Cystitis refers to inflammation of the urinary bladder. It may occur in isolation or be associated with inflammation of other parts of the urinary tract such as ureteritis or pyelonephritis.
On this page:
Epidemiology
Cystitis is more common in females due to the short length of the urethra and its close proximity to the anus, predisposing to urinary tract infection 1.
Clinical presentation
Patients typically present with local symptoms such as suprapubic pain, frequency, dysuria, hematuria, and urgency. In addition, patients may have systemic symptoms like fever, chills, rigors, and fatigue.
Serum inflammatory markers may be elevated. Urinary dipstick analysis typically shows positive leukocytes and nitrites in the setting of a urinary tract infection.
Pathology
Etiology
Cystitis has a variety of causes 1:
-
ascending urinary tract infection (most common cause):
bacterial (typically Escherichia coli, tuberculosis)
parasite (schistosomiasis)
fungal (mycosis)
-
medications:
typically from chemotherapy: e.g. cyclophosphamide
bone marrow transplant: may cause hemorrhagic cystitis 2
foreign body: including indwelling catheters
fistula: from adjacent colon, rectum, or vagina (typically seen as a complication of diverticulitis, Crohn disease, or malignancy)
idiopathic: e.g. interstitial cystitis, eosinophilic cystitis
Subtypes
Radiographic features
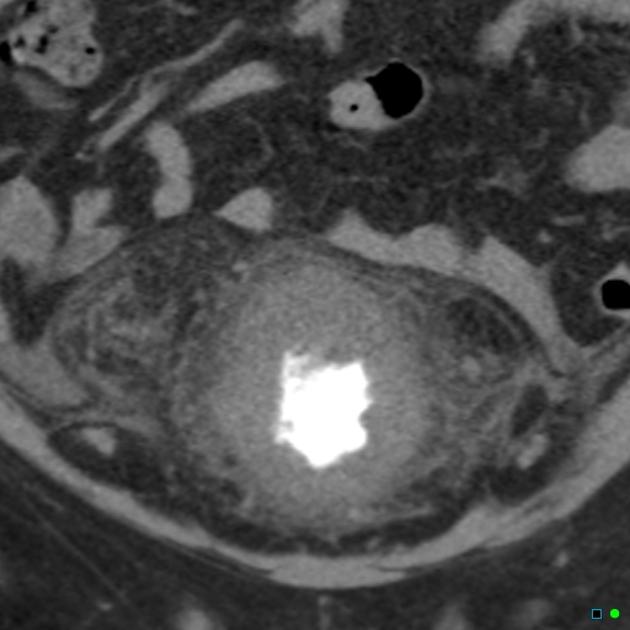
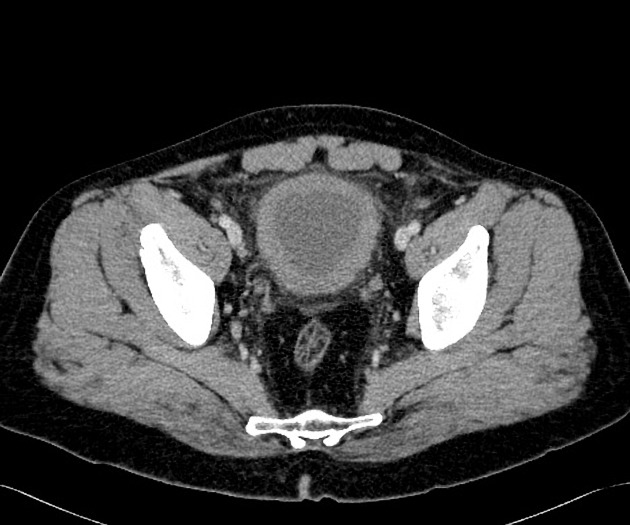
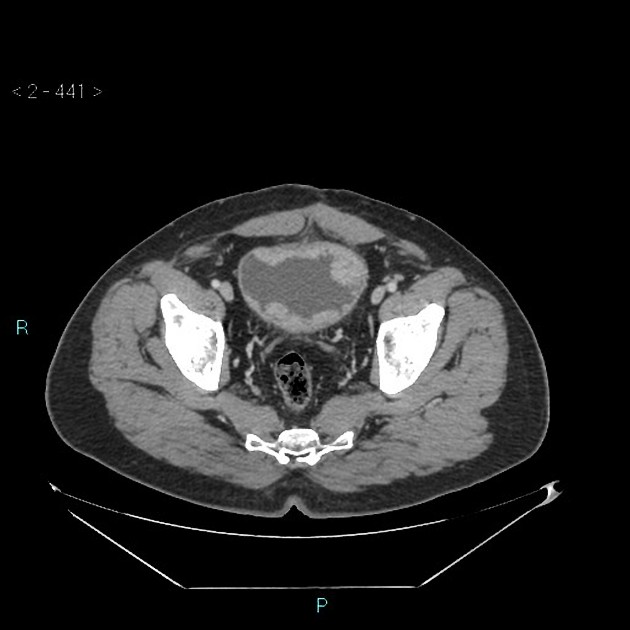
Typical imaging features include 1:
bladder mural hypertrophy: may be diffuse, or less commonly focal; defined as >3 mm when distended or >5 mm when non-distended
urothelial mucosal irregularity
layering intraluminal debris
periserosal edema: fat stranding and free fluid
mural calcification may be present: typically in schistosomiasis
A bladder neoplasm, foreign body, or diverticulum may be seen in chronic cystitis.
In cystitis secondary to tuberculosis, chronic fibrosis may result in a contracted “thimble bladder”.
CT or MRI is useful to assess for the presence of a fistula, particularly in the setting of recurrent cystitis.
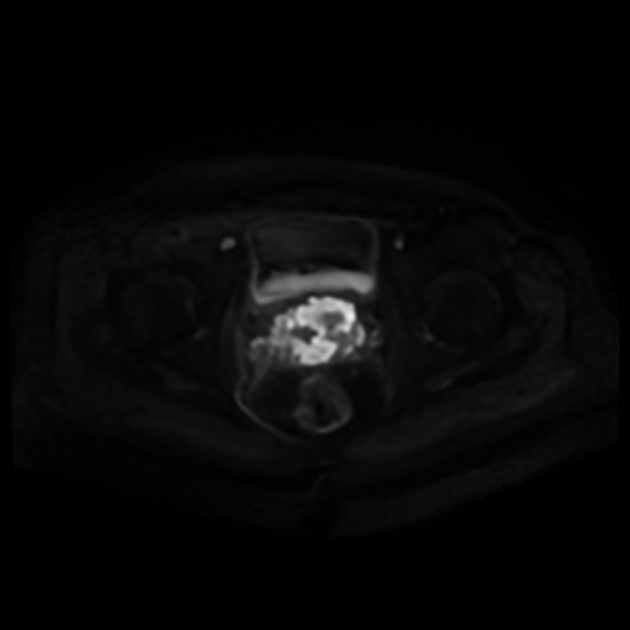
MRI
T2: hyperintense bladder mucosa 3
T1 C+ (Gd): shows increased enhancement of the affected bladder wall (but less enhancement than a bladder neoplasm), also useful in characterizing a bladder abscess
Treatment and prognosis
Antibiotics are the first-line treatment 4.
Complications
bladder abscess (may be intramural or exophytic) 1
emphysematous cystitis: gas within the bladder wall, typically seen in diabetic patients 1
Chronic cystitis may result in 5:
bladder carcinoma: typically squamous cell carcinoma
Differential diagnosis
transitional cell carcinoma of the bladder: typically demonstrates a focal mass/thickening







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.