Cerebral amyloid angiopathy (CAA) is a cerebrovascular disorder caused by the accumulation of cerebral amyloid-β (Aβ) in the tunica media and adventitia of leptomeningeal and cortical vessels of the brain. The resultant vascular fragility tends to manifest in normotensive elderly patients as lobar intracerebral haemorrhage. It is, along with Alzheimer disease, a common cerebral amyloid deposition disease.
On this page:
Epidemiology
Cerebral amyloid angiopathy can be divided into sporadic (spontaneous), familial, and iatrogenic forms.
Sporadic cerebral amyloid angiopathy
Cerebral amyloid angiopathy is a frequent incidental finding, found on screening gradient-recalled echo imaging in up to 16% of asymptomatic elderly patients 4. Autopsy studies have found a prevalence of approximately 5-9% in patients between 60 and 69 years, and 43-58% in patients over the age of 90 years 4.
Familial cerebral amyloid angiopathy
Familial cerebral amyloid angiopathy describes a group of very rare disorders that are usually encountered as autosomal dominant conditions 14,21. Many of these disorders are only isolated to only a few families and they mainly differ from spontaneous cerebral amyloid angiopathy in an earlier age of onset, typically in middle to late middle age 14,21. Furthermore, they may also be part of multisystem or other central nervous system genetic disorders 14,21.
Examples of familial cerebral amyloid angiopathy include 21:
-
Aß peptide with precursor protein APP (chromosome 21):
cerebral amyloid angiopathy related to familial Alzheimer disease
cerebral amyloid angiopathy in Down syndrome
hereditary cerebral haemorrhage with amyloidosis (Dutch, Italian, Flemish, Iowa, Piedmont, Arctic types)
ACys peptide with precursor protein cystatin C (chromosome 20): hereditary cerebral haemorrhage with amyloidosis Icelandic type
ATTR peptide with precursor protein transthyretin (chromosome 18): meningovascular amyloidosis (see cerebral transthyretin-associated amyloidoses)
AGel peptide with precursor protein gelsolin (chromosome 9): familial amyloidosis - Finnish type
PrPSc peptide with precursor prion protein (chromosome 20): Gerstmann-Straussler-Scheinker disease
ABri peptide with precursor protein ABri precursor protein (chromosome 13): familial British dementia (see case 17)
ADan peptide with precursor protein ADan precursor protein (chromosome 13): familial Danish dementia
Iatrogenic cerebral amyloid angiopathy
Iatrogenic cerebral amyloid angiopathy is an extremely rare but increasingly recognised form, considering the disease to be a prionopathy attributed to transmission of Aβ seeds through surgical procedures, such as exposure to cadaveric dura (e.g. Lyodura dural patches) or growth hormone 30. It is thought to clinically manifest approximately three decades after transmission has occurred 30.
Associations
-
pathological cerebral amyloid angiopathy changes are seen in ~80-90% of those with Alzheimer disease 5-13
~40% of those with cerebral amyloid angiopathy have Alzheimer disease
other familial syndromes (as discussed above)
Importantly, cerebral amyloid angiopathy is usually not associated with systemic amyloidoses.
Diagnosis
The Boston criteria 2.0 31, which superseded the original Boston criteria 7 and the modified Boston criteria 9, are a combination of clinical, radiographic and pathological criteria which are used to assess the probability of a diagnosis of cerebral amyloid angiopathy. These criteria require patients to have either biopsy specimens and/or brain MRI data available to make a definitive diagnosis, but probable and possible diagnoses can be made on the basis of clinicoradiological features alone 7,9. Additionally, the Edinburgh criteria for lobar intracerebral haemorrhage associated with cerebral amyloid angiopathy can be utilised, especially for patients with a lobar intracerebral haemorrhage demonstrable on CT without an MRI having been performed 26.
Clinical presentation
Manifestations of cortical vessel involvement:
lobar haemorrhages or cerebellar haemorrhages: present as stroke, often with headache, focal neurological symptoms, seizures, and decreased conscious state 19
-
cognitive impairment: occurs in three main patterns
gradual decline: a vascular dementia thought to be secondary to accumulating lobar cerebral microhaemorrhages, ischaemic leukoencephalopathy, microinfarcts, and lobar lacunes 7,15, and occurs independently to cognitive impairment of Alzheimer disease 25
step-wise decline: due to recurrent lobar haemorrhages 25
rapidly-progressive decline: may be present in inflammatory cerebral amyloid angiopathy 25, which is discussed separately
The primary manifestation of leptomeningeal vessel involvement is due to convexity subarachnoid haemorrhage, which can present with transient focal neurological episodes or symptoms (TFNE or TFNS), colloquially known as "amyloid spells" 25. These transient focal neurological episodes are classically described as recurrent, stereotyped, spreading paraesthesias lasting several minutes but there is a wide spectrum of presentations encompassing both positive (e.g. spreading paraesthesia or visual symptoms) and negative (e.g. paresis, aphasia or dysphagia) phenomenology 17,25. These symptoms are most prominent when the convexity subarachnoid haemorrhage is localised to the central sulcus 16, which is in close proximity to the primary motor and sensory cortices 25.
Other manifestations of cerebral amyloid angiopathy, which are discussed separately, include:
inflammatory cerebral amyloid angiopathy: an umbrella description for inflammatory reactions that present with rapidly-progressive cognitive decline, seizures, headache and stroke-like episodes (without lobar intracerebral haemorrhage) 1,11
cerebral amyloidoma: mass-like lesions that have a varied presentation depending on the location of the amyloidoma
Pathology
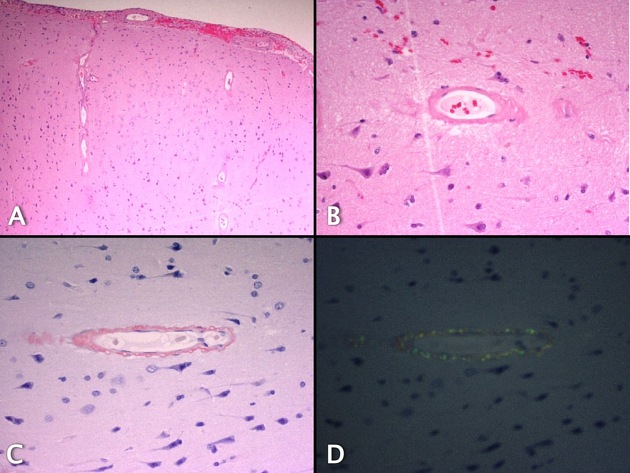
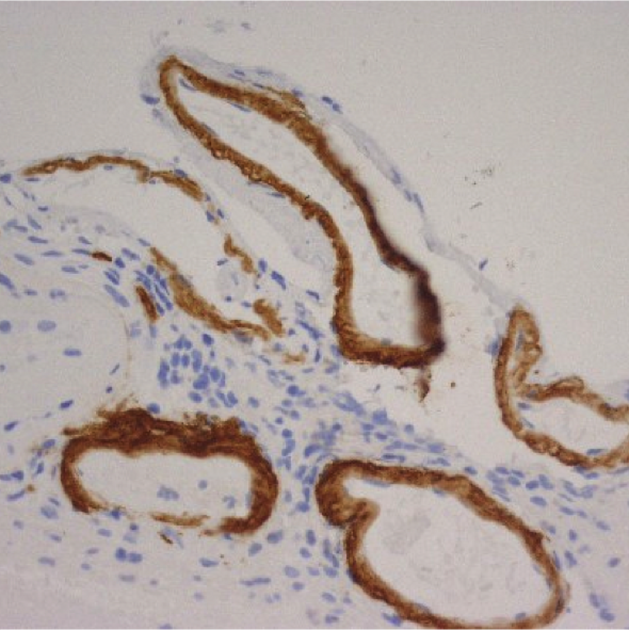
Cerebral amyloid angiopathy is characterised by the deposition of amyloid in the tunica media and/or tunica adventitia of small and medium-sized arteries of the cerebral cortex and leptomeninges 4,20. This is associated with fibrinoid degeneration with separation of the tunica media and tunica intima ('double barreling'), and microaneurysm formation 1.
There are a number of different proteins that can lead to intravascular amyloid deposition, however, the most common, as is the case in sporadic cerebral amyloid angiopathy, is Aß which is a short 42 amino acid peptide cleaved from amyloid precursor protein (APP) which is encoded on chromosome 21 20.
Aß is an eosinophilic, insoluble protein, located in the extracellular space. It stains with Congo red yielding classic apple-green birefringence when viewed with polarised light 3,20. When staining with thioflavin T and illuminated with ultraviolet light, the Aß deposits emit bright green fluorescence 20.
Radiographic features
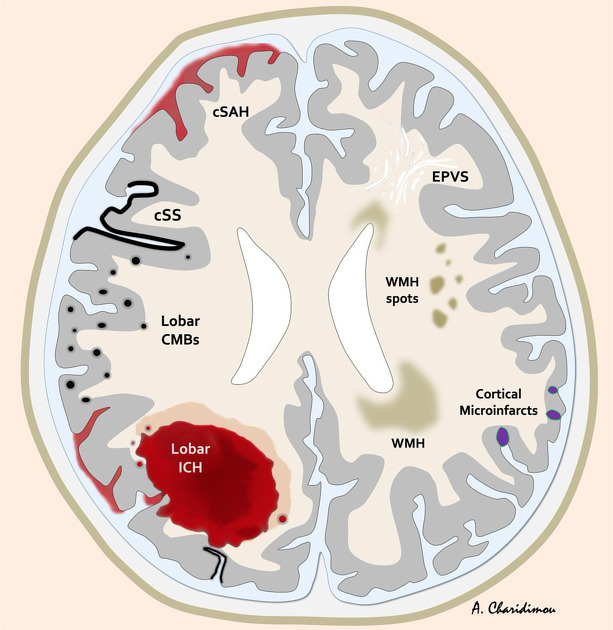
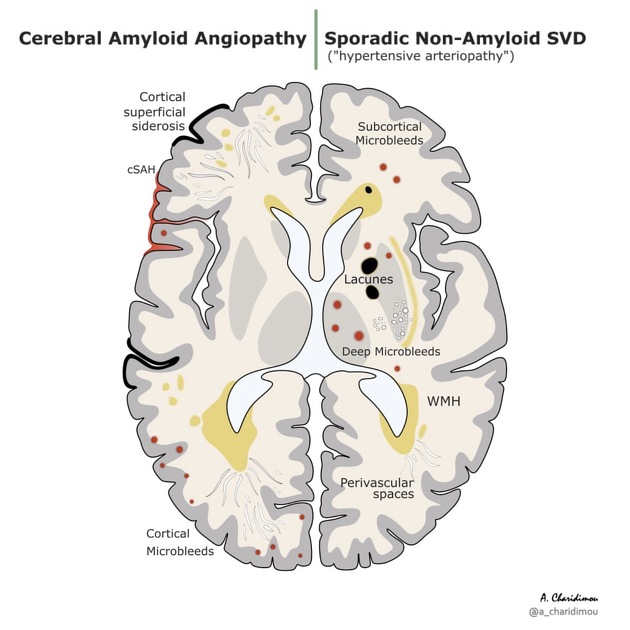
Findings reflect the various manifestations of the disease:
-
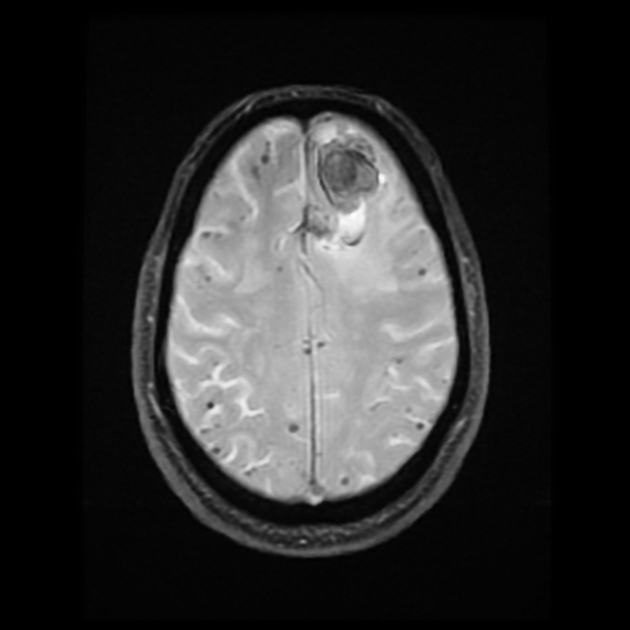
haemorrhage
-
-
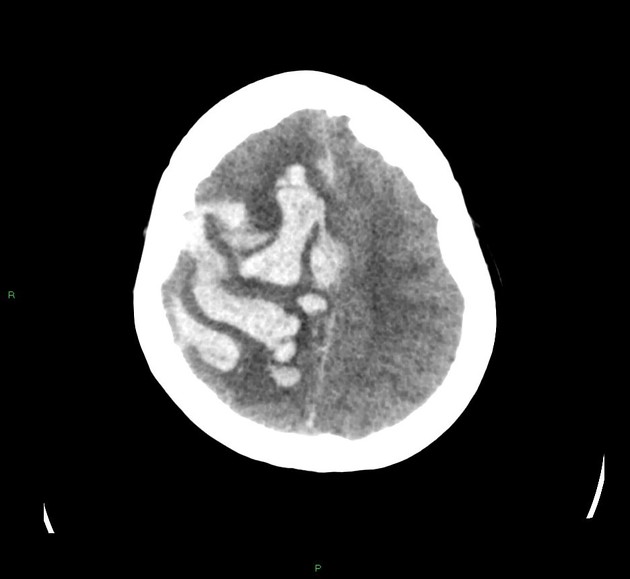
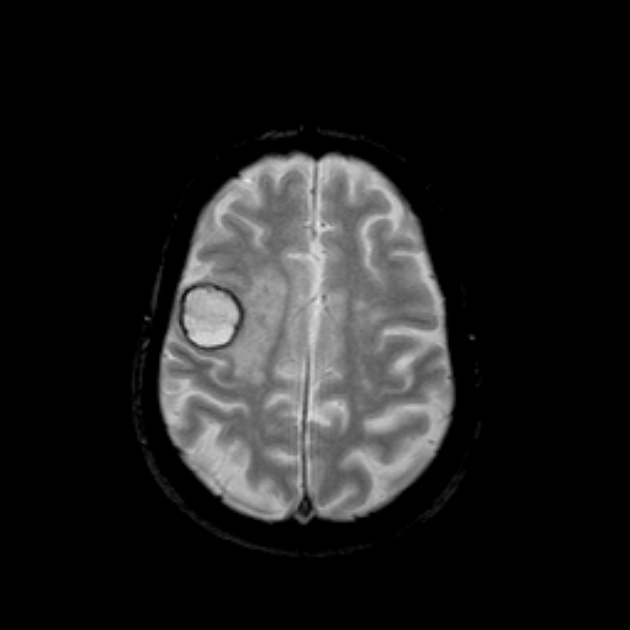
usually cortico-subcortical, in a so-called lobar location 22, but can also be seen in the 'superficial' cerebellum (especially in the cerebellar cortex or vermis) 24,34, may have finger-like projections 26
tend to spare the basal ganglia and pons (cf. hypertensive 'deep' intracerebral haemorrhage)
CT: initially hyperdense with hypodense perihaematomal oedema, often exerts positive mass-effect 25
MRI: appearance will vary according to age of bleed (see blood on MRI) 25
-
-
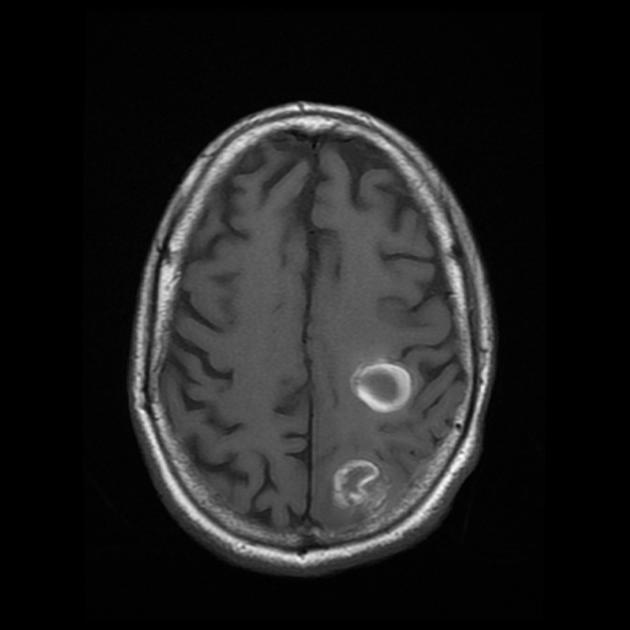
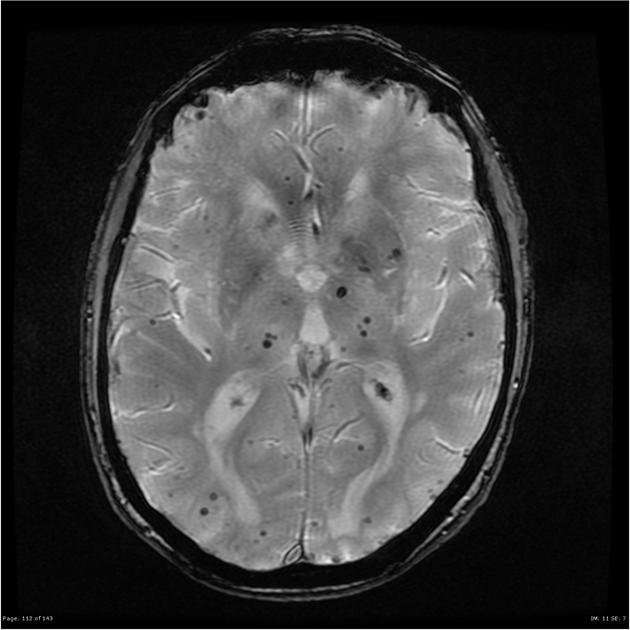
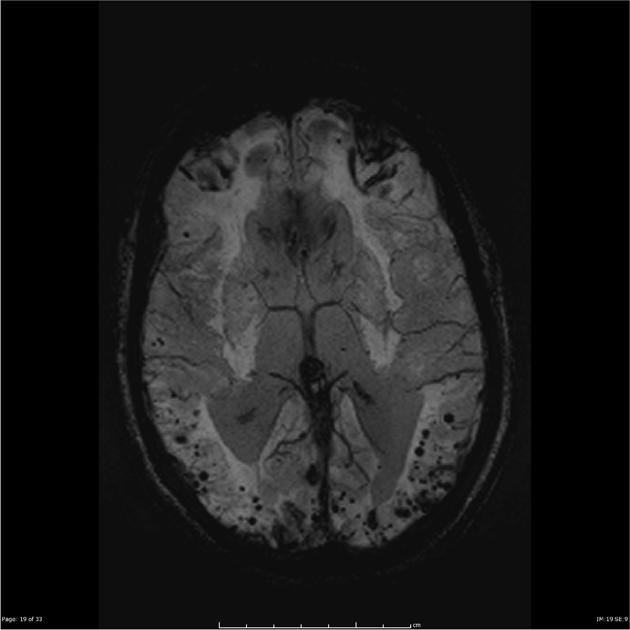
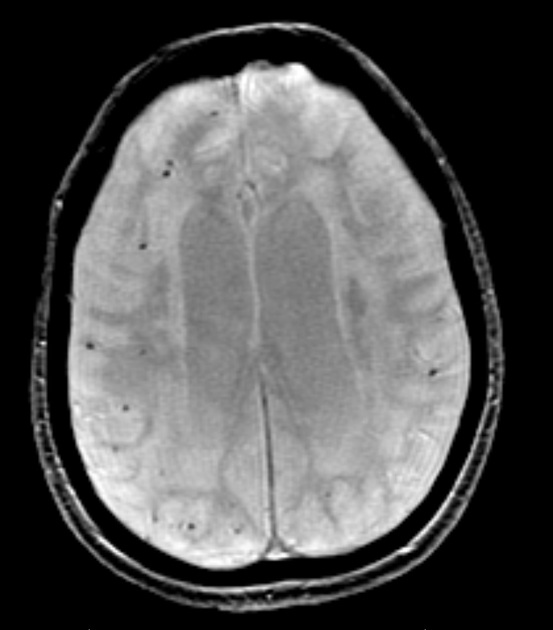
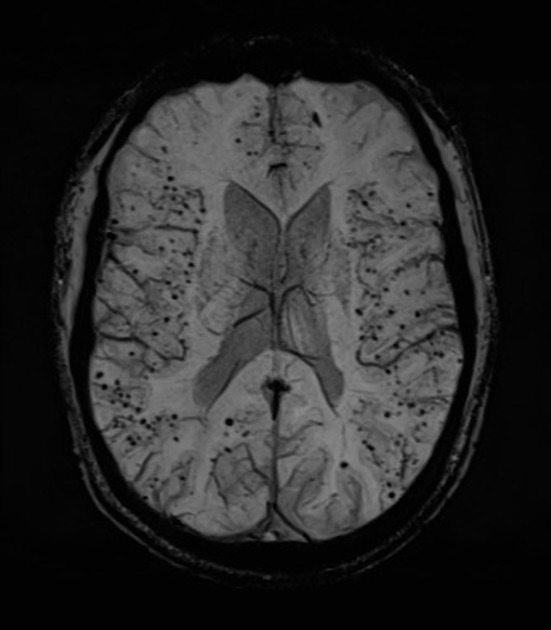
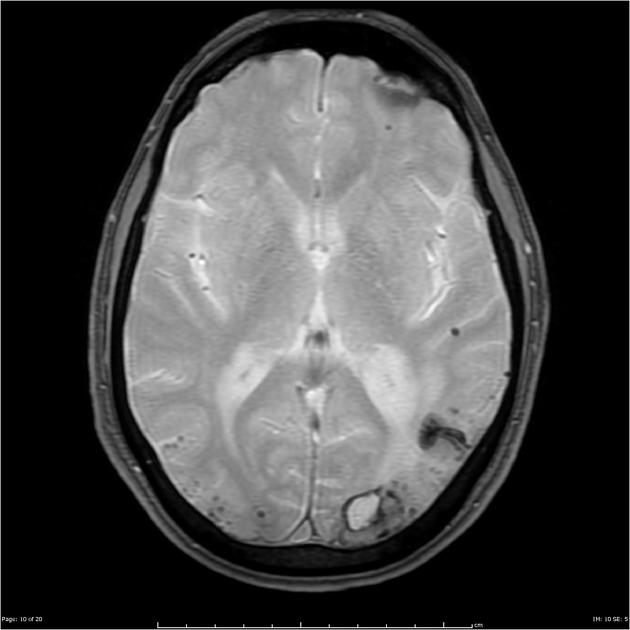
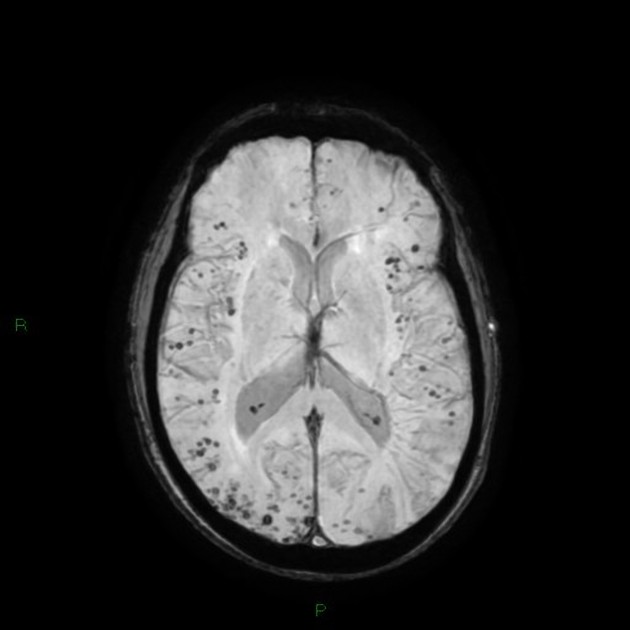
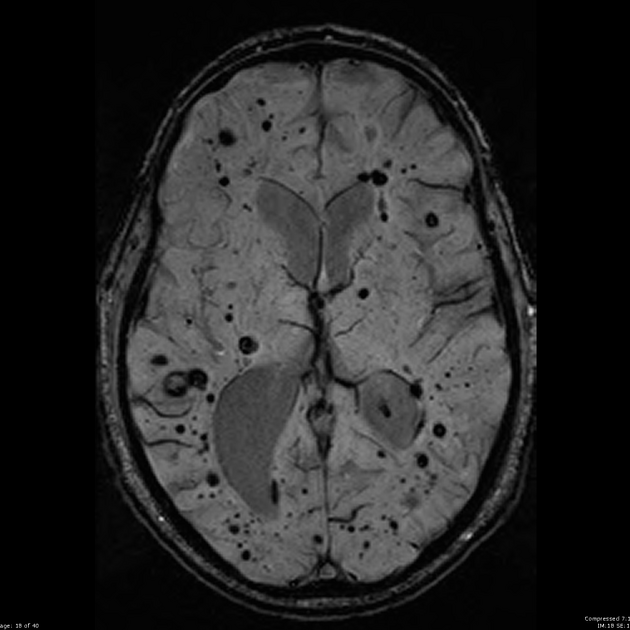
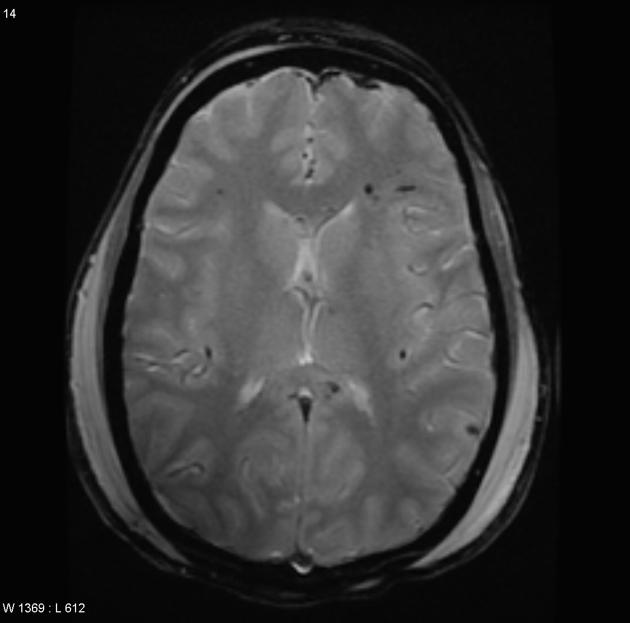
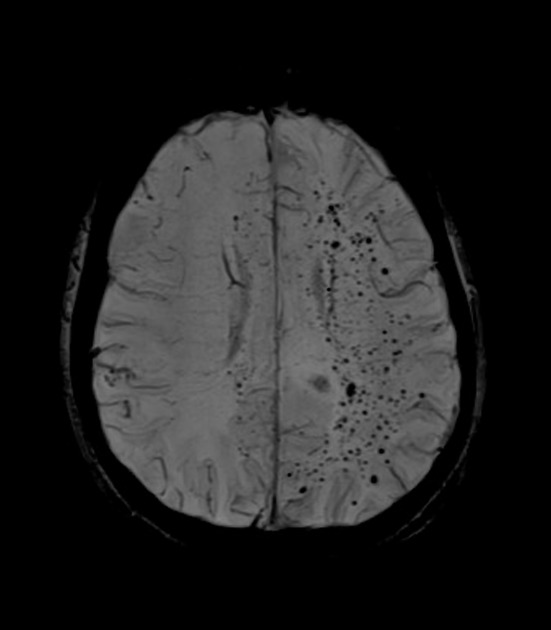
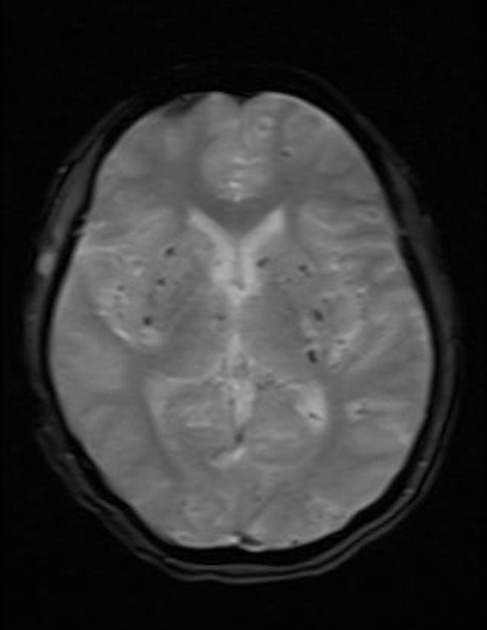
cerebral microhaemorrhage
-
defined as 2-10 millimetre, round or ovoid areas of haemorrhage, and tend to be corticosubcortical (grey-white matter junction) in distribution 25, but can also be in the superficial cerebellum 29
tend to spare the basal ganglia and pons (cf. hypertensive microhaemorrhages) 4,14
CT: not appreciated 25
MRI: only seen on T2* sequences (GRE, echo-planar, SWI) as regions of low-signal blooming artifact 12,25, not seen on conventional T1 and T2/FLAIR sequences 4
-
-
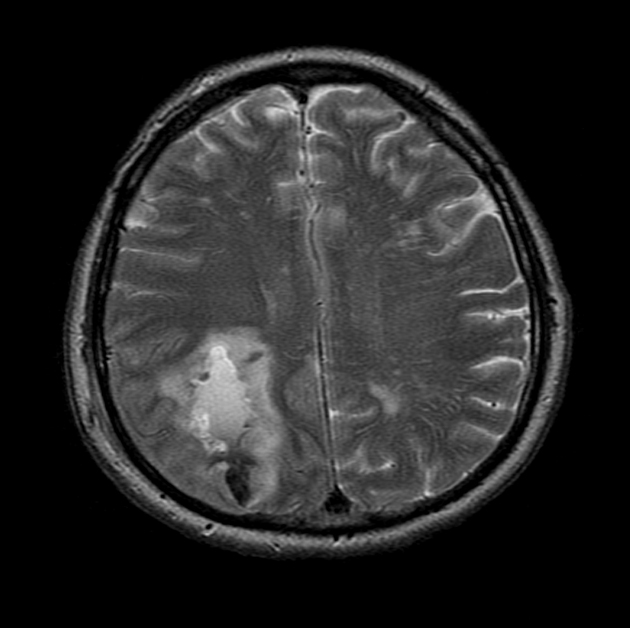
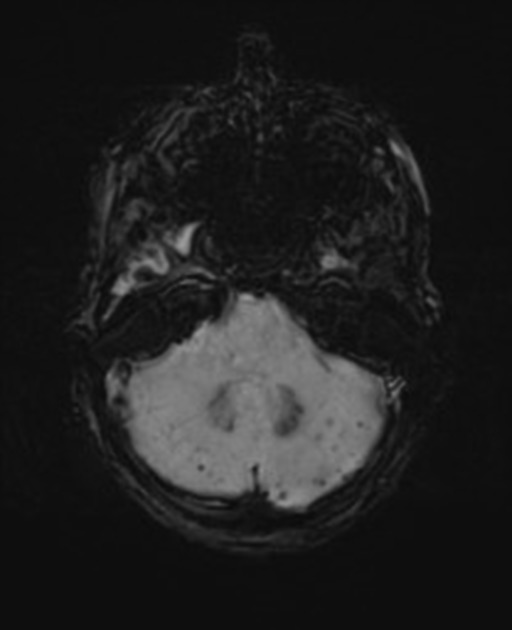
convexity subarachnoid haemorrhage
-
haemorrhage that is localised to one or more adjacent cortical sulci at the convexity of the brain
tend to spare the basal cisterns, Sylvian fissure, interhemispheric fissure and the ventricles (cf. aneurysmal subarachnoid haemorrhage or perimesencephalic subarachnoid haemorrhage) 25
CT: hyperdensity localised to one or more adjacent sulci, can be subtle 25
MRI: appearance will vary according to the age of the bleed (see blood on MRI), but is best acutely seen on T2 FLAIR as a hyperintensity 18,25
-
-
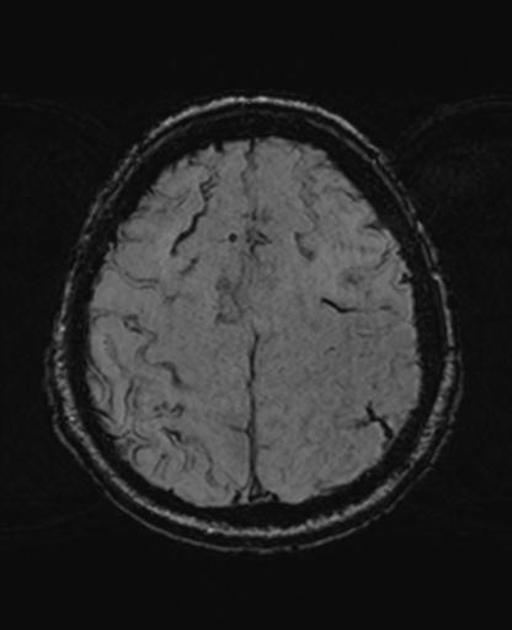
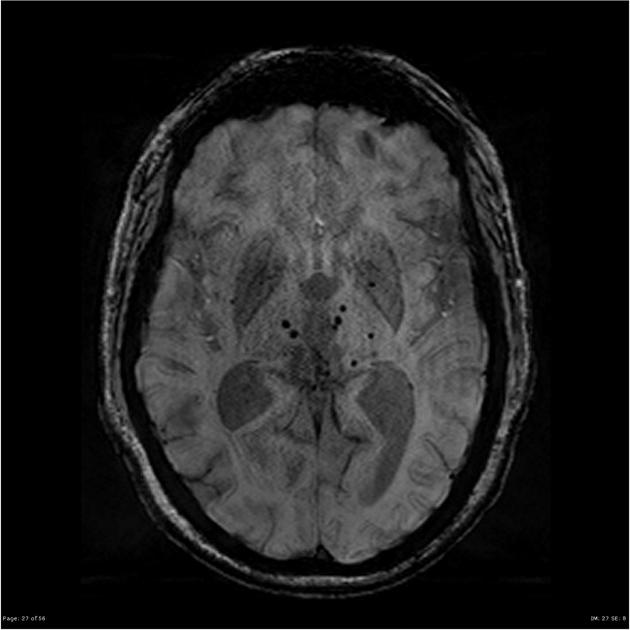
cortical superficial siderosis
-
thought to be a chronic sequela of convexity subarachnoid haemorrhage, including of haemorrhage that is asymptomatic 25
not present infratentorially (cf. superficial siderosis of the CNS) 25
CT: not appreciated 25
MRI: curvilinear regions of signal drop-out localised to one or more sulci best seen on T2* sequences (GRE, echo-planar, SWI) 9,25
-
-
cerebellar superficial siderosis 28
similar to cortical superficial siderosis but involving the folia of the cerebellum, less prevalent than cortical superficial siderosis 28
CT: not appreciated
MRI: curvilinear regions of signal drop-out localised to one or more folia best seen on T2* sequences (GRE, echo-planar, SWI) 28
-
atraumatic subdural haemorrhage 35
often seen in conjunction with intracerebral haemorrhage, but can occur independently (however, a causal link has not been definitely established) 35
CT: initially hyperdense, but appearance varies with clot age and organisation
MRI: appearance will vary according to age of bleed (see blood on MRI)
-
-
ischaemia
-
ischaemic leukoencephalopathy
chronic lesions, indistinguishable from leukoaraiosis due to other aetiologies, but tends to have a periventricular and posterior predominance 25,36
CT: diffuse hypodensity of the white matter 25
MR: T2 hyperintensity of the white matter without involvement of subcortical U-fibres (cf. cerebral amyloid angiopathy related inflammation) 7,25
-
microinfarcts and lobar lacunes
acute cortico-subcortical lesions; lobar lacunes are 3-15 millimetres in size while microinfarcts are smaller 25
CT: not appreciated 25
MRI: same signal changes as in acute ischaemic stroke, most pronounced on DWI 25
-
-
others
-
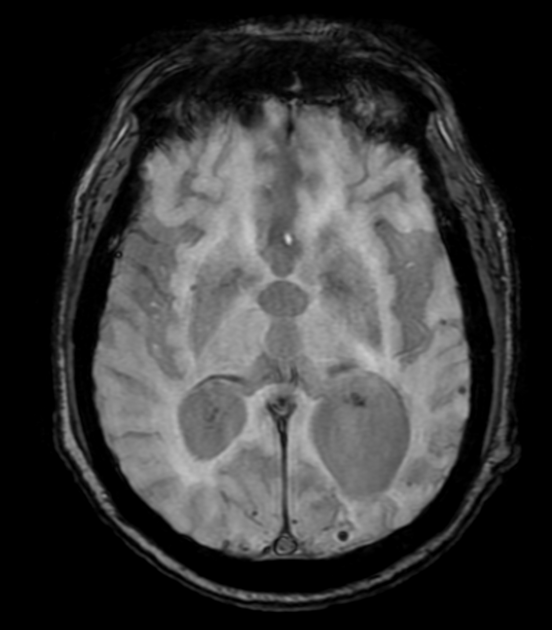
dilated perivascular spaces of the centrum semiovale
-
dilation of normal perivascular spaces in the centrum semiovale 25
tend to spare the basal ganglia and pons (cf. hypertensive dilated perivascular spaces) 25
CT: not appreciated 25
MRI: best appreciated on T2 images as CSF-signal structures with a varied appearance depending on the orientation of their draining vessel 25
-
-
cortical atrophy
CT: not appreciated 25
MRI: not readily appreciated on conventional sequences, requires cortical surface reconstructions 25
-
cortical calcifications
-
very rare in sporadic cerebral amyloid angiopathy but can be seen more commonly in certain hereditary forms (e.g. Dutch type) 32
tend to be seen in the occipital region 32
CT: readily appreciable as calcium-density areas of hyperattenuation
MRI: seen on T2* sequences (GRE, echo-planar, SWI) as regions of low-signal blooming artifact
-
-
Radiographic features of inflammatory cerebral amyloid angiopathy and cerebral amyloidoma are discussed separately.
Treatment and prognosis
There is no disease-modifying treatment available 27. Additionally, there are no guidelines regarding use of anticoagulant or thrombolytic drugs in patients with cerebral amyloid angiopathy, both medications which have been shown to possibly increase the risk of disabling haemorrhage in this patient group 27. The use of antiplatelet medications, if indicated for other reasons, may be safe 38.
Once an intracerebral haemorrhage has occurred, the highest risk of a further intracerebral haemorrhage is within the first 3 months 37. Additionally, further intracerebral haemorrhages are likely to be in close spatial proximity to the index intracerebral haemorrhage 37.
Differential diagnosis
Radiological differential diagnosis, particularly of cerebral microhaemorrhages, includes 25,33:
-
haemorrhages, including microhaemorrhages, are typically located in basal ganglia, pons and cerebellum
not associated with subarachnoid haemorrhage or superficial siderosis
-
lesions have a random distribution
random size, although Zabramski classification type IV cavernous malformations are indistinguishable from cerebral microhaemorrhages related to cerebral amyloid angiopathy
often characteristic cavernous malformations can be identified
-
haemorrhagic metastases (e.g. melanoma)
lesions have a variable size and can often be larger than microhaemorrhages
enhancing
-
lesions are typically located at the grey-white matter junction, in the corpus callosum and in more severe cases, in the brainstem
-
'starfield' pattern of distribution
lesions also show restricted diffusion on DWI and are likely visible on other sequences
-
radiation-induced vasculopathy
microhaemorrhages have a very similar appearance (similar pathophysiology)
distribution related to the treatment field
post-cardiac surgery
-
amyloid related imaging abnormalities (ARIA)
may be indistinguishable from cerebral amyloid angiopathy (especially ARIA-H), but occur in the setting of amyloid lowering therapies for Alzheimer disease







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.