Localized tenosynovial giant cell tumors are a subtype and are most commonly found in the fingers. On imaging, these lesions are commonly demonstrated as localized, solitary, subcutaneous soft tissue nodules, with low T1 and T2 signal and moderate enhancement.
Please see the overview article tenosynovial giant cell tumor for content common to both the localized-type and diffuse-type.
On this page:
Epidemiology
Typically, they present in the 3rd to 5th decades and have a slight female predilection with an F:M ratio of 1.5-2.1:1 4,13. They are the second most common soft tissue mass of the hand and wrist.
Clinical presentation
Clinically, localized tenosynovial giant cell tumors present as a slow-growing, painless mass 13.
Pathology
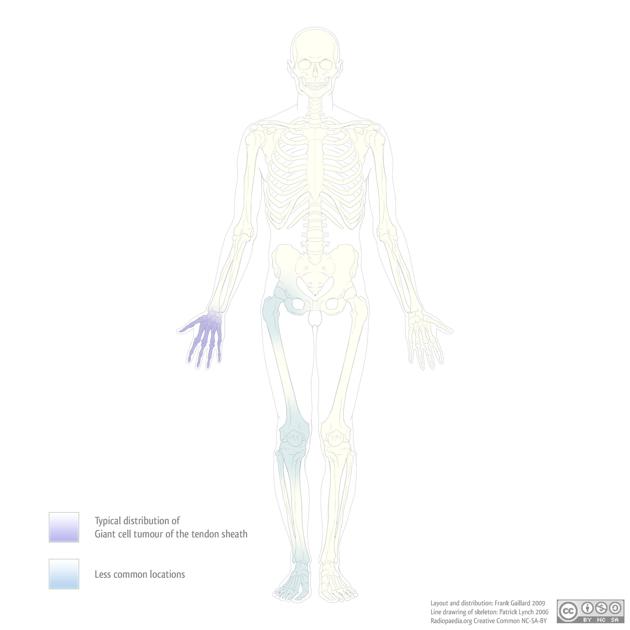
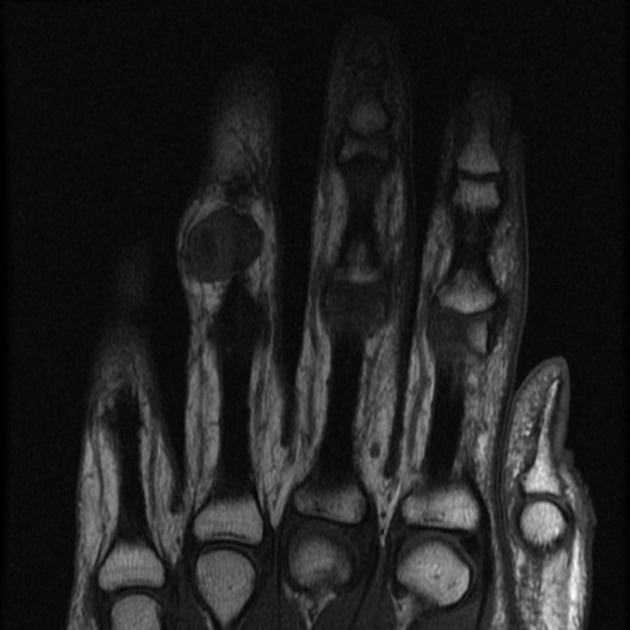
Localized tenosynovial giant cell tumors are most common in the fingers (~85%) where they are close to a tendon sheath or interphalangeal joint. Less commonly they can be found in the the wrist, ankle, foot, knee, and are rarely found in the elbow and hip 13. Localized tenosynovial giant cell tumors can be extra-articular (more common) or intra-articular 13.
Macroscopic appearance
Localized tenosynovial giant cell tumors are usually lobulated, well-cirumscribed masses between 0.5-4 cm and are white-to-grey with yellowish and brown regions 13.
Microscopic appearance
See main tenosynovial giant cell tumor article.
Radiographic features
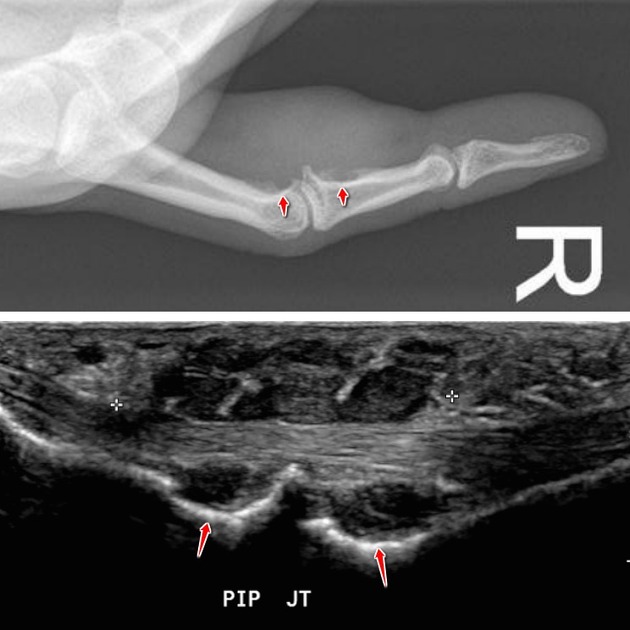
Plain radiograph
Tenosynovial giant cell tumors appear as soft tissue density peri-articular masses and can cause pressure erosion of adjacent bone, or rarely can invade the bone mimicking an intraosseous lesion 8,13. Periosteal reaction and calcification are uncommon 4,5.
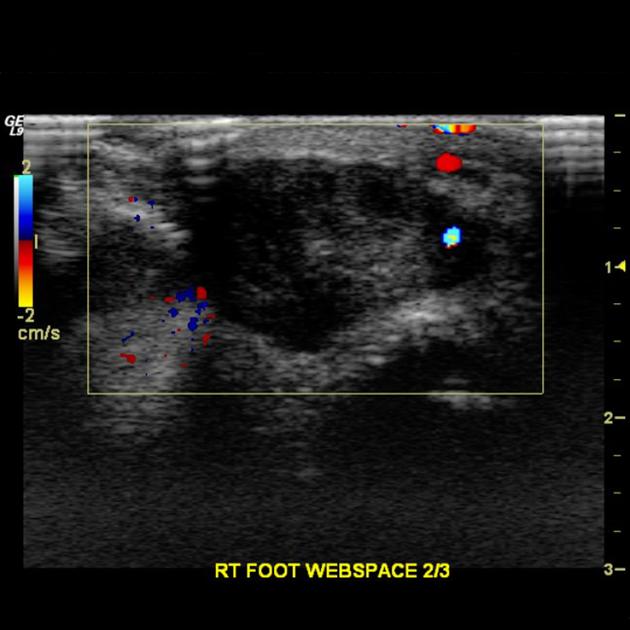
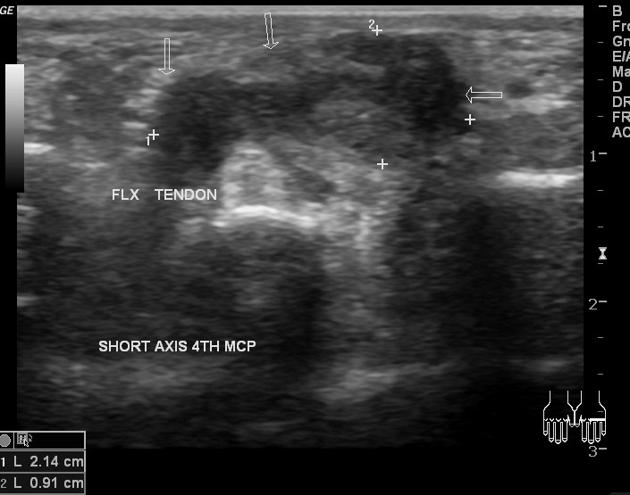
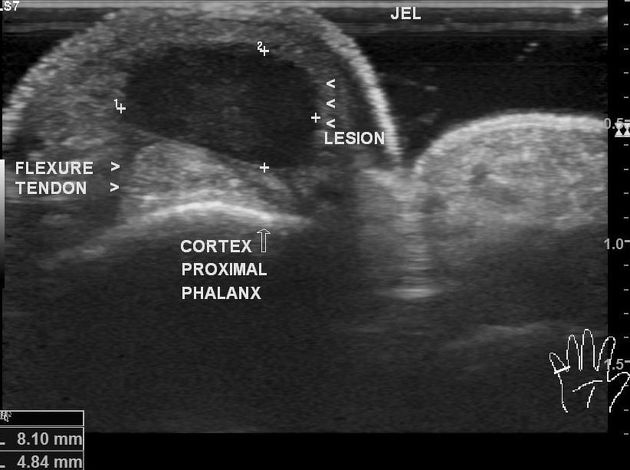
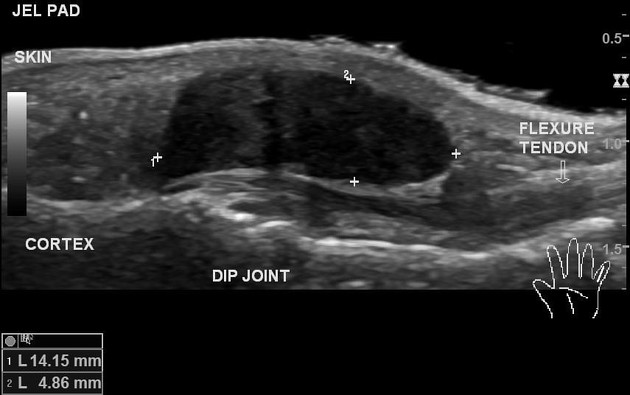
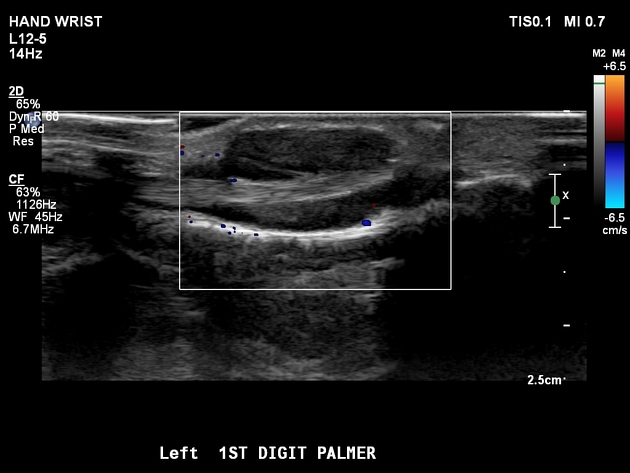
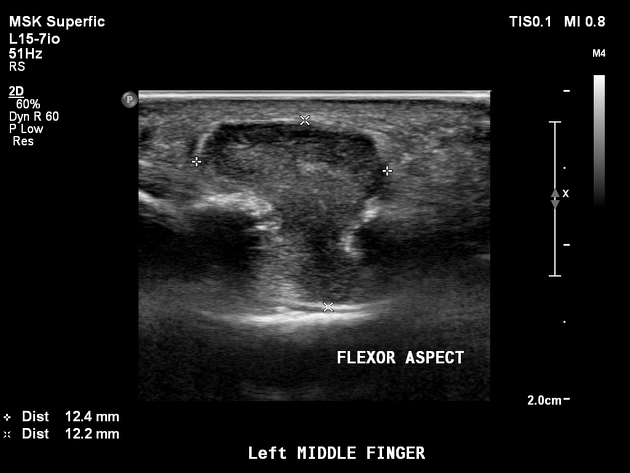
Ultrasound
Ultrasound is useful as it allows not only the characterization of the lesion but also is able to demonstrate the relationship with the adjacent tendon. On the dynamic scan, there is free movement of the tendon within the lesion. Typically they appear as:
associated with the volar surface of the digits
does not move with flexion or extension of adjacent tendons
usually homogeneously hypoechoic, although some heterogeneity may be seen in echotexture in a minority of cases 1
most will have some internal vascularity
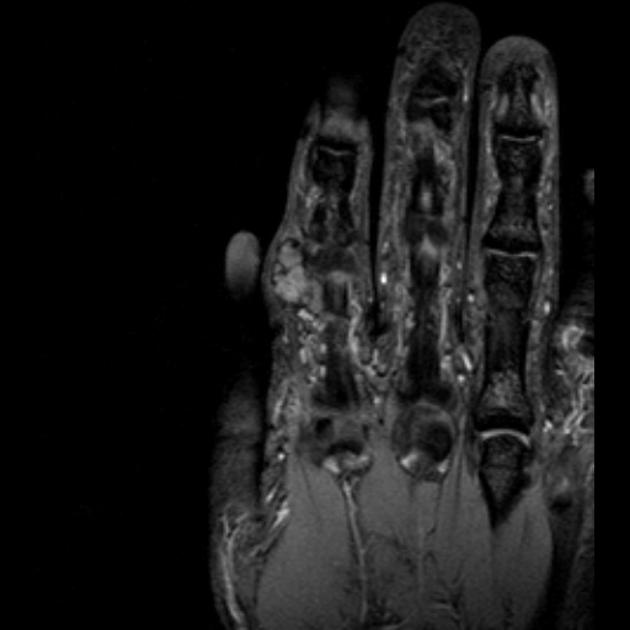
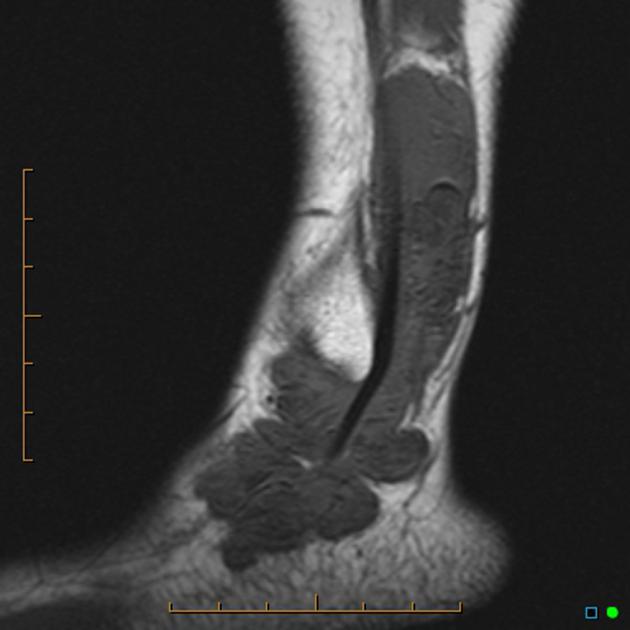
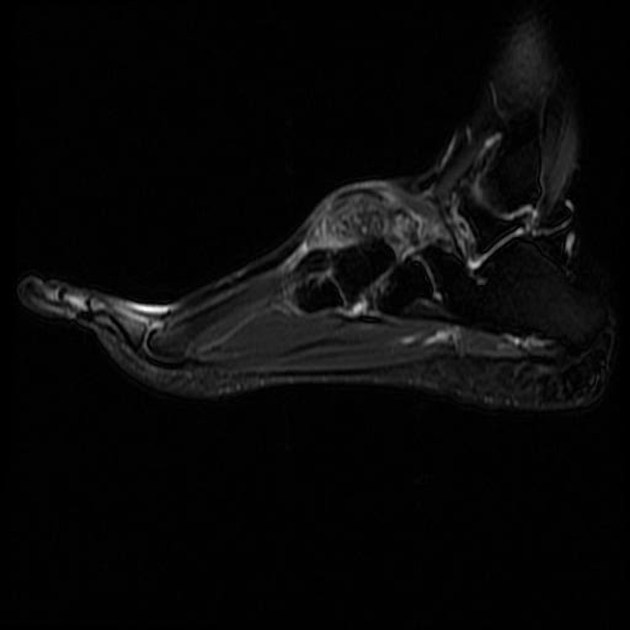
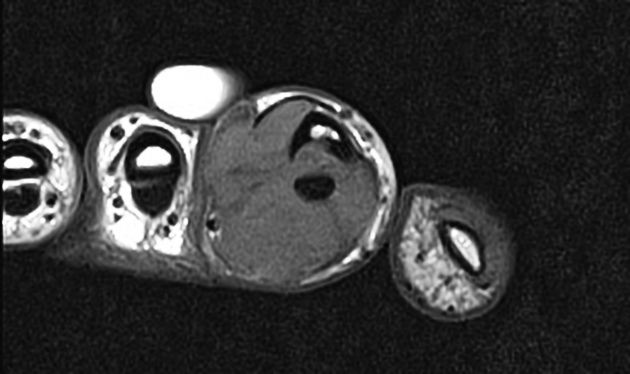
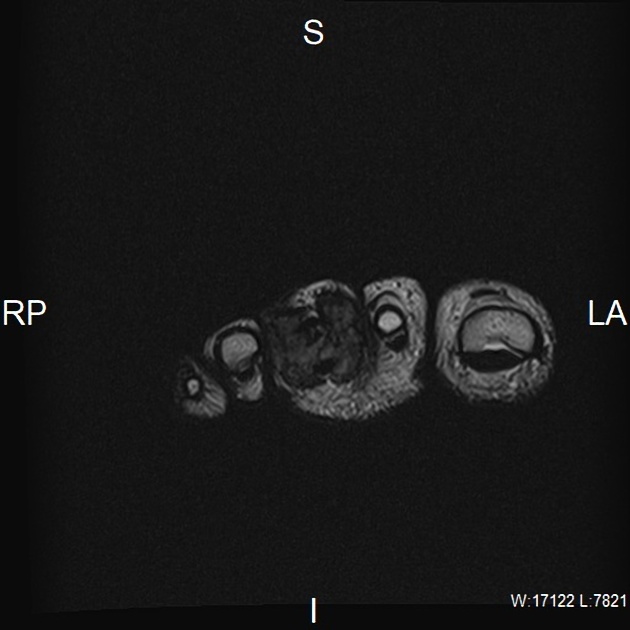
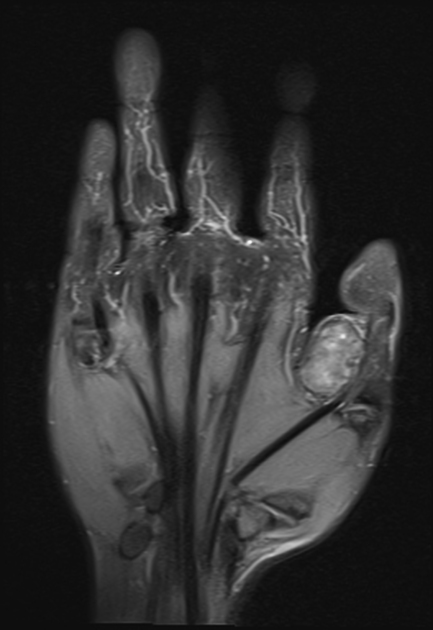
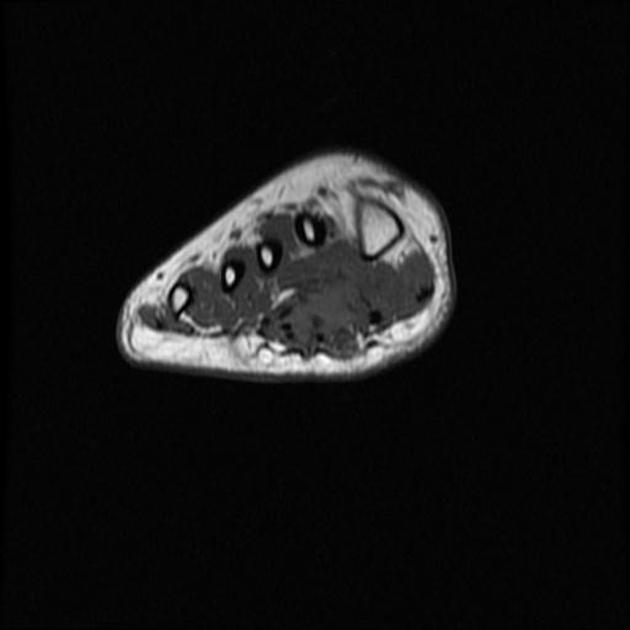
MRI
Localized type are a single mass with a capsule and small low T1/T2 intensity foci representing faint hemosiderin deposition 14. Bone erosion and neurovascular encasement can be seen 14.
T2/STIR signal is variable/heterogeneous due to differing amounts of hemosiderin, fat, fluid, fibrous and cellular elements 15.
Signal characteristics
T1: low to intermediate signal
-
T2
variable and heterogeneous
low to intermediate signal
high signal areas may be present likely due to joint fluid or inflamed synovium
STIR: variable and heterogeneous
GRE: low and may demonstrate blooming artifact
T1 C+ (Gd): often enhancing 6
Treatment and prognosis
Tenosynovial giant cell tumors are usually benign and local surgical excision usually suffices, with local recurrence (seen in 4-30% of cases) requiring more extensive surgery with or without radiotherapy being uncommon 1,13. Locally aggressive and malignant tenosynovial giant cell tumors can occur 11. Metastases can occur, most commonly to lymph nodes and lung 4.
Differential diagnosis
See main tenosynovial giant cell tumor article.















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.