Wernicke-Korsakoff syndrome comprises two related conditions, both due to thiamine (vitamin B1) deficiency most commonly encountered in people with alcohol use disorder. Wernicke encephalopathy is the acute form, which classically presents with a triad of acute confusion, ataxia, and ophthalmoplegia. If not treated expediently, these patients can go on to develop severe psychiatric and cognitive deficits known as Korsakoff syndrome.
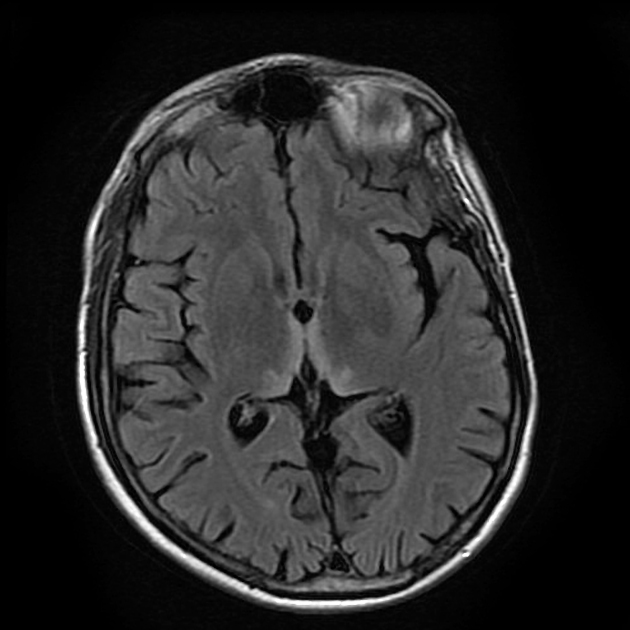
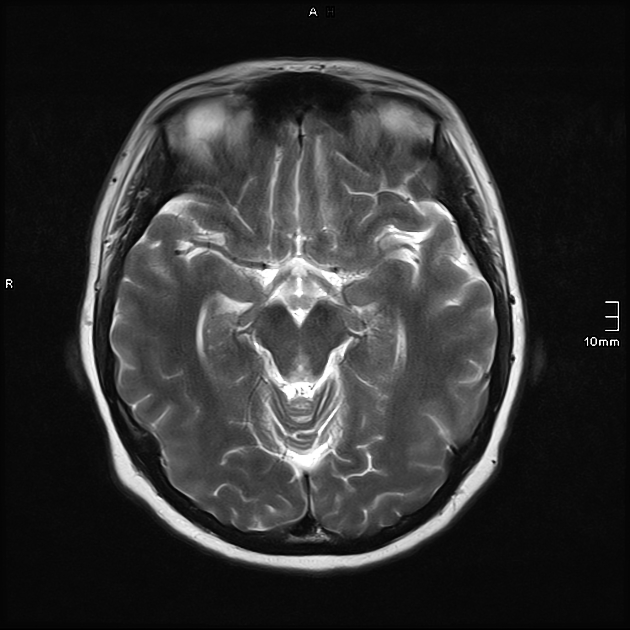
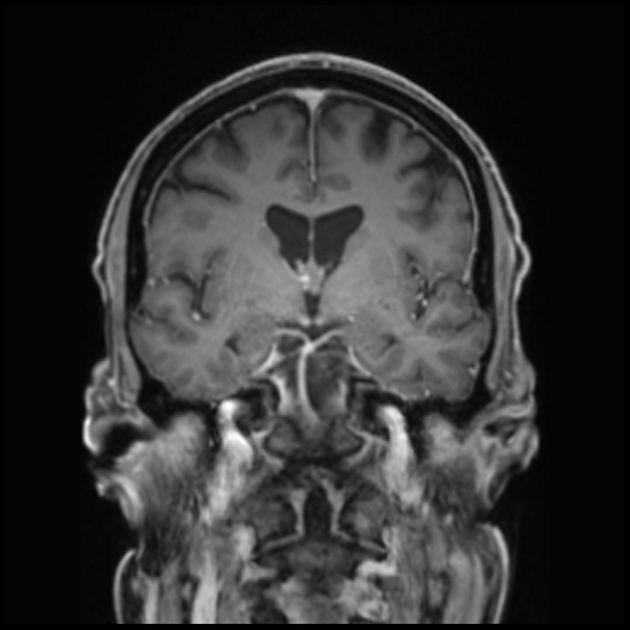
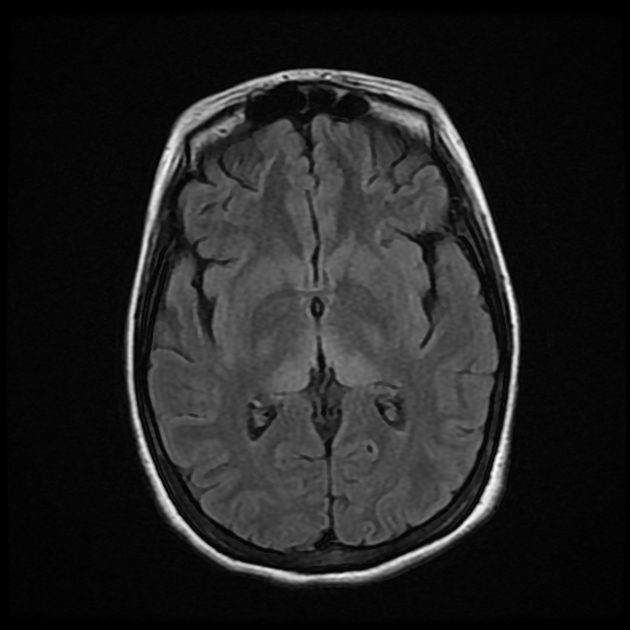
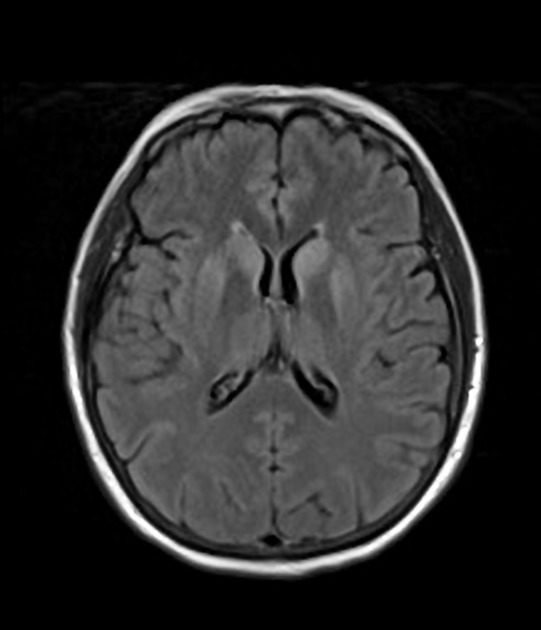
Wernecke encephalopathy may have few imaging features early in the course of presentation but eventually demonstrates areas of symmetrical increased T2/FLAIR signal involving the dorsomedial thalami, tectal plate, periaqueductal area and/or around the third ventricle. The mammillary bodies are also often affected and may enhance. In Korsakoff psychosis, mammillary body atrophy, along with thalamic and mesial temporal lobe atrophy, are the main findings 1,3,13.
On this page:
Terminology
Some advocate the use of the term alcoholic encephalopathy in an effort to avoid the eponym Wernecke encephalopathy. However, this does not take into account the many other, albeit less common, causes.
Korsakoff syndrome, or Korsakoff psychosis, is sometimes referred to as the residual syndrome but only in the context of Werneke encephalopathy 12.
Clinical presentation
Wernecke encephalopathy was originally described as characterized by the triad of:
acute confusion
ataxia
ophthalmoplegia (most commonly horizontal nystagmus and conjugate gaze palsies)
However, only a minority of patients will have all three features and some will have none 1,14.
If not promptly and thoughrouly treated, Wernicke encephalopathy can evolve into the chronic form (Korsakoff syndrome) characterized by:
memory loss (global amnesia)
confabulation
Pathology
The underlying cause is vitamin B1 (thiamine) deficiency resulting from malnutrition or malabsorption, which can occur for a number of reasons 6,7:
alcohol use disorder (up to 90% in industrialised countries 5)
starvation/fasting
prolonged total parenteral nutrition without supplementation
postbariatric surgery
hyperemesis gravidarum
gastrointestinal malignancy
chronic dialysis
Radiographic features
Werknecke encephalopathy is characterized by acute changes consisting of edema, enhancement and even hemorrhage, necrosis in a distinctive distribution (see below). In Korsakoff syndrome, these progress to atrophy most marked in the mammillary bodies.
CT
CT is generally unhelpful and is normal in the majority of patients 3,15. In the minorty of patients that have visibal abnormalities, they typically consist of hypoattenuation in the areas of oedeam (see MRI).
MRI
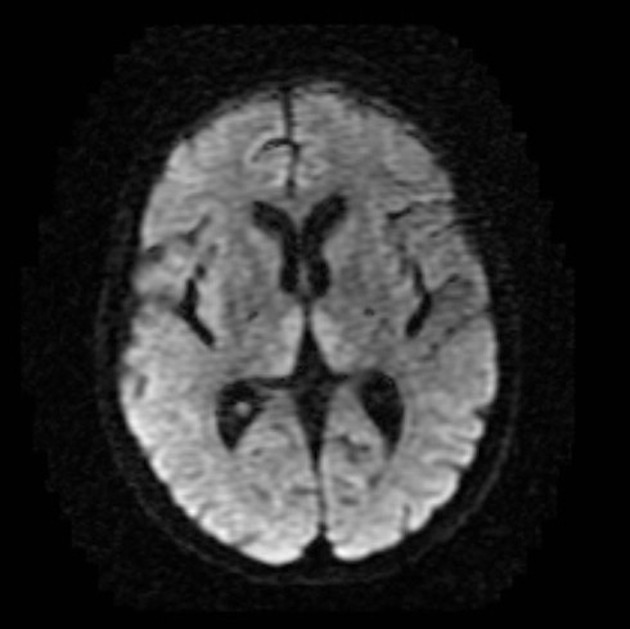
Wernecke encephalopathy
The findings in the acute phase are dominated by breakdown of the blood brain barrier with resultant odema.
-
T2/FLAIR: symmetrically increased signal intensity in the
around the third ventricle
cerebral cortex 10,11
T1 C+ (Gd): contrast enhancement can also be seen in the same regions, most commonly of the mammillary bodies 4
DWI/ADC: restricted diffusion can also be seen in the same regions 4
MR spectroscopy: may show decreased or normal NAA with the notable presence of lactate 4
SWI: petechial hemorrhage may seen as punctate regions of signal loss in the mammillary bodies 17
Korsakoff syndrome
The sequelae of Wernicke encephalopathy is gliosis and volume loss in the same regions. This often most obvious in anterior and dorsomedial thalamus and mammillary bodies 16.
Treatment and prognosis
Treatment of acute Wernicke encephalopathy is with intravenous thiamine hydrochloride, along with other vitamins/minerals, and treatment of the underlying cause (e.g. alcohol cessation). Untreated, there is high mortality of up to 20% 9.
Delayed, repeated or incompletely treated cases may progress to Korsakoff syndrome which is largely irreversible, representing damage to the aforementioned structures.
History and etymology
Carl Wernicke, a German neurologist and psychiatrist (1848-1905), first coprehensively described the acute presentation that now bares his name in 1881. He described three patients (two alcoholic men and one woman with intractable emesis) 2,13.
Sergei Korsakoff, a Russian neuropsychiatrist (1853-1900), first described the chornic form of this disease in 1887 2,13.
Differential diagnosis
General imaging differential considerations include:
Leigh disease: mammillary bodies not involved
metronidazole-induced encephalopathy: dentate nuclei, cranial nerve nuclei and splenium also involved 10
-
bilateral medial thalami abnormalities
central venous thrombosis







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.