Pituitary apoplexy is an acute clinical condition caused by either hemorrhagic or non-hemorrhagic necrosis of the pituitary gland. Although presentation is variable, it typically comprises headache, visual deficits, ophthalmoplegia, and altered mental status. An existing pituitary macroadenoma is usually present (60-90%), but occasionally it happens in normal glands.
On this page:
Epidemiology
The demographics generally follow that of pituitary macroadenomas.
Risk factors
Predisposing factors include 2:
medical treatment of a prolactinoma (especially with bromocriptine) 6
prior irradiation of the mass
pregnancy (Sheehan syndrome)
trauma and surgery
anticoagulation therapy
changes in intracranial pressure
Clinical presentation
As the gland suddenly enlarges it may cause compression of structures adjacent to the sella, and thus elicit a number of signs and symptoms, including 7,8:
sudden headache, including of 'thunderclap' nature, often retro-orbital or between eyes
loss of visual acuity with a chiasmal field defect
oculomotor palsies
Also, the patient may experience a decreased level of consciousness, hypopituitarism, Addisonian crisis 3, and subarachnoid irritation, the latter being secondary to hemorrhage.
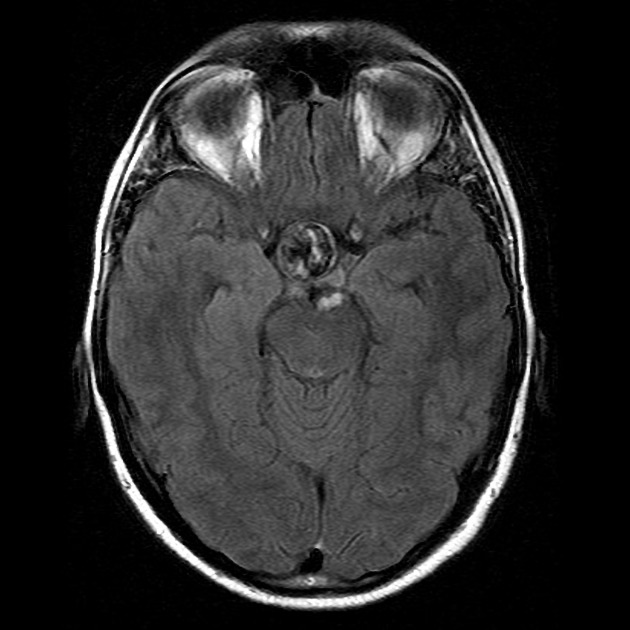
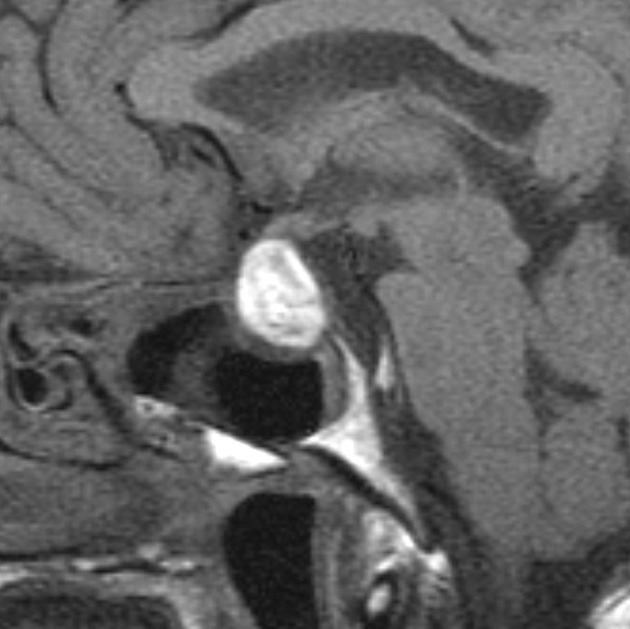
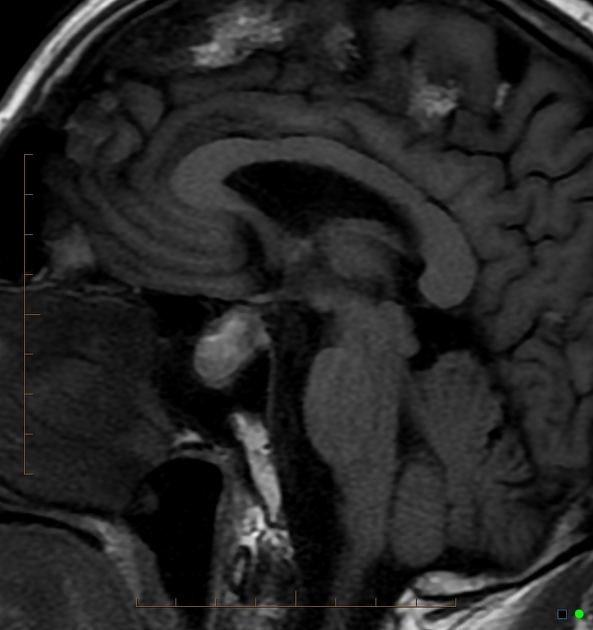
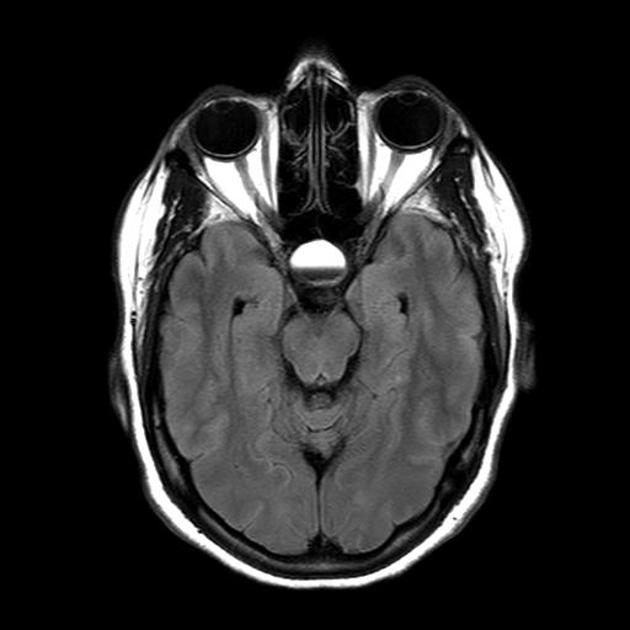
Radiographic features
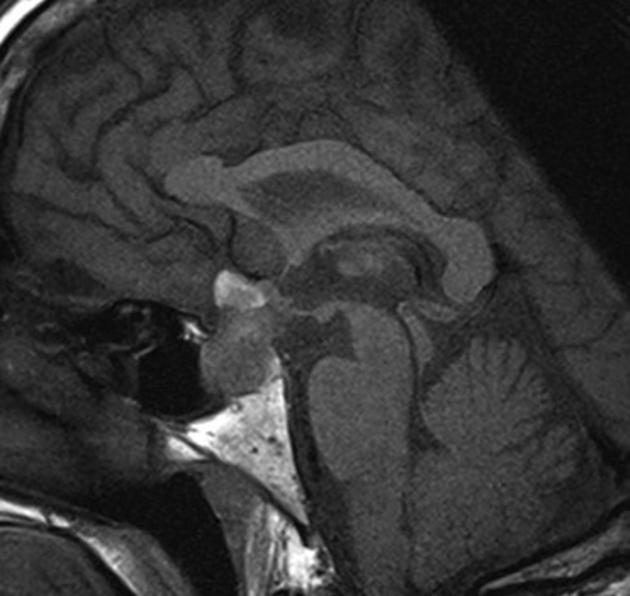
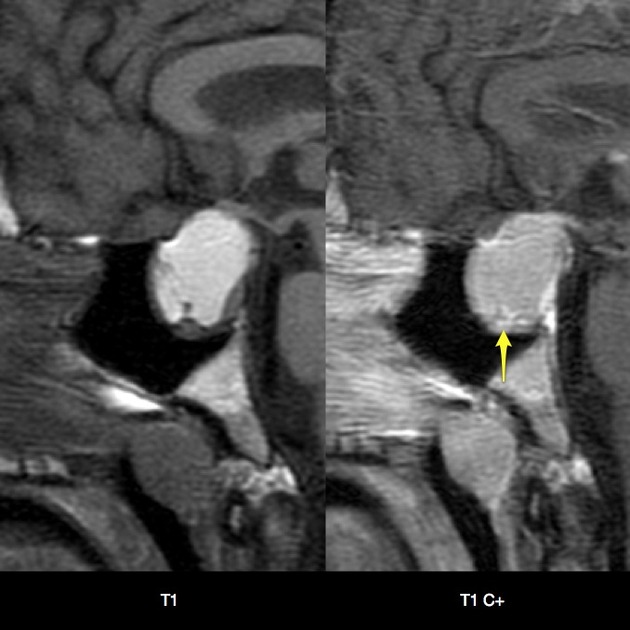
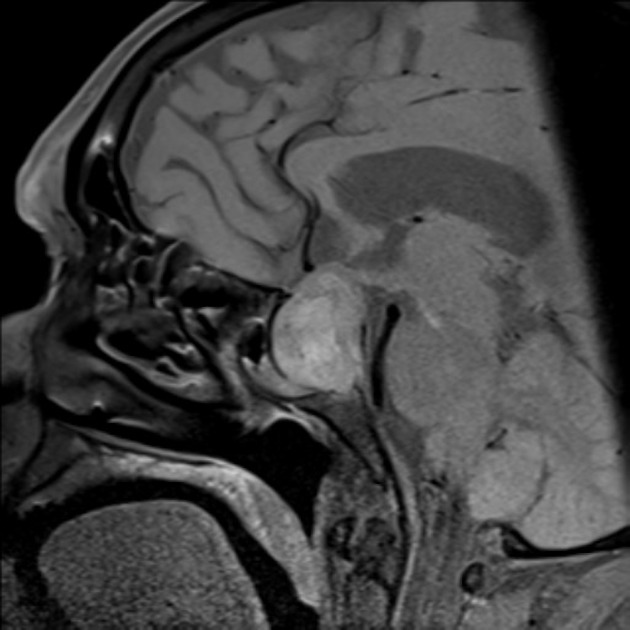
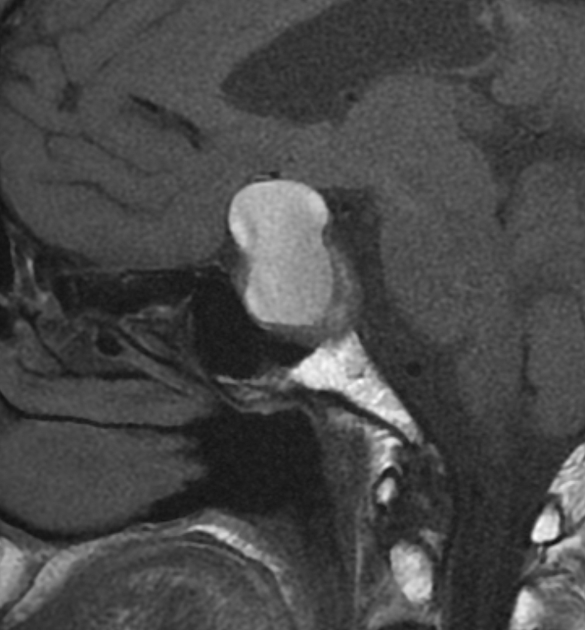
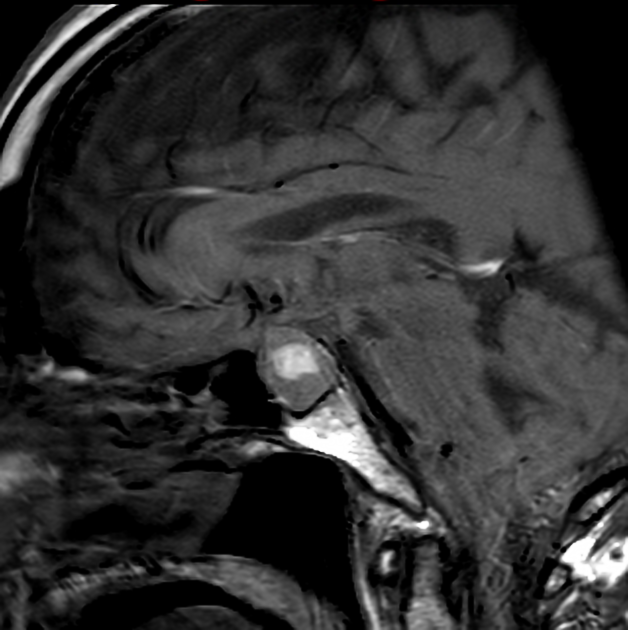
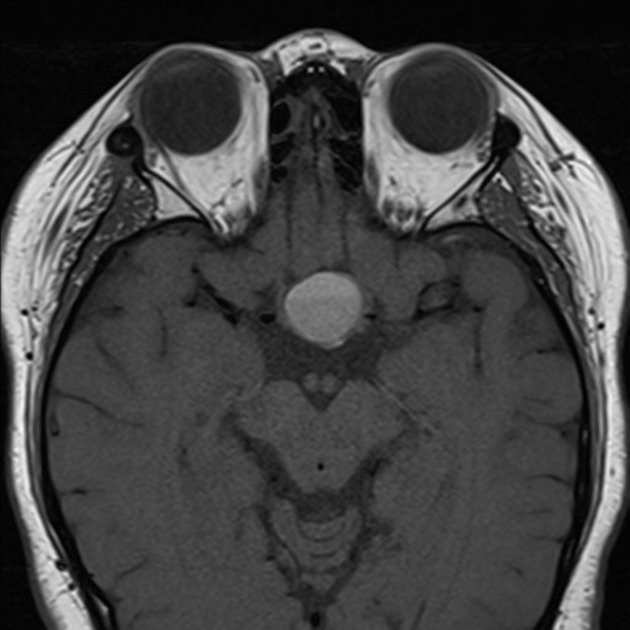
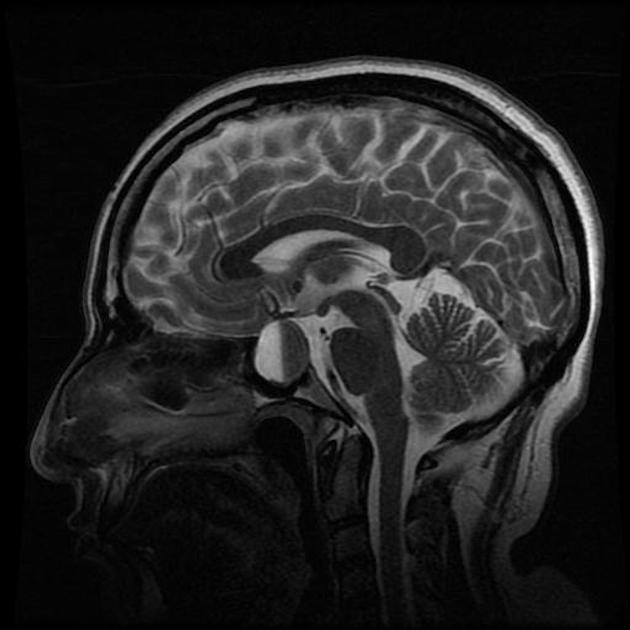
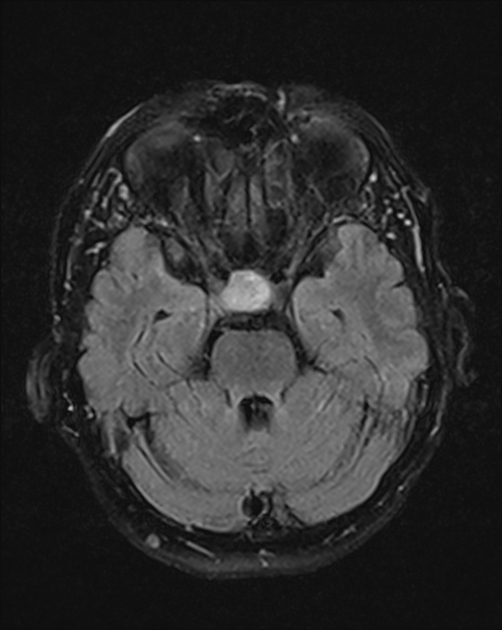
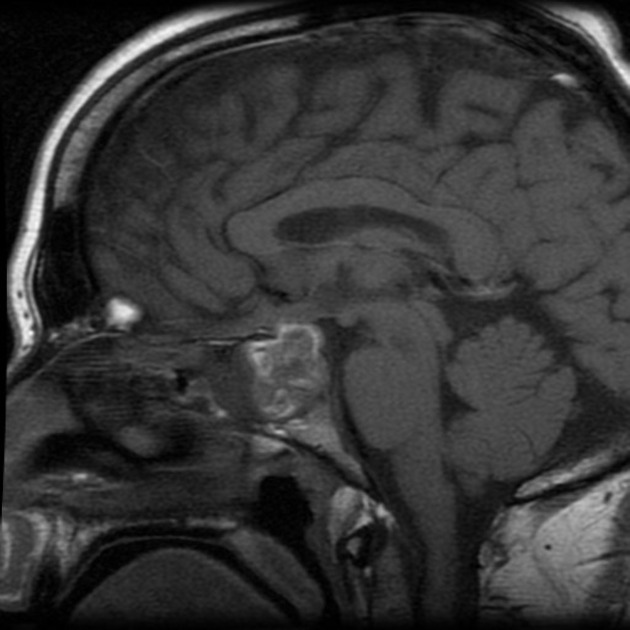
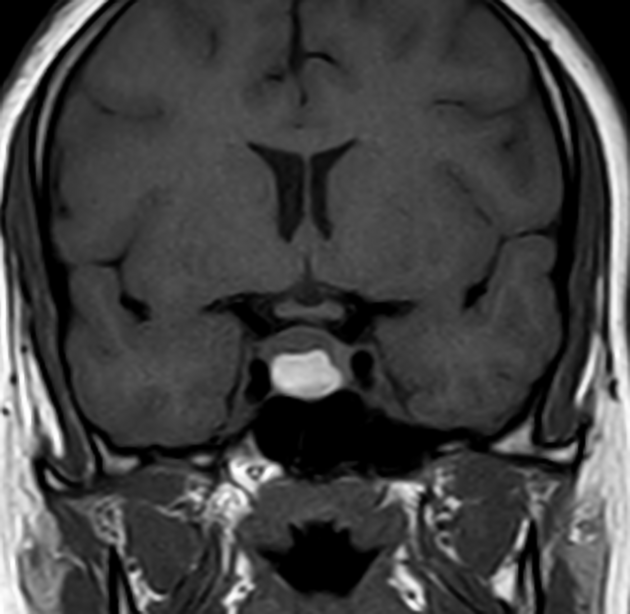
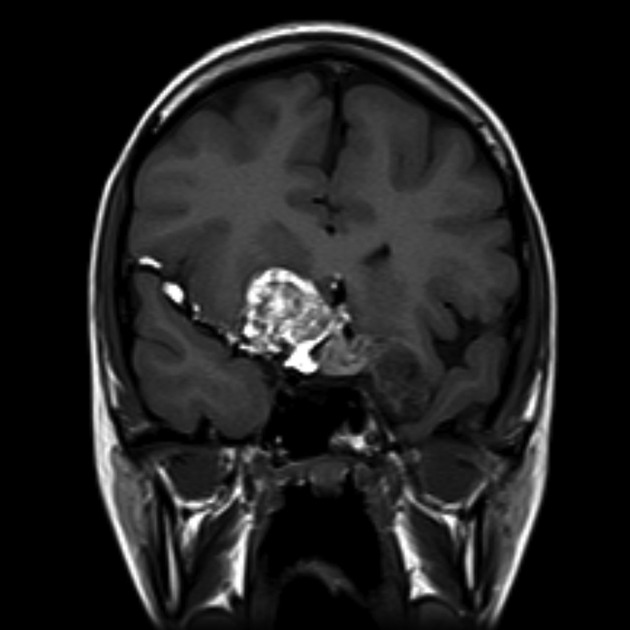
General features of pituitary apoplexy include enlargement of the pituitary gland, with or without bleeding. Macroscopic hemorrhage is common and occurs in about 85%. It shows peripheral enhancement around a non-enhancing infarcted center. Surrounding edema may be seen in the optic tracts and chiasm.
CT
Routine CT is insensitive to pituitary apoplexy unless frank intracranial hemorrhage is present. The pituitary mass may be evident and may be hyperdense. Fluid-debris levels may also be evident.
MRI
MRI typically demonstrates a pituitary region mass.
T1: variable; in cases with hemorrhagic infarction, it is hyperintense due to blood (see aging blood on MRI)
T2: variable signal
T1 C+ (Gd): enhancement variable; usually peripheral and may be difficult to identify due to intrinsic high T1 signal
DWI: restricted diffusion may be present in solid infarcted components 4
Treatment and prognosis
Immediate management includes prompt resuscitation, including administration of intravenous corticosteroids to avoid Addisonian crisis. Subsequent management is either neurosurgical or initially conservative 8. Generally, neurosurgical intervention is favored, with a transsphenoidal approach to decompress the pituitary gland, although a conservative approach may be considered in carefully selected patients without visual loss and with normal consciousness 8. Pituitary apoplexy is usually associated with irreversible hypopituitarism mandating long-term hormone replacement therapy 8, and often ophthalmoplegia and visual loss 5.
Follow-up
MRI is the preferred imaging method for follow-up. A follow-up MRI should be performed at 3 months to assess for a decrease in pituitary/macroadenoma size. Stability in size after several months may indicate an alternative diagnosis 9.
Differential diagnosis
The differential is broadly that of a pituitary region mass, but as these patients present acutely with acute or subacute blood products, it can usually be limited to pituitary region masses with intrinsic high T1 signal.
-
necrotic/hemorrhagic pituitary macroadenoma
appearances are the same, but patients do not present acutely
whether or not the term apoplexy can be used in subacute presentations is debatable
-
adamantinomatous craniopharyngioma
calcification in 90%
usually in children
usually not acute presentation
-
usually asymptomatic
no associated mass
spherical
-
usually have a fat component
unless ruptured, the presentation is usually insidious
if ruptured, locules of fat density/intensity material are often seen in the subarachnoid space






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.