The IASLC (International Association for the Study of Lung Cancer) 8th edition lung cancer staging system was introduced in 2016 and supersedes the IASLC 7th edition. It is a TNM staging system.
Standard-of-care lung cancer staging ideally should be performed in a multidisciplinary meeting using the information provided both from CT and FDG-PET-CT with further inputs from the histopathologic findings (pathological staging). The National Comprehensive Cancer Network (NCCN) guidelines recommend that FDG-PET-CT should be offered to all patients with non-small cell lung cancer (NSCLC) and that PET-positive findings for mediastinal nodes and/or distant disease require histopathological or other radiological confirmation 4.
The revised 9th edition of the TNM system for lung cancer is scheduled for 2024 6.
TNM system
T: primary tumor
Tx: primary tumor cannot be assessed or tumor proven by the presence of malignant cells in sputum or bronchial washings but not visualized by imaging or bronchoscopy
T0: no evidence of a primary tumor
Tis: carcinoma in situ - tumor measuring 3 cm or less and has no invasive component at histopathology
-
T1: tumor measuring 3 cm or less in greatest dimension surrounded by lung or visceral pleura without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e. not in the main bronchus)
-
T1a(mi): minimally invasive adenocarcinoma
tumor has an invasive component measuring 5 mm or less at histopathology
T1a ss: superficial spreading tumor in central airways (spreading tumor of any size but confined to the tracheal or bronchial wall)
T1a: tumor ≤1 cm in greatest dimension
T1b: tumor >1 cm but ≤2 cm in greatest dimension
T1c: tumor >2 cm but ≤3 cm in greatest dimension
-
-
T2: tumor >3 cm but ≤5 cm or tumor with any of the following features:
involves the main bronchus regardless of distance from the carina but without the involvement of the carina
invades visceral pleura
associated with atelectasis or obstructive pneumonitis that extends to the hilar region (involving part or all of the lung)
T2a: tumor >3 cm but ≤4 cm in greatest dimension
T2b: tumor >4 cm but ≤5 cm in greatest dimension
-
T3: tumor >5 cm but ≤7 cm in greatest dimension or associated with separate tumor nodule(s) in the same lobe as the primary tumor or directly invades any of the following structures:
chest wall (including the parietal pleura and superior sulcus)
parietal pericardium
-
T4:
-
tumor
>7 cm in greatest dimension or
associated with separate tumor nodule(s) in a different ipsilateral lobe than that of the primary tumor
or
-
invades any of the following structures
diaphragm
mediastinum
heart
great vessels
esophagus
vertebral body
carina
-
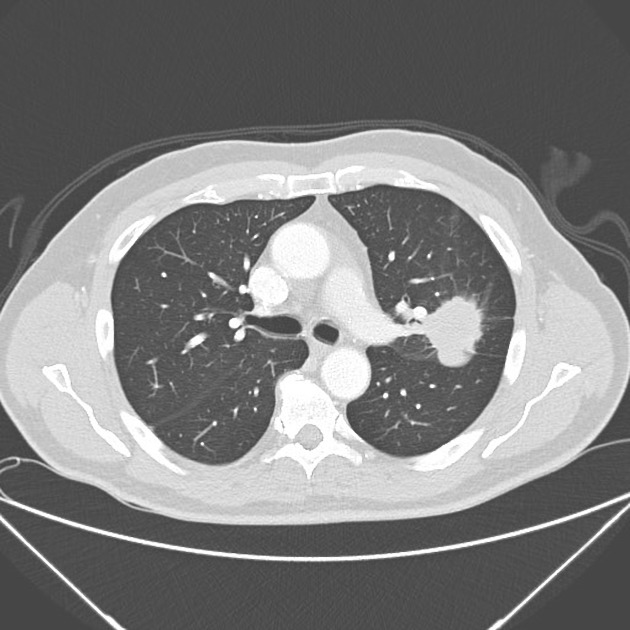
It is recommended that solid and non-solid lesions should be measured on the image that shows the greatest tumor dimension (on axial, coronal, or sagittal planes). Although those lesions that are part solid should be measured on both their largest average diameter and the largest diameter of the solid component, only the solid component measurement is to be used for staging 3. The solid component of subsolid lesions should be measured on a lung or intermediate window rather than mediastinal window 3.
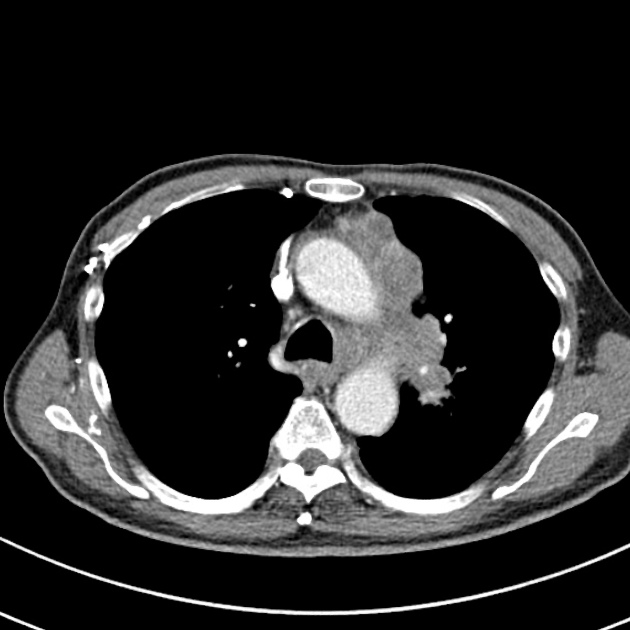
For those centrally located lung tumors associated with peripheral post-obstructive atelectasis, FDG-PET-CT is useful in further delineating the real tumor size and, leading to a more precise T staging and a smaller targeted volume in radiation treatment planning.
N: regional lymph node involvement
Nx: regional lymph nodes cannot be assessed
N0: no regional lymph node metastasis
N1: metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension
N2: metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s)
N3: metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s)
Please note that there has been no change in nodal involvement staging since the 7th edition of the IASLC.
PET-CT plays an important role in staging nodal disease. FDG uptake higher than the blood pool is suspicious, and uptake higher than the liver is highly concerning for nodal metastases. Endobronchial biopsy of an FDG-avid node is recommended to confirm the highest pathologic stage of disease 4.
M: distant metastasis
M0: no distant metastasis
-
M1: distant metastasis present
M1a: separate tumor nodule(s) in a contralateral lobe; tumor with pleural or pericardial nodule(s) or malignant pleural or pericardial effusions
-
M1b: single extrathoracic metastasis, involving a single organ or a single distant (nonregional) node
a single extrathoracic metastasis has a better survival and different treatment choices, which is why it has now been staged separately
M1c: multiple extrathoracic metastases in one or more organs
NB: The MX category is no longer used, it was removed in the 6th edition of the TNM system, if presence of metastases is not known the cancer is assigned M0 5.
There is a recommendation that the number of metastatic lesions, the larger diameter of individual metastatic deposits, and the number of involved organs should be stated in the radiological report 3. However, note that the site of the metastasis by itself is not a prognostic factor 4.
FDG PET-CT has a higher diagnostic value for the diagnosis of bone metastases compared to other methods. Therefore, bone scintigraphy is not recommended for staging purposes 4.
Histologic diagnosis is recommended when the adrenal gland is the only site of metastatic disease, given the risk of a false-positive 4.
Stage groupings
-
stage 0
TNM equivalent: Tis, N0, M0
-
stage Ia
TNM equivalent: T1, N0, M0
5-year survival: up to 92%
-
stage Ib
TNM equivalent: T2a, N0, M0
5-year survival: 68%
-
stage IIa
TNM equivalent: T2b, N0, M0
5-year survival: 60%
-
stage IIb
TNM equivalent: T1/T2, N1, M0 or T3, N0, M0
5-year survival: 53%
-
stage IIIa
TNM equivalent: T1/T2, N2, M0 or T3/T4, N1, M0 or T4, N0, M0
5-year survival: 36%
-
stage IIIb
TNM equivalent: T1/T2, N3, M0 or T3/T4, N2, M0
5-year survival: 26%
-
stage IIIc
TNM equivalent: T3/T4, N3, M0
5-year survival: 13%
-
stage IVa
TNM equivalent: any T, any N with M1a/M1b
5-year survival: 10%
-
stage IVb
TNM equivalent: any T, any N with M1c
5-year survival: 0%





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.