Hiatus hernias (alternative plural: herniae) occur when there is herniation of abdominal contents through the esophageal hiatus of the diaphragm into the thoracic cavity.
On this page:
Epidemiology
The prevalence of hiatus hernia increases with age, with a slight female predilection.
Clinical presentation
Many patients with hiatus hernia are asymptomatic, and it is an incidental finding. However, symptoms may include epigastric or chest pain, postprandial fullness, nausea and vomiting 3.
Sometimes hiatus hernias are considered synonymous with gastro-esophageal reflux disease (GERD), but there is a poor correlation between the two conditions.
Pathology
The most common content of a hiatus hernia is the stomach. There are two main types of hiatus hernia (although they may co-exist):
sliding hiatus hernia (>90%)
Some divide them into four types:
type 1: sliding hiatal hernia (~95%)
type 2: paraesophageal hiatal hernia with the gastro-esophageal junction in a normal position
type 3: mixed or compound type, paraesophageal hiatal hernia with displaced gastro-esophageal junction
type 4: mixed or compound type hiatal hernia with additional herniation of viscera
Subtypes
Sliding hiatus hernia
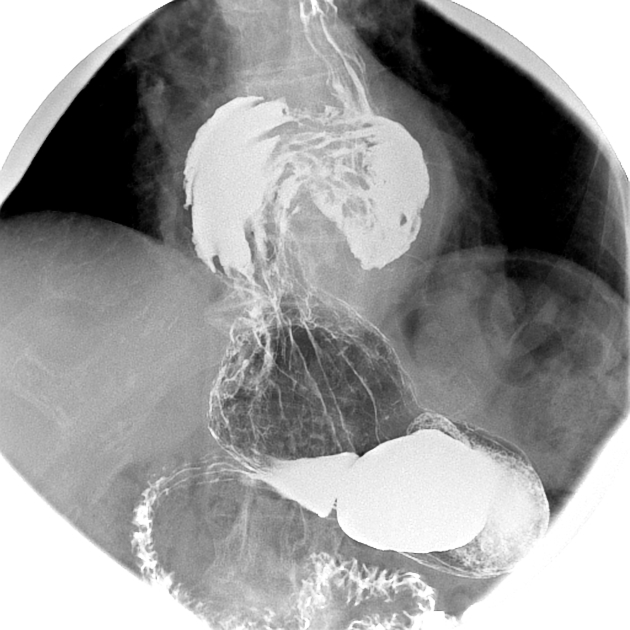
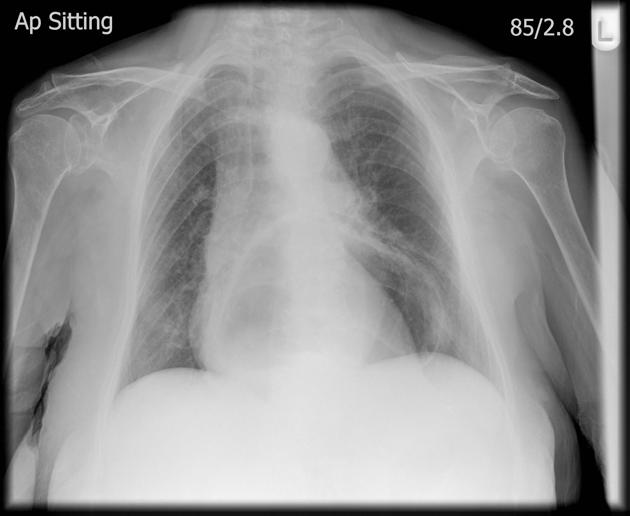
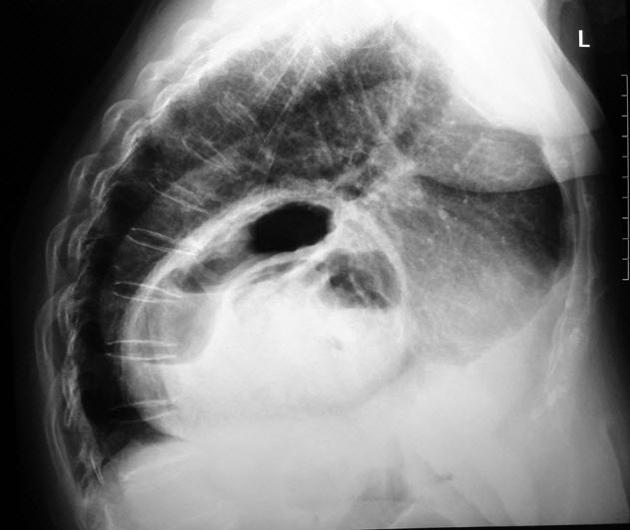
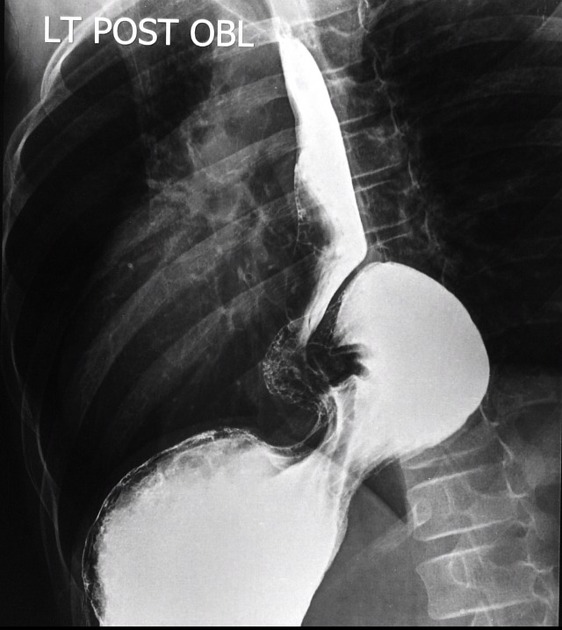
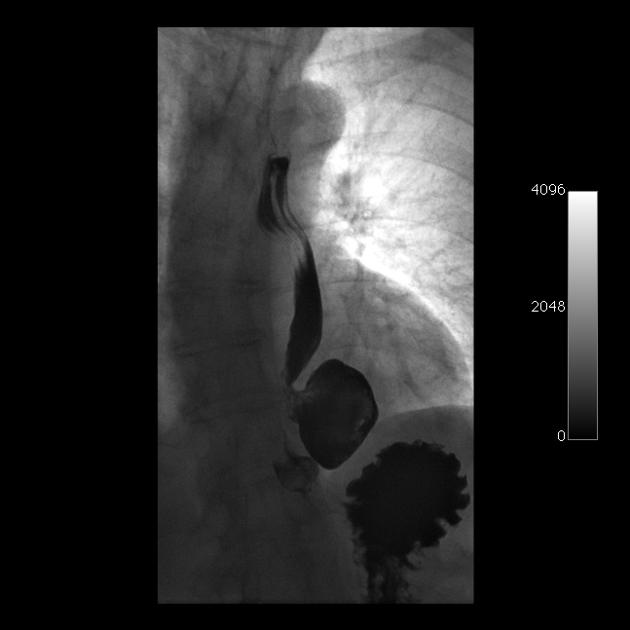
This is the most common type of hiatus hernia (~90%). The gastro-esophageal junction (GEJ) is usually displaced >2 cm above the esophageal hiatus. The esophageal hiatus is often abnormally widened to 3-4 cm (the upper limit of normal is 1.5 cm). Under fluoroscopy, if >3 gastric folds are seen above the hiatus, this is suggestive of a sliding hiatus hernia.
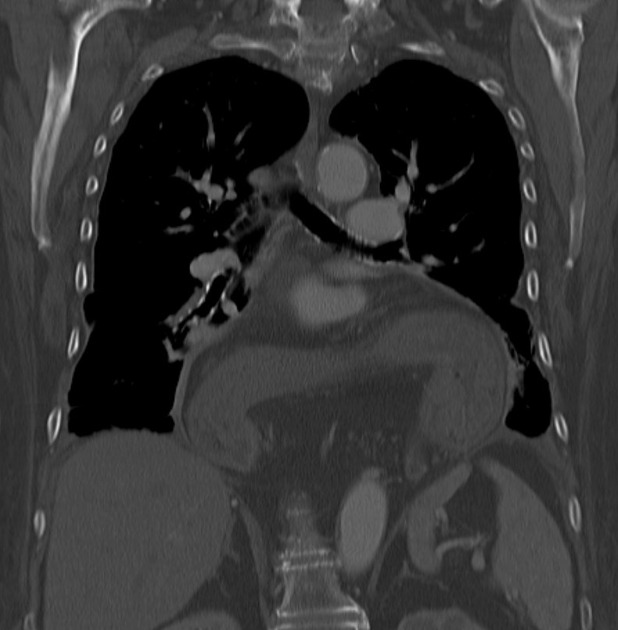
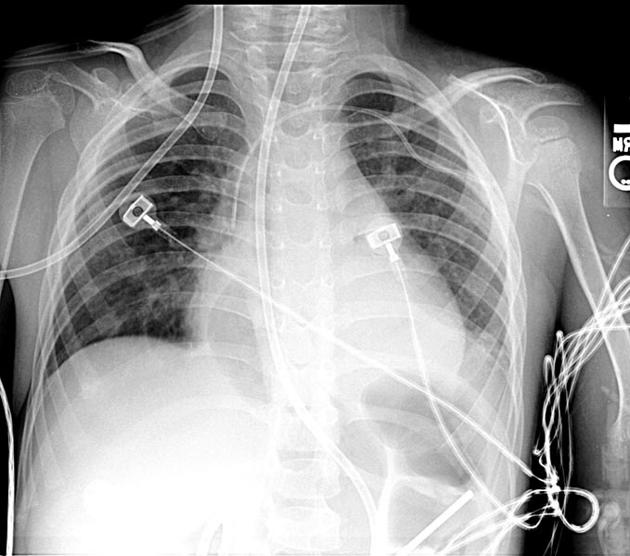
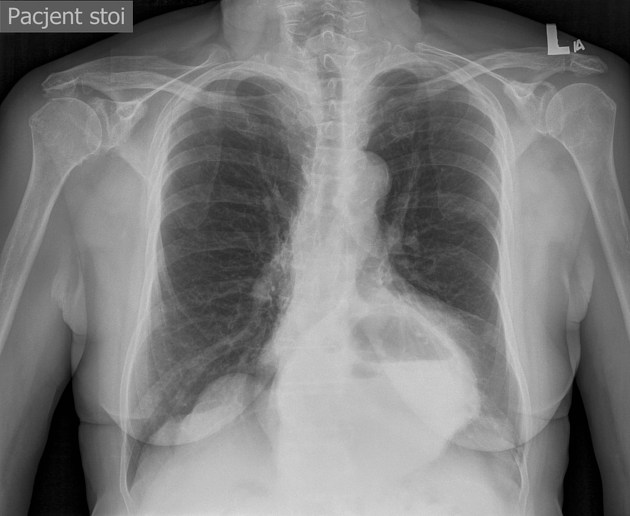
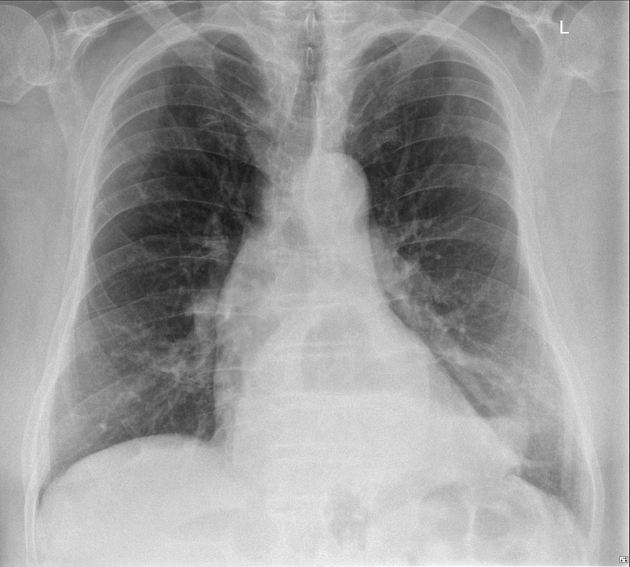
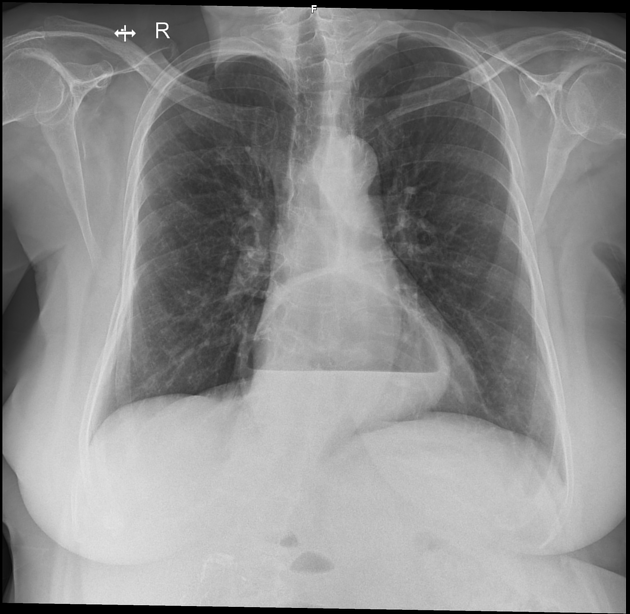
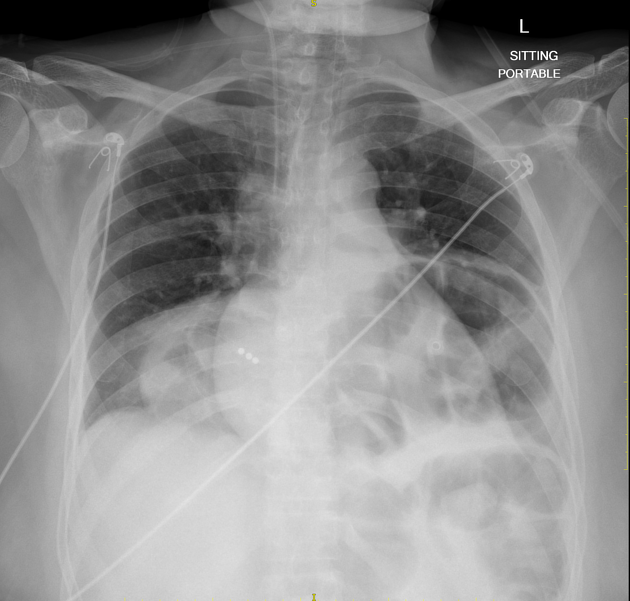
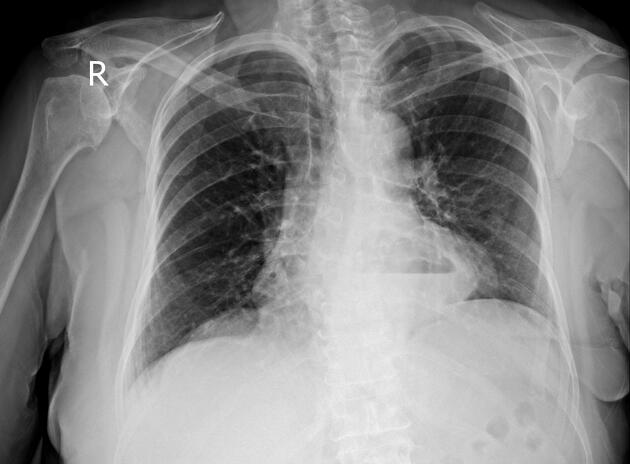
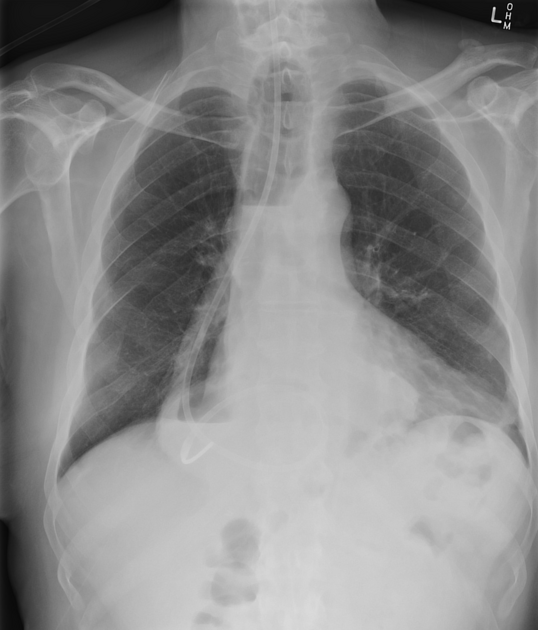
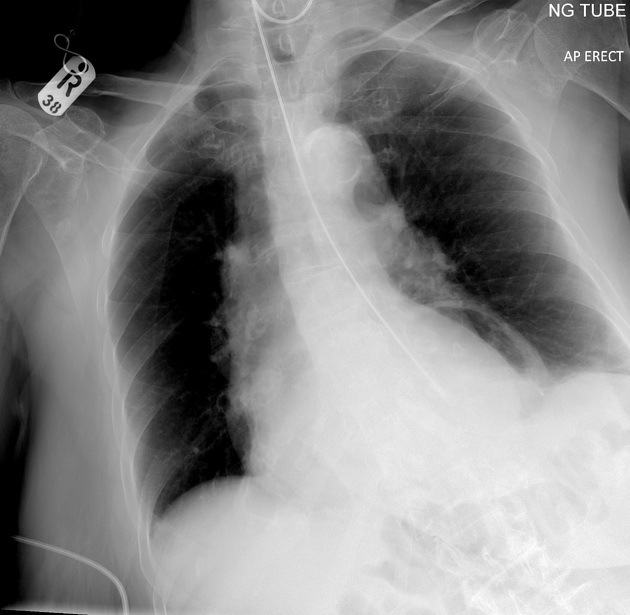
The gastric fundus may also be displaced above the diaphragm and present as a retrocardiac mass on a chest radiograph. The presence of an air-fluid level in the mass suggests the diagnosis.
Small, sliding hiatus hernias commonly reduce in the upright position. The mere presence of a sliding hiatus hernia is of limited clinical significance in most cases. The function of the lower esophageal sphincter and the presence of pathologic gastro-esophageal reflux are the crucial factors in producing symptoms and causing complications.
Rolling (paraesophageal) hiatus hernia
The rolling (paraesophageal) hiatus hernia is much less common than the sliding type. The GEJ remains in its normal location while a portion of the stomach herniates above the diaphragm.
Mixed rolling and sliding hiatus hernia
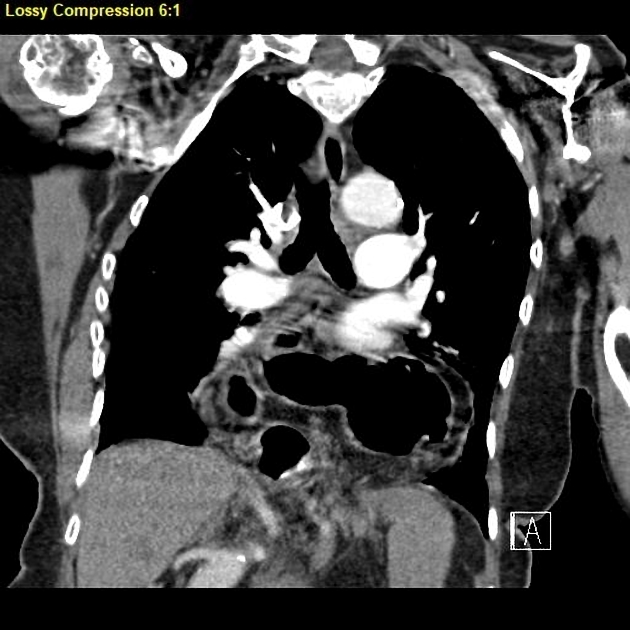
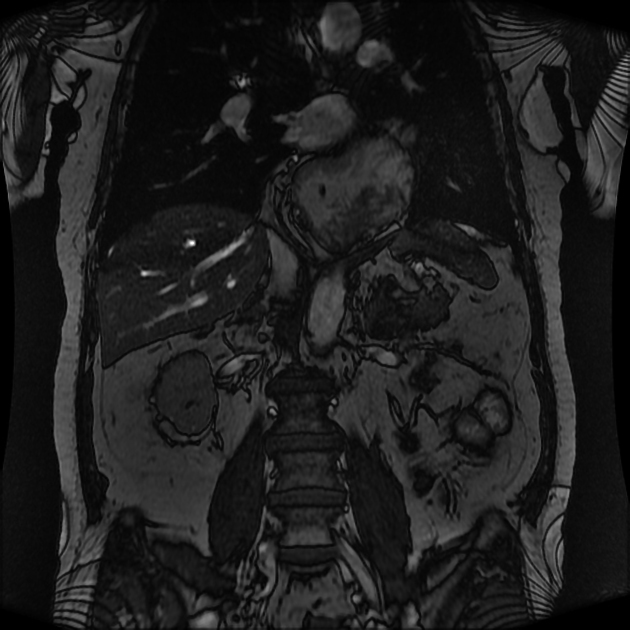
The mixed or compound hiatus hernia is the most common type of paraesophageal hernia. The GEJ is displaced into the thorax with a large portion of the stomach, which is usually abnormally rotated. Large paraesophageal hernias, with most of the stomach in the thorax, increase the risk for complications such as volvulus, obstruction, and ischemia 6.
Radiographic features
Plain radiograph
retrocardiac opacity with gas-fluid level
Fluoroscopy
numerous coarse thick gastric folds within the suprahiatal pouch
tortuous esophagus with an eccentric gastro-esophageal junction
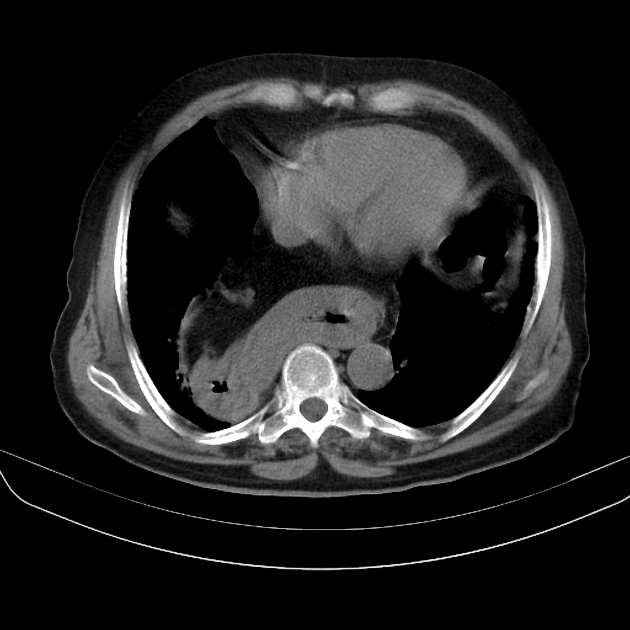
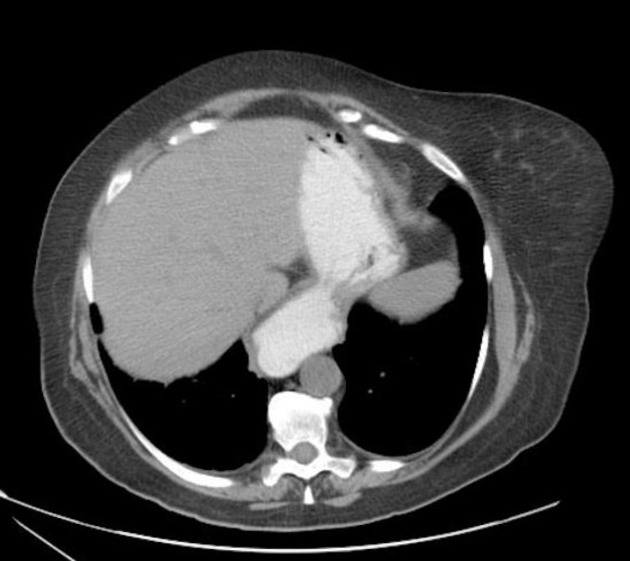
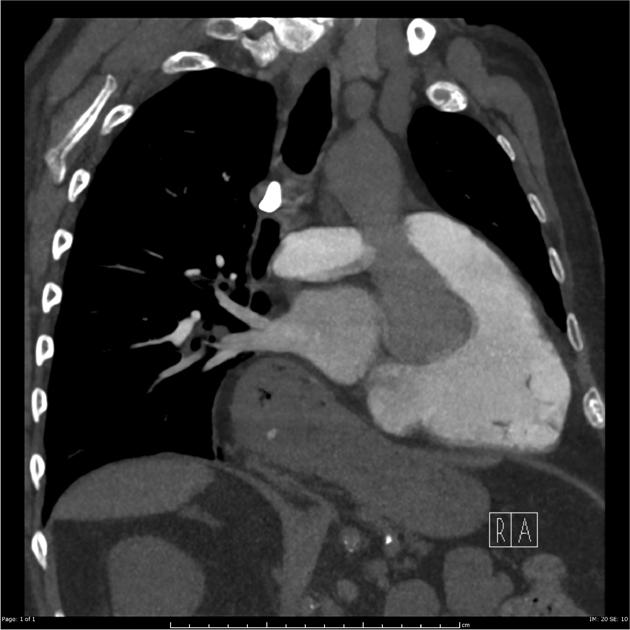
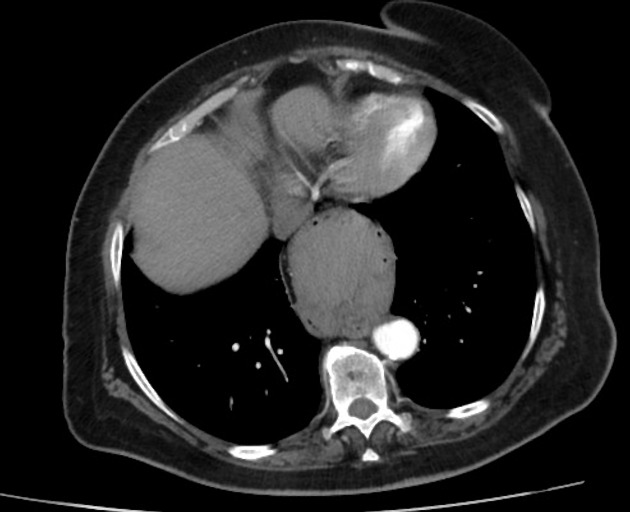
CT
-
focal fat collection in the middle mediastinum
omentum herniates through the phrenico-esophageal ligament
may see an increase in the fat surrounding the distal esophagus
-
paraesophageal hernia through a widened esophageal hiatus
visualize contents, size, orientation of herniated stomach within the lower thorax
herniated contents lie adjacent to the esophagus
-
widening of esophageal hiatus
dehiscence of diaphragmatic crura (>15 mm): increased distance between crura and esophageal wall
Preoperative assessment
In some institutions measurement of a hiatal surface area (HSA) has been proposed 7,8.
Treatment and prognosis
Symptomatic hiatus hernias, especially types 2-4, should be managed surgically 5.
Complications
a hiatus hernia containing the stomach may result in a gastric volvulus, which in turn presents as intestinal obstruction and may result in ischemia/infarction, or very rarely a tension gastrothorax, causing respiratory failure and eventual cardiac arrest
Cameron lesions: erosions in the setting of a large hiatus hernia
Differential diagnosis
On a frontal chest radiograph consider:
retrocardiac lung abscess
retrocardiac empyema
postoperative change: esophagectomy with gastric pull-up procedure
In the setting of trauma consider diaphragmatic rupture.
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.