Osteoarthritis
Updates to Article Attributes
Osteoarthritis (OA), also known as degenerative joint disease (DJD), is the most common form of arthritis, being widely prevalent with high morbidity and social cost.
Terminology
Some authors prefer the term osteoarthrosis instead of osteoarthritis as some authors do not believe in an inflammatory cause as might be suggested by the suffix "itis". The condition is sometimes called non-erosive osteoarthritis, to differentiate it from erosive osteoarthritis, although this is considered a form of osteoarthritis 6.
Epidemiology
Osteoarthritis is common, affecting ~25% of adults 7. The prevalence increases with age. In the age group below 50 years, men are more often affected, while in the older population the disease is more common in women. It is estimated that over 300 million people in the world suffered from OAosteoarthritis in 2017 13.
Clinical presentation
Patients present with decreased function from joint pain, instability, and stiffness 7,10. The pain is typically worsened by activity and decreases at rest; in later disease stages, it may become continuous 12. Many cases of radiological OAosteoarthritis are asymptomatic and conversely clinically apparent OAosteoarthritis may not manifest radiographic change 9,10.
Pathology
The pathogenesis and pathophysiology of OAosteoarthritis are yet to be fully understood 7. Despite emphasis being placed on articular cartilage degeneration, the remainder of the joint is involved including bone remodelling, osteophyte formation, ligamentous laxity, periarticular muscle weakness, and synovitis 8,10.
Classification
Osteoarthritis can be 19:
-
primary (idiopathic)
- absence of an antecedent insult
- strong genetic component with the disease primarily affecting middle-aged women 5
-
secondary
- abnormal mechanical forces (e.g. occupational stress, obesity)
- previous joint injury
-
post-traumatic osteoarthritis
- accounts for ~12% of all
OAosteoarthritis 11 - major cause in young adults 9
- accounts for ~12% of all
- prior surgery
- crystal deposition (e.g. gout, CPPD)
- inflammatory arthritis (e.g. rheumatoid arthritis, seronegative spondyloarthritis)
- haemochromatosis
-
post-traumatic osteoarthritis
Distribution
OAOsteoarthritis can affect both the axial and appendicular skeleton. The most common peripheral joints affected include ref:
Risk factors
Strong risk factors for developing OAosteoarthritis include 7,10:
- obesity
- increasing age
- female sex (particularly between the age 50 and 80)
- family history
Radiographic features
Key radiographic features are joint space narrowing (JSN), subchondral sclerosis, and osteophytosis. If all three of these findings are not present, another diagnosis should be considered. Recently, with increasing use of MRI in the assessment of OAosteoarthritis, other findings have been studied, such as bone marrow lesions and synovitis.
- joint space narrowing
- characteristically asymmetric
- least specific: present in many other pathological processes
- subchondral sclerosis
- sclerotic changes occur at joint margins
- frequently seen unless severe osteoporosis is present
- osteophytosis
- i.e. development of osteophytes
- common degenerative joint disease finding
- will also be diminished in the setting of osteoporosis
- some osteophytes carry eponymous names, e.g. Heberden nodes, Bouchard nodes
- joint erosions
- several joints may exhibit degenerative erosions 1:
- subchondral cysts
- also known as geodes
- cystic formations that occur around joints in a variety of disorders, including, rheumatoid arthritis, calcium pyrophosphate dihydrate crystal deposition disease (CPPD), and avascular necrosis
- bone marrow lesions
(BML)14,16- visible on MRI as bone marrow oedema-like lesions, often adjacent to areas of cartilage damage - likely representing early
OAosteoarthritis changes - have been shown to correlate with joint pain and progression of cartilage loss
- may progress to subchondral cysts
- visible on MRI as bone marrow oedema-like lesions, often adjacent to areas of cartilage damage - likely representing early
-
synovitis
- a non-specific finding, present also in other diseases, including inflammatory and infectious conditions
- present in up to 50% of
thepatients withOAosteoarthritis 14 - according to some authors it may be correlated with pain, disease severity and progression 14,15
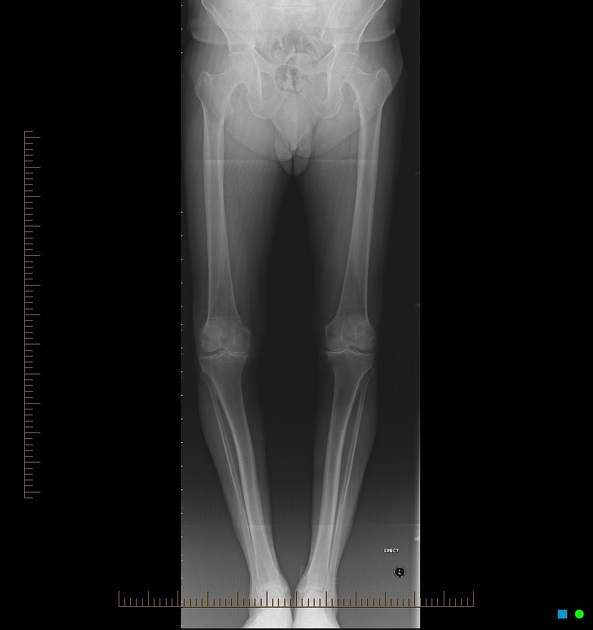
Plain radiograph
Plain radiograph is the most commonly used modality in assessment of OAosteoarthritis due to its availability and low cost. It can detect bony features of OAosteoarthritis, such as joint space loss, subchondral cysts and sclerosis, and osteophytes. It is, however, relatively insensitive to early disease changes. Other limitations are a lack of assessment of soft-tissue structures and low intrareader reliability 17.
Scoring systems used to assess the severity of OAosteoarthritis on radiographs include 17,18:
- Kellgren and Lawrence classification
- Osteoarthritis Research Society International (OARSI) atlas
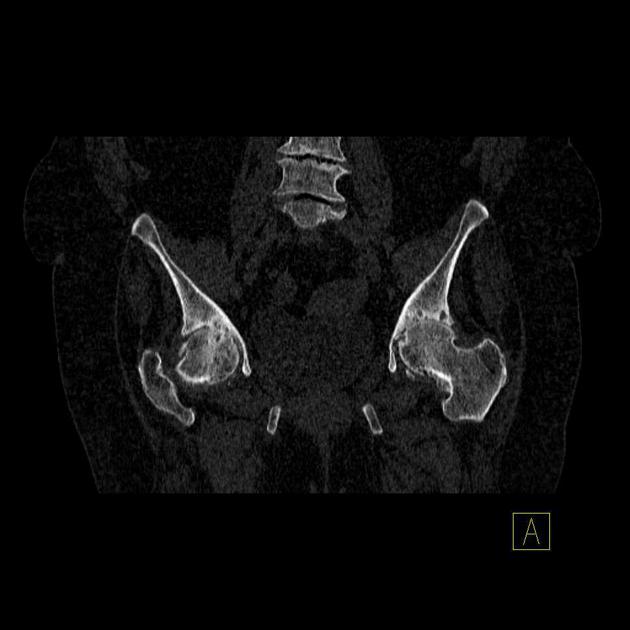
CT
CT has excellent accuracy in assessing bony OAosteoarthritis changes. It is especially useful in the assessment of the facet joints. In order to reliably assess the articular cartilage, an arthro-CT must be performed.
Ultrasound
Ultrasound is not routinely used in OAosteoarthritis. The assessment of the bony structure and deep joint structures using this modality is impossible. However, it is useful in detecting joint effusion, synovitis, and osteophytes. It can also act as guidance in joint interventions.
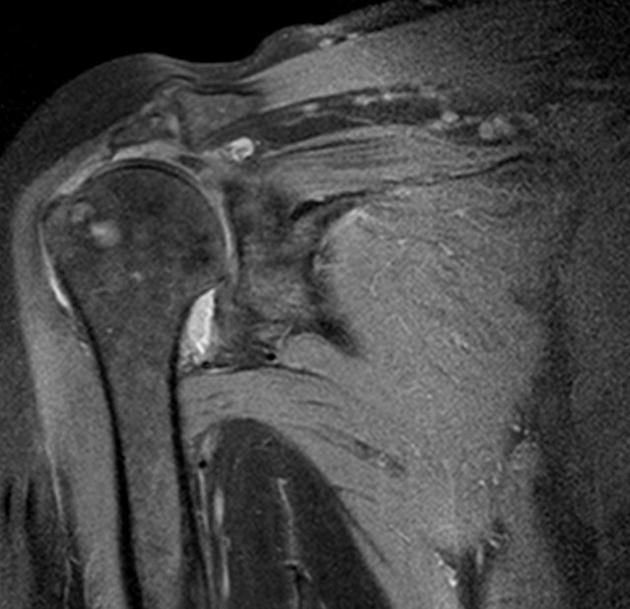
MRI
MRI can very accurately assess both bones and soft-tissue joint structures. It can detect bone marrow changes and cartilage loss, both of which are early OAosteoarthritis changes and are not visible on radiographs. On conventional MR, articular cartilage is best assessed using fluid-sensitive sequences with fat suppression; with the advent of new methods of cartilage quantification and composition assessment - currently used in research - the sensitivity is further increased. Contrast administration enhances the visualisation of synovitis.
Several scoring systems using MRI assessment of OAosteoarthritis of the knee have been proposed 14:
- Whole-Organ Magnetic Resonance Imaging Score
- Knee Osteoarthritis Scoring System
- Boston Leeds Osteoarthritis Knee Score
Nuclear medicine
While not routinely used in clinical practice, nuclear medicine studies can provide information about multiple joints in one examination. The changes in the joints with OAosteoarthritis show increased radiotracer uptake due to reactive bone turnover. The potential disadvantage of a poor anatomical resolution can be solved by using hybrid imaging 14.
Nuclear medicine examination used in the assessment of OAosteoarthritis are:
- scintigraphy with Tc-99m hydroxymethylene diphosphonate (HDP)
- PET with 18FDG or 18F
Treatment and prognosis
There is no effective treatment to slow or reverse the changes of osteoarthritis 7. The mainstays of treatment include exercise, walking aids, bracing, and analgesia (including intra-articular steroid injections) 8. Arthroplasty can result in improved function and reduced pain 10.
History and etymology
The term "osteoarthritis" was introduced as a synonym for rheumatoid arthritis by English physician, John K Spender (1829-1916) in 1886, however, it was not until 1907 that the English physician Archibald E Garrod (1857-1936) applied the term to the condition that is now considered to be osteoarthritis 19-21.
References changed:
- 1. William E. Brant, Clyde A. Helms. Fundamentals of Diagnostic Radiology. (2007) ISBN: 9780781765183 - <a href="http://books.google.com/books?vid=ISBN9780781765183">Google Books</a>
- 2. Jacobson J, Girish G, Jiang Y, Sabb B. Radiographic Evaluation of Arthritis: Degenerative Joint Disease and Variations. Radiology. 2008;248(3):737-47. <a href="https://doi.org/10.1148/radiol.2483062112">doi:10.1148/radiol.2483062112</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/18710973">Pubmed</a>
- 3. Lane N & Kremer L. Radiographic Indices for Osteoarthritis. Rheum Dis Clin North Am. 1995;21(2):379-94. - <a href="https://www.ncbi.nlm.nih.gov/pubmed/7631034">Pubmed</a>
- 4. Lane N, Nevitt M, Genant H, Hochberg M. Reliability of New Indices of Radiographic Osteoarthritis of the Hand and Hip and Lumbar Disc Degeneration. J Rheumatol. 1993;20(11):1911-8. - <a href="https://www.ncbi.nlm.nih.gov/pubmed/8308778">Pubmed</a>
- 5. Fernández-Moreno M, Rego I, Carreira-Garcia V, Blanco F. Genetics in Osteoarthritis. Curr Genomics. 2008;9(8):542-7. <a href="https://doi.org/10.2174/138920208786847953">doi:10.2174/138920208786847953</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/19516961">Pubmed</a>
- 6. Marshall M, Nicholls E, Kwok W et al. Erosive Osteoarthritis: A More Severe Form of Radiographic Hand Osteoarthritis Rather Than a Distinct Entity? Ann Rheum Dis. 2015;74(1):136-41. <a href="https://doi.org/10.1136/annrheumdis-2013-203948">doi:10.1136/annrheumdis-2013-203948</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/24095935">Pubmed</a>
- 7. Chen D, Shen J, Zhao W et al. Osteoarthritis: Toward a Comprehensive Understanding of Pathological Mechanism. Bone Res. 2017;5(1):16044. <a href="https://doi.org/10.1038/boneres.2016.44">doi:10.1038/boneres.2016.44</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/28149655">Pubmed</a>
- 8. Kolasinski S, Neogi T, Hochberg M et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72(2):220-33. <a href="https://doi.org/10.1002/art.41142">doi:10.1002/art.41142</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/31908163">Pubmed</a>
- 9. Zhang Y & Jordan J. Epidemiology of Osteoarthritis. Clin Geriatr Med. 2010;26(3):355-69. <a href="https://doi.org/10.1016/j.cger.2010.03.001">doi:10.1016/j.cger.2010.03.001</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/20699159">Pubmed</a>
- 10. Litwic A, Edwards M, Dennison E, Cooper C. Epidemiology and Burden of Osteoarthritis. Br Med Bull. 2013;105(1):185-99. <a href="https://doi.org/10.1093/bmb/lds038">doi:10.1093/bmb/lds038</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/23337796">Pubmed</a>
- 11. Punzi L, Galozzi P, Luisetto R et al. Post-Traumatic Arthritis: Overview on Pathogenic Mechanisms and Role of Inflammation. RMD Open. 2016;2(2):e000279. <a href="https://doi.org/10.1136/rmdopen-2016-000279">doi:10.1136/rmdopen-2016-000279</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/27651925">Pubmed</a>
- 13. Kloppenburg M & Berenbaum F. Osteoarthritis Year in Review 2019: Epidemiology and Therapy. Osteoarthritis Cartilage. 2020;28(3):242-8. <a href="https://doi.org/10.1016/j.joca.2020.01.002">doi:10.1016/j.joca.2020.01.002</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/31945457">Pubmed</a>
- 14. Braun H & Gold G. Diagnosis of Osteoarthritis: Imaging. Bone. 2012;51(2):278-88. <a href="https://doi.org/10.1016/j.bone.2011.11.019">doi:10.1016/j.bone.2011.11.019</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/22155587">Pubmed</a>
- 15. Guermazi A, Hayashi D, Roemer F et al. Severe Radiographic Knee Osteoarthritis--Does Kellgren and Lawrence Grade 4 Represent End Stage Disease?--The MOST Study. Osteoarthritis Cartilage. 2015;23(9):1499-505. <a href="https://doi.org/10.1016/j.joca.2015.04.018">doi:10.1016/j.joca.2015.04.018</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/25929973">Pubmed</a>
- 16. Tanamas S, Wluka A, Pelletier J et al. Bone Marrow Lesions in People with Knee Osteoarthritis Predict Progression of Disease and Joint Replacement: A Longitudinal Study. Rheumatology. 2010;49(12):2413-9. <a href="https://doi.org/10.1093/rheumatology/keq286">doi:10.1093/rheumatology/keq286</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/20823092">Pubmed</a>
- 17. Hayashi D, Roemer F, Guermazi A. Imaging for Osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):161-9. <a href="https://doi.org/10.1016/j.rehab.2015.12.003">doi:10.1016/j.rehab.2015.12.003</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/26797169">Pubmed</a>
- 18. Altman R & Gold G. Atlas of Individual Radiographic Features in Osteoarthritis, Revised. Osteoarthritis Cartilage. 2007;15 Suppl A:A1-56. <a href="https://doi.org/10.1016/j.joca.2006.11.009">doi:10.1016/j.joca.2006.11.009</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/17320422">Pubmed</a>
- 19. Sangha O. Epidemiology of Rheumatic Diseases. Rheumatology (Oxford). 2000;39 Suppl 2(suppl_2):3-12. <a href="https://doi.org/10.1093/rheumatology/39.suppl_2.3">doi:10.1093/rheumatology/39.suppl_2.3</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/11276800">Pubmed</a>
- 20. Dronamraju K. Profiles in Genetics: Archibald E. Garrod (1857-1936). Am J Hum Genet. 1992;51(1):216-9. <a href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1682897">PMC1682897</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/1609799">Pubmed</a>
- 21. British Medical Journal Publishing Group. JOHN KENT SPENDER, M.D.Lond. BMJ. 1916;1(2886):606-7. <a href="https://doi.org/10.1136/bmj.1.2886.606-c">doi:10.1136/bmj.1.2886.606-c</a>
- 1. William E. Brant, Clyde A. Helms. The Brant and Helms Solution: Fundamentals of Diagnostic Radiology, Third Edition, Plus Integrated Content Website (4 Vol. Set). (2006) ISBN: 0781765188
- 2. Jacobson J, Girish G, Jiang Y, Sabb B. Radiographic Evaluation of Arthritis: Degenerative Joint Disease and Variations. Radiology. 2008;248(3):737-47. <a href="https://doi.org/10.1148/radiol.2483062112">doi:10.1148/radiol.2483062112</a>
- 3. Lane N & Kremer L. Radiographic Indices for Osteoarthritis. Rheum Dis Clin North Am. 1995;21(2):379-94. <a href="https://www.ncbi.nlm.nih.gov/pubmed/7631034">PMID 7631034</a>
- 4. Lane N, Nevitt M, Genant H, Hochberg M. Reliability of New Indices of Radiographic Osteoarthritis of the Hand and Hip and Lumbar Disc Degeneration. J Rheumatol. 1993;20(11):1911-8. <a href="https://www.ncbi.nlm.nih.gov/pubmed/8308778">PMID 8308778</a>
- 5. Fernandez-Moreno M, Rego I, Carreira-Garcia V, Blanco F. Genetics in Osteoarthritis. CG. 2008;9(8):542-7. <a href="https://doi.org/10.2174/138920208786847953">doi:10.2174/138920208786847953</a>
- 6. Marshall M, Nicholls E, Kwok W et al. Erosive Osteoarthritis: A More Severe Form of Radiographic Hand Osteoarthritis Rather Than a Distinct Entity? Ann Rheum Dis. 2013;74(1):136-41. <a href="https://doi.org/10.1136/annrheumdis-2013-203948">doi:10.1136/annrheumdis-2013-203948</a>
- 7. Chen D, Shen J, Zhao W et al. Osteoarthritis: Toward a Comprehensive Understanding of Pathological Mechanism. Bone Res. 2017;5(1):1-13. <a href="https://doi.org/10.1038/boneres.2016.44">doi:10.1038/boneres.2016.44</a>
- 8. Kolasinski S, Neogi T, Hochberg M et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72(2):220-33. <a href="https://doi.org/10.1002/art.41142">doi:10.1002/art.41142</a>
- 9. Zhang Y & Jordan J. Epidemiology of Osteoarthritis. Clinics in Geriatric Medicine. 2010;26(3):355-69. <a href="https://doi.org/10.1016/j.cger.2010.03.001">doi:10.1016/j.cger.2010.03.001</a>
- 10. Litwic A, Edwards M, Dennison E, Cooper C. Epidemiology and Burden of Osteoarthritis. British Medical Bulletin. 2013;105(1):185-99. <a href="https://doi.org/10.1093/bmb/lds038">doi:10.1093/bmb/lds038</a>
- 11. Punzi L, Galozzi P, Luisetto R et al. Post-Traumatic Arthritis: Overview on Pathogenic Mechanisms and Role of Inflammation. RMD Open. 2016;2(2):e000279. <a href="https://doi.org/10.1136/rmdopen-2016-000279">doi:10.1136/rmdopen-2016-000279</a>
- 13. Kloppenburg M & Berenbaum F. Osteoarthritis Year in Review 2019: Epidemiology and Therapy. Osteoarthritis and Cartilage. 2020;28(3):242-8. <a href="https://doi.org/10.1016/j.joca.2020.01.002">doi:10.1016/j.joca.2020.01.002</a>
- 14. Braun H & Gold G. Diagnosis of Osteoarthritis: Imaging. Bone. 2012;51(2):278-88. <a href="https://doi.org/10.1016/j.bone.2011.11.019">doi:10.1016/j.bone.2011.11.019</a>
- 15. Guermazi A, Hayashi D, Roemer F et al. Severe Radiographic Knee Osteoarthritis – Does Kellgren and Lawrence Grade 4 Represent End Stage Disease? – the MOST Study. Osteoarthritis and Cartilage. 2015;23(9):1499-505. <a href="https://doi.org/10.1016/j.joca.2015.04.018">doi:10.1016/j.joca.2015.04.018</a>
- 16. Tanamas S, Wluka A, Pelletier J et al. Bone Marrow Lesions in People with Knee Osteoarthritis Predict Progression of Disease and Joint Replacement: A Longitudinal Study. Rheumatology. 2010;49(12):2413-9. <a href="https://doi.org/10.1093/rheumatology/keq286">doi:10.1093/rheumatology/keq286</a>
- 17. Hayashi D, Roemer F, Guermazi A. Imaging for Osteoarthritis. Annals of Physical and Rehabilitation Medicine. 2016;59(3):161-9. <a href="https://doi.org/10.1016/j.rehab.2015.12.003">doi:10.1016/j.rehab.2015.12.003</a>
- 18. Altman R & Gold G. Atlas of Individual Radiographic Features in Osteoarthritis, Revised. Osteoarthritis and Cartilage. 2007;15:A1-A56. <a href="https://doi.org/10.1016/j.joca.2006.11.009">doi:10.1016/j.joca.2006.11.009</a>
- 19. Sangha O. Epidemiology of Rheumatic Diseases. Rheumatology. 2000;39(suppl_2):3-12. <a href="https://doi.org/10.1093/rheumatology/39.suppl_2.3">doi:10.1093/rheumatology/39.suppl_2.3</a>
- 20. Dronamraju K. Profiles in Genetics: Archibald E. Garrod (1857-1936). Am J Hum Genet. 1992;51(1):216-9. <a href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1682897">PMC1682897</a>
- 21. Obituitary - John Kent Spender, M.D.Lond. Br Med J. 1916 Apr 22;1(2886):606–7. PMCID: PMC2347337.














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.