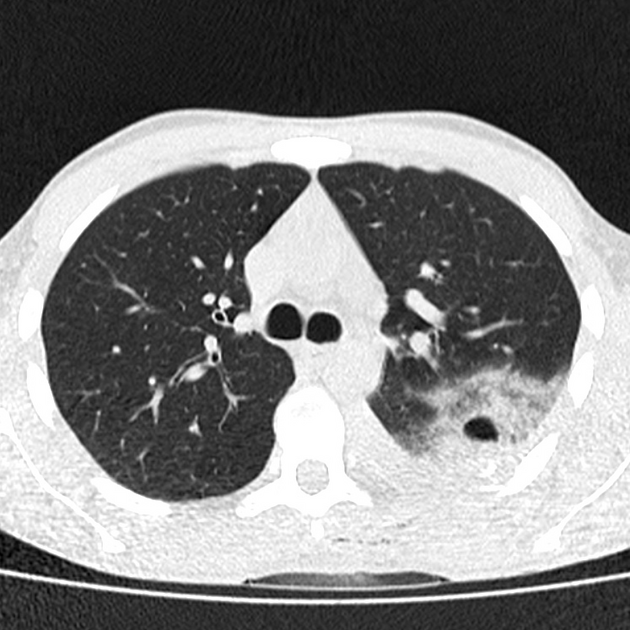
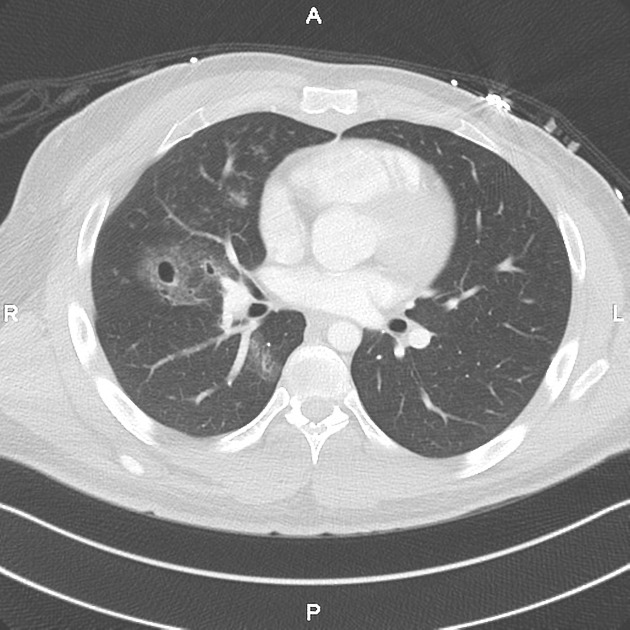
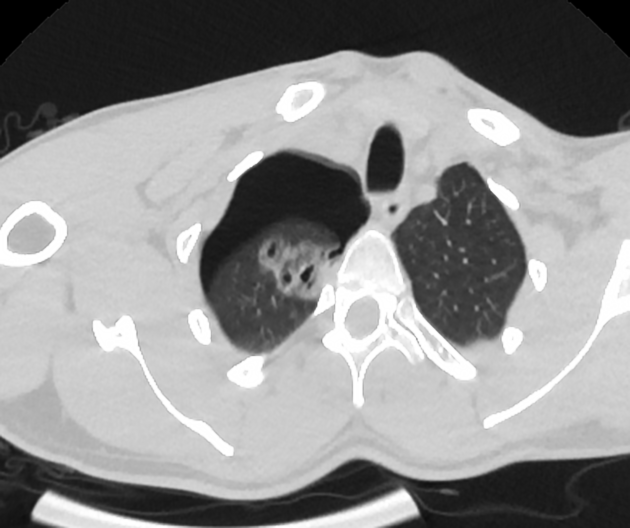
Pneumatoceles are intrapulmonary gas-filled cystic spaces that can have a variety of sizes and appearances. They usually occur as a result of pneumonia or in neonates as the result of a ventilator-induced lung injury. They should not be mistaken for a cavitating lung mass.
On this page:
Epidemiology
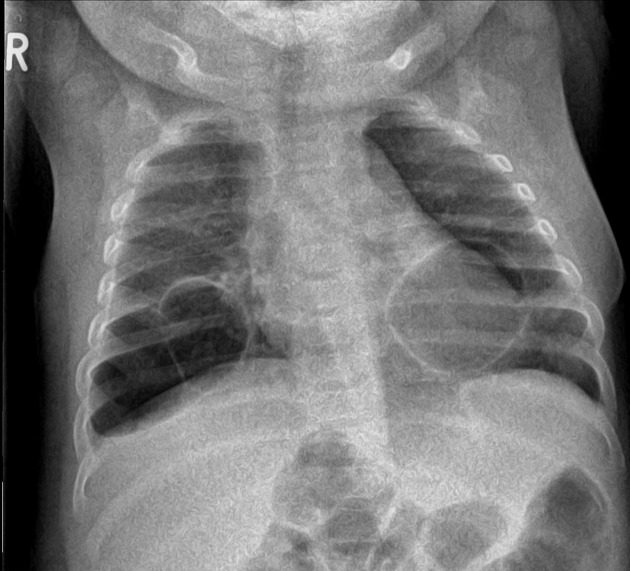
Although pneumatoceles are seen in all age groups, they are most frequently encountered in infancy 1.
Clinical presentation
Pneumatoceles are typically asymptomatic and remain visible if secondary to pneumonia after septic symptoms have resolved 1. Occasionally pneumatoceles become large enough to compress adjacent lung tissue and the mediastinum enough to cause respiratory or cardiovascular symptoms.
Secondary infection may occur resulting in features of chest sepsis.
Pathology
The majority of pneumatoceles occur as a result of pneumonia (post-infectious pneumatocele). The causative agents include:
Staphylococcus aureus (most common)
Streptococcus pneumoniae
Haemophilus influenza
Escherichia coli
group A streptococci
Klebsiella pneumoniae
adenovirus
COVID-19 (infrequent) 7,8
In addition to infection, pneumatoceles are also seen in several other settings, including:
trauma: traumatic pulmonary pseudocyst / traumatic pneumatocele (separate article)
positive pressure ventilation, especially in preterm neonates 4
Three main theories have been put forward to explain the formation of pneumatoceles 1:
pulmonary overinflation caused by transient bronchial/bronchiolar obstruction and a ball-valve effect
drainage of necrotic lung parenchyma with subsequent enlargement secondary to a ball-valve effect
focal collections of air within the pulmonary interstitium following inflammation and necrosis of the airway wall and fistula formation with the pleura
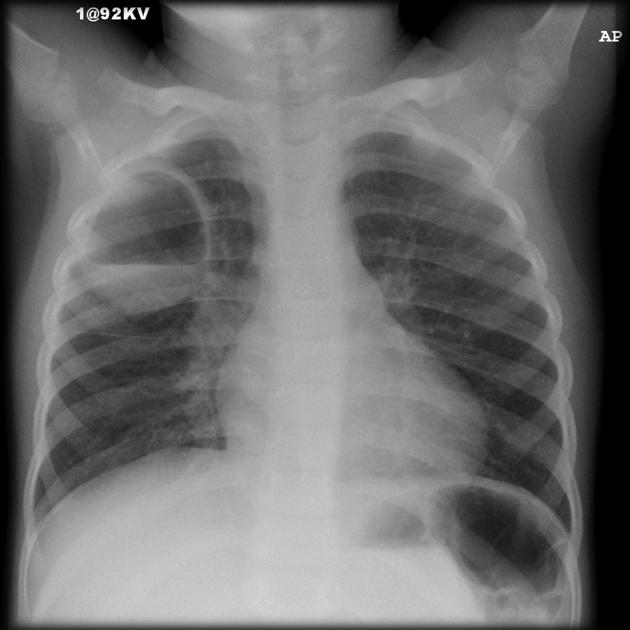
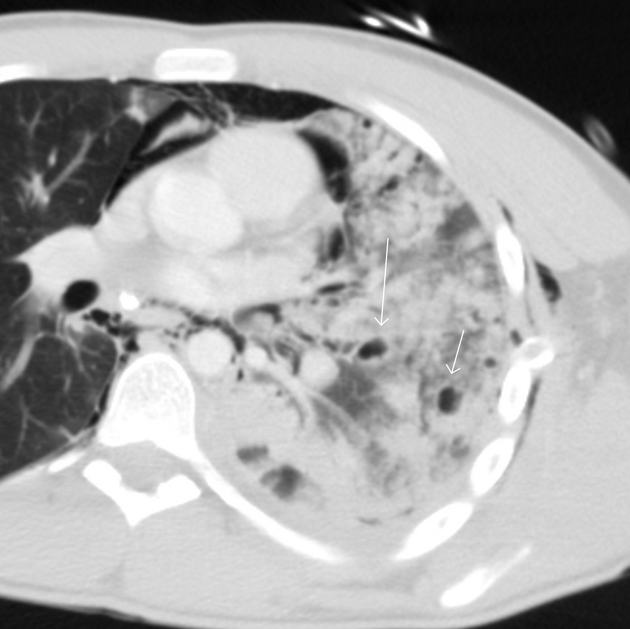
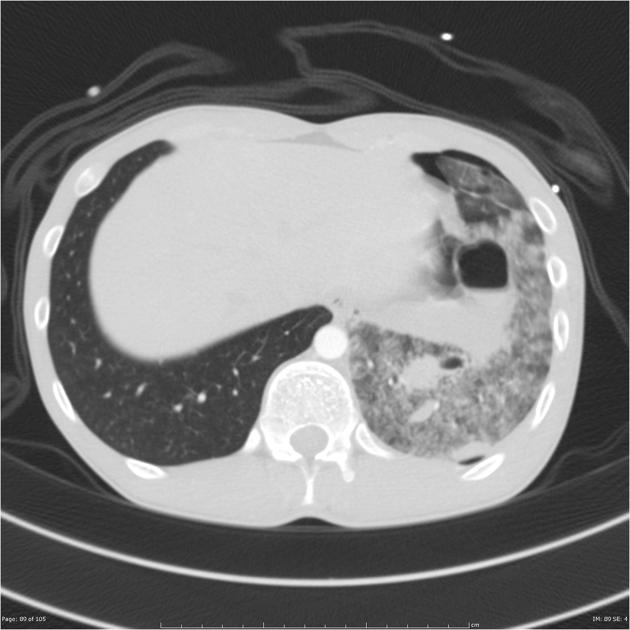
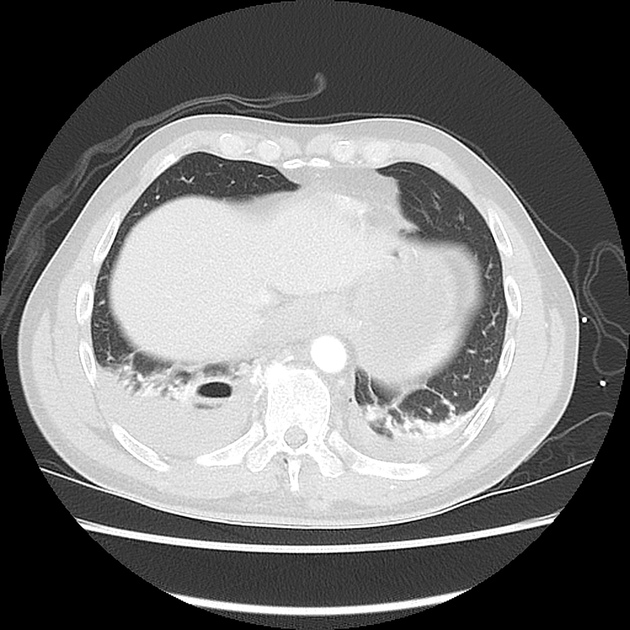
Radiographic features
When mature, pneumatoceles appear as thin-walled gas-containing cystic spaces within the lung parenchyma. However, it is important to remember that as they usually occur in the setting of infection, their appearance may vary, depending on the stage at which they are imaged.
They tend to appear within the first week of infection and have usually resolved by week six.
If they are imaged during formation, they may have surrounding consolidation and be difficult to distinguish from abscesses. Features that favor a pneumatocele over an abscess include 1:
smooth inner margins
little if any fluid content
the wall, if visible, is thin and regular
tend to persist despite an absence of symptoms
Treatment and prognosis
Post-infectious pneumatoceles tend to spontaneously resolve, providing that the infection is adequately treated with antibiotics. Surgical intervention is only required if the pneumatocele causes symptoms due to mass effect or if it ruptures into the pleural space resulting in a pneumothorax.
Complications
a rupture of a pneumatocele may cause a pneumothorax 3
secondary infection of the pneumatocele 5
Differential diagnosis
If thin-walled, consider the differential for a single lung cyst.
If thick-walled, the differential is generally that of cavitating lung masses and other air-containing lung lesions.
-
can be difficult to distinguish
thicker irregular walls
should resolve as symptoms resolve
infected pulmonary sequestration
In an older patient, the differential diagnosis for a cavitating lung lesion includes:





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.