Osteoarthritis (OA) of the knee is very common and is a major cause of morbidity, especially in the older population. For a general discussion on osteoarthritis, please see the general osteoarthritis article.
On this page:
Terminology
The term early osteoarthritis of the knee has been proposed and has been defined as meeting three main criteria 9:
knee pain
Kellgren-Lawrence grade 2 or less on radiographs
arthroscopic cartilage lesion and/or OA-related MRI findings such as subchondral bone marrow lesions and/or cartilage and meniscal degeneration
Epidemiology
Knee OA is very common and is the most common joint disease in the elderly. It is estimated to affect ~12.5% of patients >45 years 8 in the community.
The medial femorotibial joint compartment is more commonly affected and often more severe than the lateral 2.
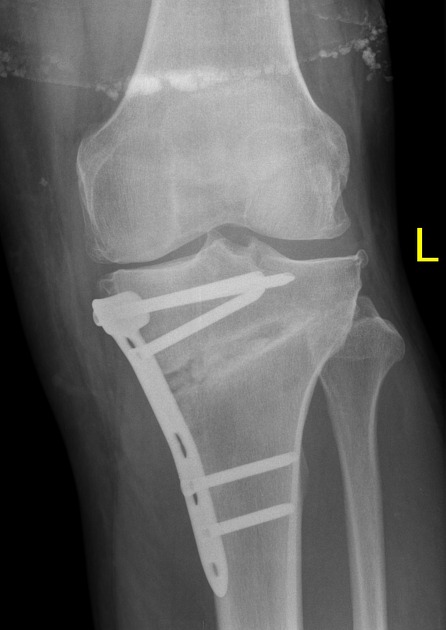
Radiographic features
The hallmarks of knee osteoarthritis are the same for most other joints 6:
-
joint space narrowing
usually asymmetric, typically of the medial tibiofemoral compartment, and/or patellofemoral compartment 3
<3 mm on weight-bearing knee radiographs is considered a finding of absolute joint space narrowing with a normal joint space >5 mm 7
weight-bearing radiographs will demonstrate more joint space narrowing than non-weight-bearing radiographs, hence affecting the radiographic severity 7,8
subchondral sclerosis
marginal osteophytes
subchondral cysts (geodes)
altered shape of the femoral condyles and tibial plateau
Plain radiographs are the workhorse of imaging including follow-up, although there is a poor correlation between radiographic findings and clinical symptoms 1,2.
The initial study of any patient with suspicion of knee osteoarthritis should include a Rosenberg view, a PA radiograph with weight-bearing and 45 degrees of flexion, which is more sensitive to detect joint space narrowing 5.
Grading
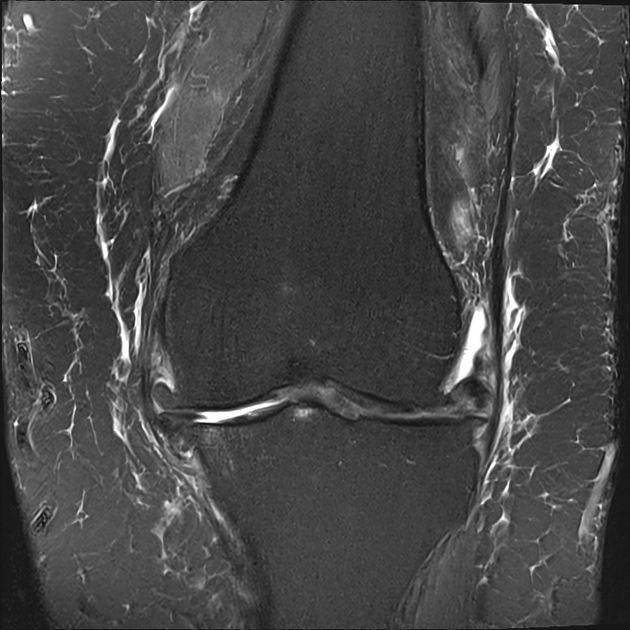
MRI
The following features are seen additionally on MRI 1,10:
effusion and synovial thickening / synovitis
subchondral bone marrow edema and/or cysts
cartilaginous defects (partial or full-thickness)
bursitis
Treatment and prognosis
Non-operative management involves simple analgesia and weight loss. However, patients will often eventually require joint replacement. Total knee joint replacement is effective. Unicompartmental joint replacement may be considered in some institutions for cases where the disease is predominantly isolated to a single joint compartment.
Differential diagnosis
Other causes of degenerative joint disease, for example:













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.