Intramedullary spinal tumors are rare, representing 4-10% of all CNS tumors and <10% of all pediatric CNS neoplasms 5. They account for 20% of all intraspinal tumors in adults and 35% of all intraspinal tumors in children 8.
A long duration of symptoms prior to diagnosis is typical.
On this page:
Pathology
Classification
They can be classified according to many ways:
-
intramedullary neoplastic lesion
-
glial neoplasms: 90-95% of all intramedullary tumors 5
spinal ependymoma: 60% of all glial spinal cord tumors 5
spinal astrocytoma: 33% of all glial spinal cord tumors 5
spinal ganglioglioma: 1% of all glial spinal cord tumors 5
spinal glioblastoma (primary): 7.5% of all intramedullary gliomas and only 1.5% of all spinal cord tumors 11
-
non-glial neoplasms
-
highly vascular lesions
-
other rare lesions
-
-
-
intramedullary benign masses
Associations
Intramedullary spinal neoplasms are more common in patients with neurofibromatosis:
ependymomas occur more often in patients with NF2
astrocytomas occur more often in patients with NF1
Approximately 70% of intramedullary tumors are associated with cysts 3. Two types of cysts are recognized:
-
tumoral (or intratumoral) cysts
contained within the tumor itself
typically demonstrate peripheral enhancement
may result from necrosis, fluid secretion, or degeneration of the neoplasm
need to be resected along with the solid portion of the tumor because there is a high likelihood of neoplastic cells within the cyst wall
-
occurs in association with the following proportion of tumors 5,6,9
spinal ganglioglioma: in 46%
spinal ependymoma: in 22%
spinal astrocytoma: in 21%
spinal hemangioblastoma: in 2-4%
-
non-tumoral (or reactive) cysts
occur rostral or caudal to the solid portion of the tumor
occur due to dilatation of the central canal
do not enhance
present in 60% of all intramedullary spinal tumors
may resolve once the neoplasm is resected
Syringomyelia occurs in approximately 50% of all intramedullary tumors but is most frequently associated with hemangioblastomas 3.
Clinical presentation
The presentation of intramedullary tumors depends on their size and location. The most common presenting symptoms include back/neck pain, radicular pain, weakness, paresthesia, gait disturbance and bowel and bladder dysfunction. Brown-Sequard syndrome may occur. An uncommon presentation is acute headache due to subarachnoid hemorrhage 8.
In children, progressive scoliosis may be seen. Motor regression and frequent falls may be the presenting features in young children 7.
Symptoms are usually slowly progressive. Due to their non-specific nature, the diagnosis is often delayed. An exception is intramedullary metastastases, which are diagnosed within one month of symptom onset in up to 75% of cases 6.
Radiographic features
Plain radiograph
Widening of the interpedicular distance may be seen in less than 10% of cases
CT
Generally not useful because bony changes are relatively rare.
Myelography
the spinal cord can be enlarged
gradual subarachnoid space effacement
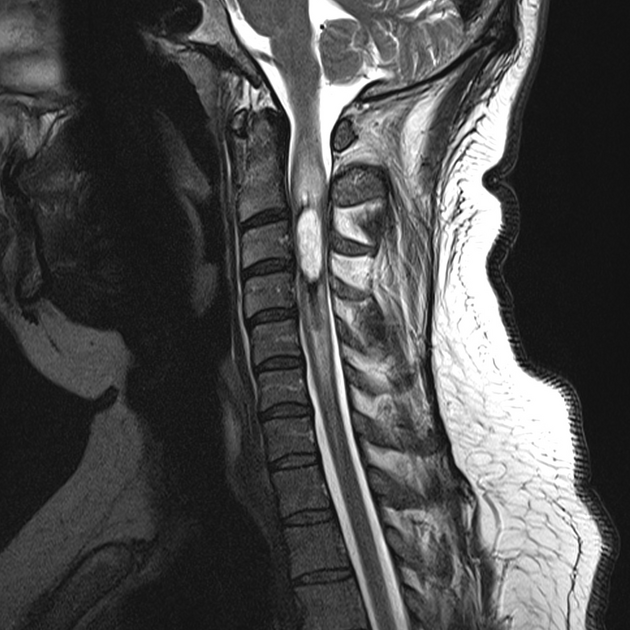
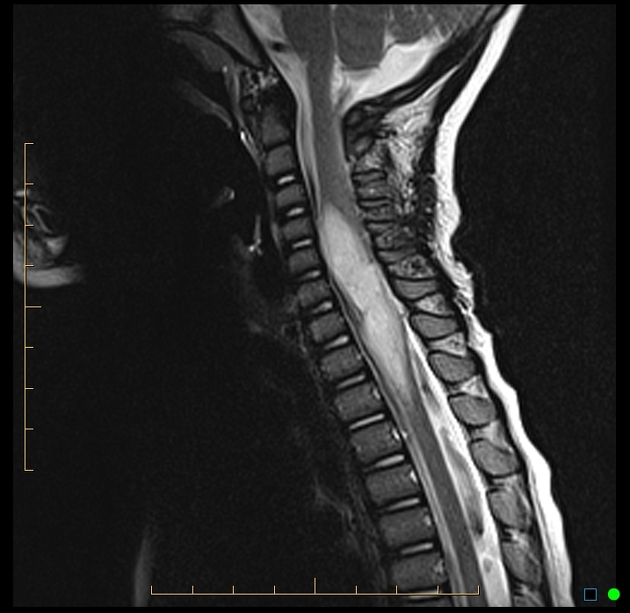
MRI
Three general characteristics of intramedullary neoplasms are recognized on MRI:
they cause either focal or diffuse spinal cord expansion
they produce high signal intensity on proton density and T2 weighted images
the vast majority show at least some contrast enhancement, in contrast to intracranial neoplasms, even low-grade intramedullary tumors enhance to some degree; however, the absence of enhancement does not exclude an intramedullary neoplasm in the presence of cord expansion 8,12
Differential diagnosis
Various lesions may mimic intramedullary tumors. The differential diagnosis of intramedullary tumors includes:
-
vascular lesions
-
cavernous malformation (cavernoma)
rounded regions of heterogeneous signal intensity on T1 and T2 weighted images due to blood
products of varying ages (“popcorn appearance”)
low signal intensity rim on T2 weighted images (hemosiderin)
hypointense “blooming” on gradient echo sequences (hemosiderin)
may demonstrate minimal enhancement on post-contrast images
minimal cord expansion or edema unless there has been recent hemorrhage
-
dural arteriovenous fistula (DAVF)-(type I AVM)
spinal cord may be normal size or enlarged
hyperintense on T2 weighted images (due to edema)
prominent vessels (flow voids) are usually present on the posterior aspect of the cord
variable enhancement on post-contrast images
typically located in the dorsal aspect of the lower thoracic cord and conus medullaris
-
spinal cord is usually enlarged
hyperintense on T2 weighted images and DWI
post-contrast enhancement may or may not be present (enhancement is usually present in the subacute stage)
signal intensity abnormality may be limited to the central grey matter or may involve most of the cross sectional area of the cord
signal abnormality typically extends over multiple vertebral body segments
can occur at any location in the cord but has a propensity for the upper thoracic or thoracolumbar regions
vertebral body T2 hyperintensity may occasionally be seen (due to concomitant infarction)
-
-
inflammatory lesions
-
demyelination (e.g. multiple sclerosis)
usually no spinal cord enlargement (enlargement is seen in 6-14% cases) 4
plaques are generally shorter than two vertebral body segments in length and involve less than half the cross-sectional area of the cord
characteristically peripherally located in the dorsal and lateral columns
isointense to hypointense on T1 weighted images (unlike brain plaques, cord plaques may not be visible as areas of hypointensity on T1 weighted imaegs)
hyperintense on T2 weighted images
signal abnormality is typically poorly marginated
plaque enhancement correlates with acute lesion activity (usually lasts less than two months)
in most patients additional lesions of variable enhancement are present in the brain and spinal cord (MS is solely confined to the spinal cord in 5-24% of patients 4)
-
variable enlargement of the spinal cord
hyperintense on T2 weighted images and iso- or hypointense on T1 weighted images
variable enhancement patterns (none, diffuse, patchy, peripheral)
lesions commonly extend for 3-4 spinal segments
lesions typically occupy greater than two thirds of the cross-sectional area of the cord
acute clinical course
-
core is hypointense on T1 weighted images and hyperintense on T2 weighted images
rim enhancement
cord expansion
may show restricted diffusion on DWI
may have adjacent vertebral or disc abnormalities
-
-
spinal cord contusion (acute)
isointense to hypointense on T1 weighted images, hyperintense on T2 weighted images
cord swelling
usually associated with other spinal injuries (osseous, disc, vascular)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.