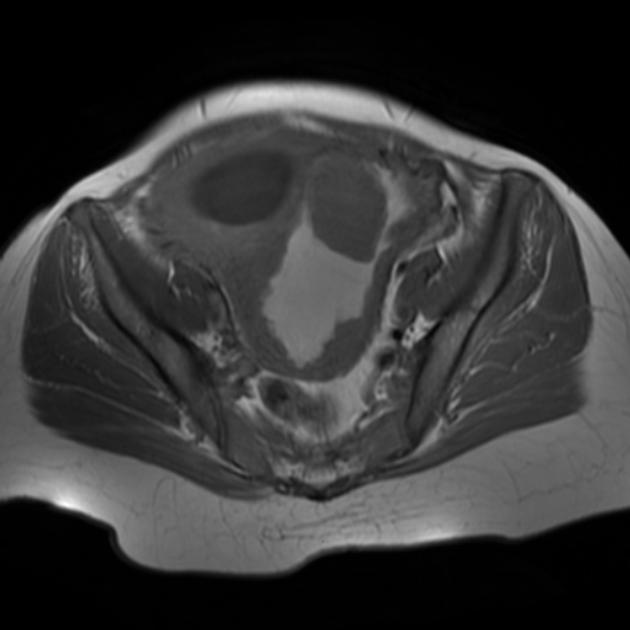
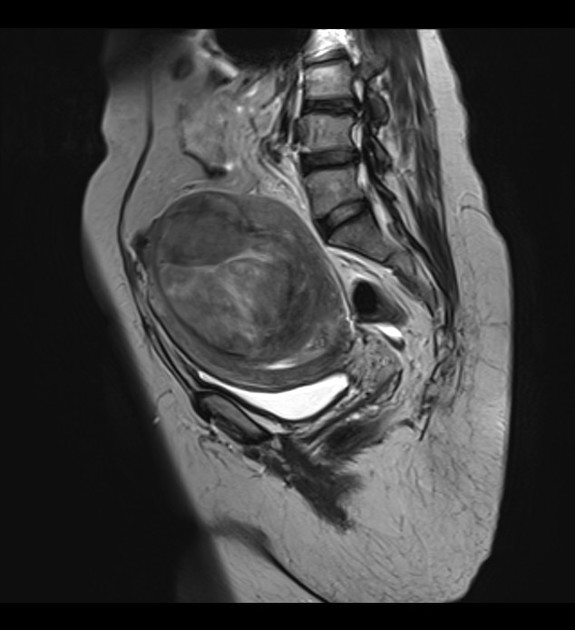
MRI
MRI is not generally required for diagnosis, except for complex or problem-solving cases. It is however more sensitive than ultrasound for detecting, localising, and characterising fibroids. Size, location, and signal intensity should be noted.
Signal characteristics are variable and include 1,2:
-
T1
non-degenerated fibroids and calcification appear as low to intermediate signal intensity compared with the normal myometrium
characteristic high T1 signal
an irregular, T1 hyperintense rim around a centrally located myoma suggests red degeneration, which is caused by venous thrombosis
-
T2
non-degenerated fibroids and calcification appear as low signal intensity
as they are usually hypervascular, flow voids are often observed around them 10
fibroids that have undergone cystic degeneration / necrosis can have a variable appearance, usually appearing as high T2 signal
hyaline degeneration is demonstrated as low T2 signal
cystic degeneration, which is an advanced stage of intratumoural oedema, also shows high T2 signal and does not enhance 10
-
T1 C+ (Gd)
variable enhancement is seen with contrast administration
the marked high signal intensity with gradual enhancement (albeit mild) suggests myxoid degeneration
MRI is of significant value in the symptomatic patient when surgery and uterine salvage therapy are considered. It is also of great value in differentiating a pedunculated fibroid from an adnexal mass 5.
Treatment and prognosis
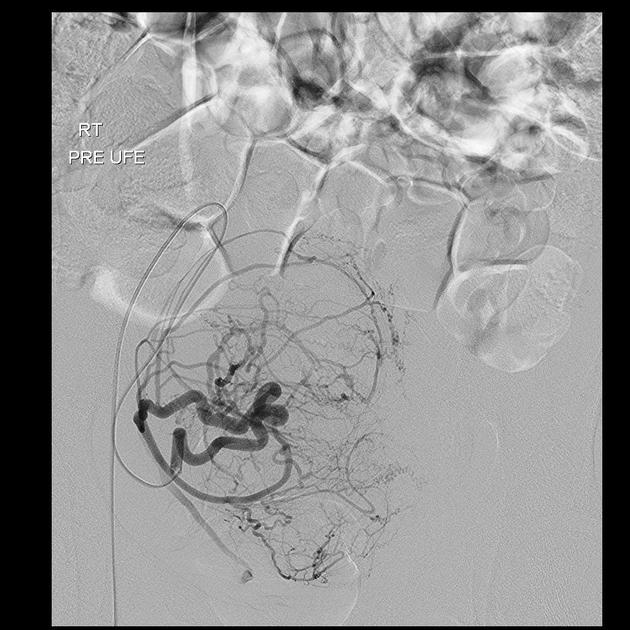
There are various medical, surgical, and interventional treatment options:
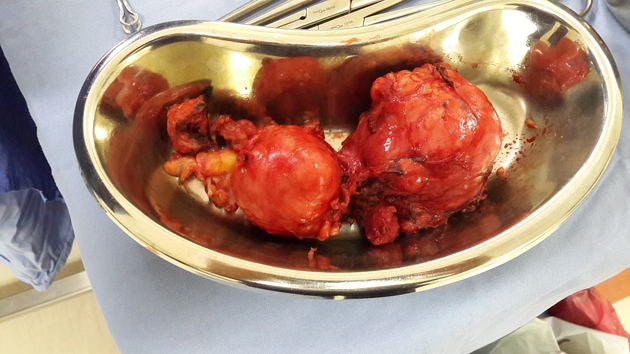
myomectomy: recurrence rate of 40-55% at 5 years 23
focal endometrial curettage
hormone administration
Complications
invasion of adjacent venous channels leading to intravenous leiomyomatosis: rare 15
malignant degeneration into leiomyosarcomas: rare (0.1-0.5%)
benign metastasising leiomyoma: extremely rare 3
pyomyoma 19
-
changes in pregnancy
around one-third of fibroids may grow in pregnancy (especially in the 1st trimester 18)
pregnancy may cause fibroid growth by 30%
-
intraperitoneal haemorrhage 24,25
a rare complication from rupture of a fibroid
usually secondary to an increase in abdominal pressure, which causes rupture of superficial veins
less often, bleeding can be arterial and associated with hypertension
trauma causing avulsion of a fibroid, torsion of a pedunculated fibroid, and pregnancy causing venous congestion
Differential diagnosis
General imaging differential considerations include:
-
malignant transformation into leiomyosarcoma is rare.
unfortunately, no imaging modality can reliably differentiate a benign leiomyoma from the rare leiomyosarcoma
uterine smooth muscle tumours of uncertain malignant potential: rare
uterine lipoleiomyoma: greater fat content (sometimes considered a variant of a leiomyoma)
focal myometrial contraction (Braxton Hicks contraction): especially if seen during pregnancy
focal adenomyosis: less well-defined; colour Doppler demonstrates tortuous vessels through the abnormality; no calcifications 4,17
In occasional situations, it may be difficult to differentiate between uterine leiomyomas and:
ovarian or adnexal masses (especially if the leiomyoma is pedunculated)

























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.