Gynaecomastia refers to a benign excess of the male breast tissue, that is usually reversible. It is not a risk factor per se for developing male breast cancer.
On this page:
Epidemiology
While it can occur at any age, it tends to have greater prevalence in two groups: adolescent boys and older men (some publications describe a trimodal age distribution, occurring in neonatal, pubertal, and elderly males 8). Prevalence of "asymptomatic" gynaecomastia ranges around 8:
neonates: 60-90%
adolescents: 50-60%
men aged 50 to 69 years: up to 70%
Prevalence of "symptomatic" cases is markedly lower.
Clinical presentation
Palpation usually demonstrates a palpable, tender, firm, mobile, disc-like mound of tissue 8.
Pathology
In gynaecomastia, there is enlargement of the male breast due to benign ductal and stromal proliferation. A hallmark of gynaecomastia is its central location under the nipple. Gynaecomastia in most cases tends to be unilateral and/or asymmetrical 3.
The imbalance between oestrogen action relative to androgen action at the breast tissue level appears to be a key aetiological factor in gynaecomastia 8.
Aetiology
The causes of gynaecomastia are many and include:
-
hormonal
neonatal: maternal oestrogens
pubertal: high oestradiol levels
elderly: decline in testosterone levels
-
hypogonadism/androgen deficiency states:
testicular failure, e.g. testicular cancer
-
drugs
diethylstilboestrol
spironolactone
thiazide diuretics
digoxin
anabolic steroids
oestrogen treatment
flutamide
finasteride
isoniazid
ergotamine
-
narcotics:
marijuana
heroin
cimetidine
nifedipine
reserpine
efavirenz
methyldopa
theophylline
valproic acid
-
systemic disorders
advanced alcoholic cirrhosis
chronic pulmonary disease, e.g. emphysema, tuberculosis
haemodialysis in chronic renal failure
malnutrition
-
tumours: particularly oestrogenic tumours
testicular cancer: including sex-cord stromal, and germ cell tumours 9
idiopathic
Microscopic appearance
There can be three histological forms:
florid
intermediate
fibrotic
Radiographic features
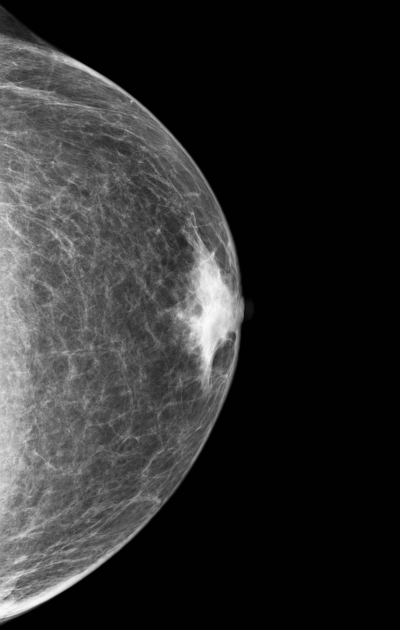
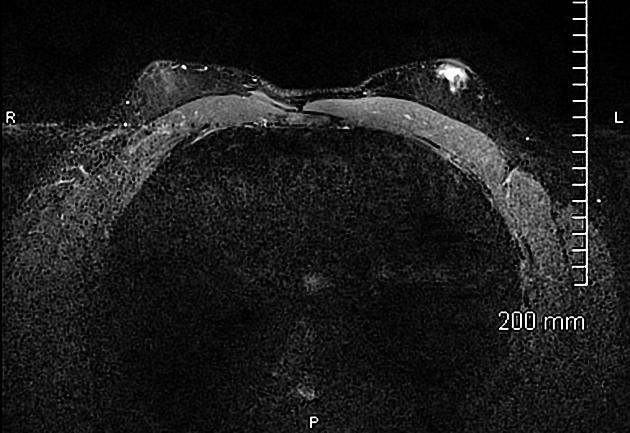
Mammography
May appear as an increased sub-areolar density, which may be flame-shaped.
Three mammographic patterns of gynaecomastia have been described representing various degrees and stages of ductal and stromal proliferation. They are 14:
nodular pattern
dendritic pattern
diffuse glandular pattern
Early nodular gynaecomastia (florid phase) is seen in patients with gynaecomastia for less than 1 year. At mammography, there is often a nodular subareolar density.
Chronic dendritic gynaecomastia (quiescent phase) is seen in patients with gynaecomastia for longer than 1 year. Fibrosis becomes the dominant process and is irreversible. Mammograms this phase typically show a dendritic subareolar density with posterior linear projections radiating into the surrounding tissue toward the upper-outer quadrant.
Diffuse glandular gynaecomastia is commonly seen in patients receiving exogenous oestrogen. At mammography, there is enlargement of the breast and diffuse density with both dendritic and nodular features.
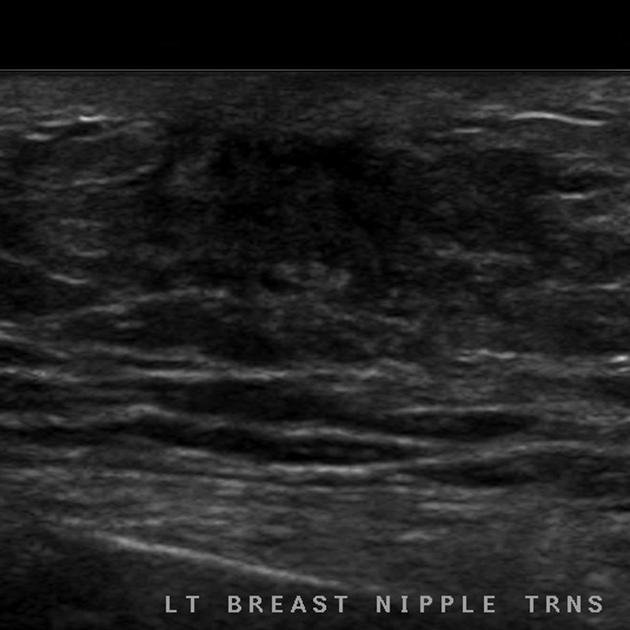
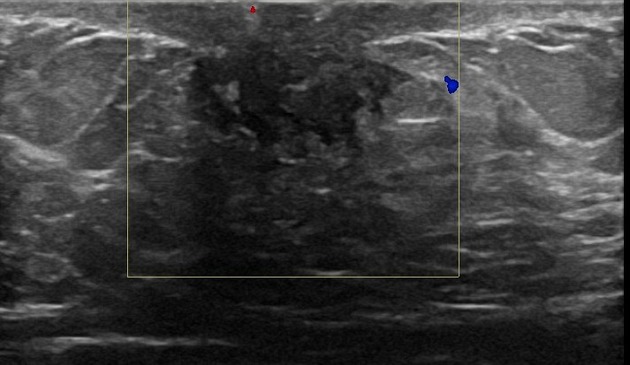
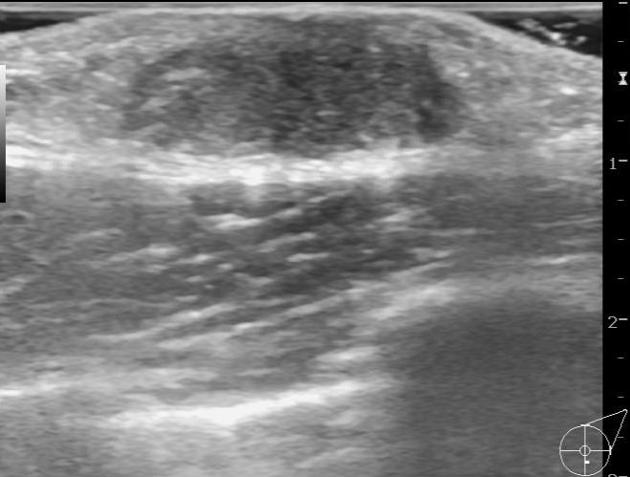
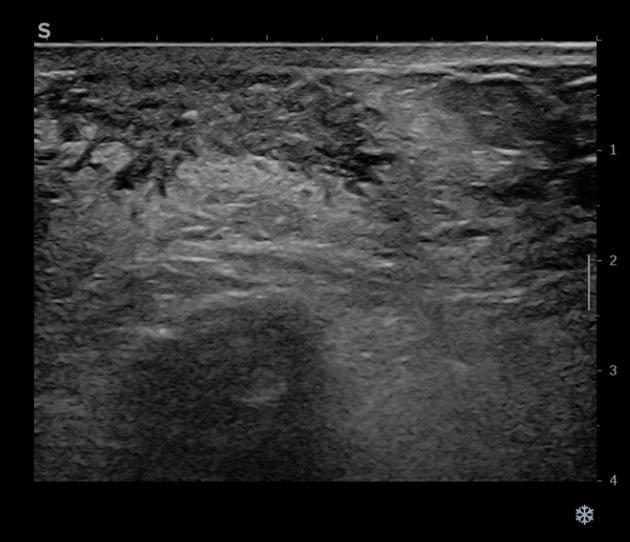
Ultrasound
Focal gynaecomastia can variably appear as a retroareolar, triangular, hypoechoic (~80% 2) mass.
In early nodular gynaecomastia, there can be subareolar fan or disc-shaped hypoechoic nodule surrounded by normal fatty tissue.
In diffuse glandular gynaecomastia, both nodular and dendritic features are seen surrounded by diffuse hyperechoic fibrous breast tissue.
In chronic dendritic gynaecomastia, there is often a subareolar hypoechoic lesion with an anechoic star-shaped posterior border, which can be described as fingerlike projections or "spider legs" insinuating into the surrounding echogenic fibrous breast tissue.
Differential diagnosis
pseudogynaecomastia: involves breast enlargement (usually bilateral) caused by an excess of adipose tissue, which is not necessarily associated with constitutional obesity
-
unilateral fixed painless irregular hard mass
may occur remotely from the areola (gynaecomastia does not)
skin thickening and tethering



























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.